All published articles of this journal are available on ScienceDirect.
Comparison of Endotracheal Intubation Through I-gel and Intubating Laryngeal Mask Airway
Abstract
Background:
Supraglottic airway devices (SADs) are very useful airway adjunct in managing anticipated and unanticipated difficult airway and can be used as a ventilating aid and as a conduit for tracheal intubation. The new versions of SADs like i-gel and intubating laryngeal mask airway (ILMA), have advantage of hands-free airway maintenance without the need for tracheal intubation, they can be placed easily without direct visualization of the larynx, ensure predictable ventilation and can be used as conduit for tracheal intubation.
Objective:
To compare ease and success of placement of both SADs and ease and success of endotracheal (ET) intubation through both SADs.
Method:
Eighty patients of both sexes, aged between 18-60 years and belonging to ASA grade I and II undergoing surgical procedure under general anaesthesia (GA) were randomly divided into two group (i-gel and ILMA) of equal number. Following induction the allocated device was inserted and after confirming adequate ventilation, blind ET intubation was attempted through the device. First attempt and overall success rate of SAD insertion and ET intubation through SAD; time taken for SAD insertion and ET intubation through SAD; hemodynamic changes and postoperative complications were recorded and compared between groups.
Result:
Demographic profile, success rate of SAD insertion, haemodynamic changes and adverse effects were similar between groups (p>0.05).Overall time needed for successful SAD insertion was significantly shorter in group i-gel (22.52±5.64 sec) than group ILMA (31.15±5.52 sec) (p value <0.0001). Overall success rate of blind ET intubation was higher in group i-gel (75%) in comparison to group ILMA (65%). I-gel required significantly less time to achieve successful ET intubation than ILMA (26.30±11.35 sec vs. 33.53±13.13 sec)(p<0.0001).
Conclusion:
Both the SADs were proved to be useful alternative to conventional laryngoscope for ET intubation, although i-gel required lesser time and had better success rate of ET intubation as compared to ILMA.
INTRODUCTION
The basic responsibility of an anaesthesiologist is to maintain adequate gas exchange in patients by securing a patent airway through face mask, supraglottic airway devices (SADs) or endotracheal (ET) intubation. Among these techniques patency of the airway is best ensured by an ET tube and direct laryngoscopy (DLS) is the gold standard method for placement of ET tube. However, training in ET intubation requires time, appropriate instruments, and adequate circumstances. Furthermore, ET intubation requires continued practice and carries with it its own set of complications. Technical problems with placement of ET tube have been the most frequent cause of anaesthetic deaths in published analysis from all over the world [1, 2].
SADs are novel devices that provide greater control of the airway than the face mask without the invasive disadvantages of the ET tube. They are helpful in managing anticipated and unanticipated difficult airway and can be used as a ventilating device and as a conduit for ET intubation. The advantage of SADs in comparison to DLS are easy to insert, less traumatic, less haemodynamic derangements, better view of glottic area using fiberoptic method etc [3]. The new version of SADs like i-gel® (Intersurgical, Wokingham, Berkshire, UK) and intubating laryngeal mask airway (ILMA) (LMA Fastrach™, LMA North America, San Diego, CA) allow easy placement with predictable ventilation, minimize the chances of pulmonary aspiration and serve as a conduit for ET intubation.
Present study aimed at comparing i-gel® and ILMA™, in relation to ease and success rate of blind ET intubation through them in anaesthetized, paralyzed adult patients with normal airway posted for surgery under general anaesthesia (GA) with respect to success rate of SAD insertion and ET intubation; time taken for SAD insertion and for ET intubation through SAD. Haemodynamic changes and postoperative complications were also compared.
MATERIALS AND METHODS
After getting approval from the institutional ethical committee and informed consent from the patients, the present prospective, randomized, controlled trial was conducted on 80 patients belonging to American Society of Anaesthesiologist (ASA) grade I-II, aged between 18-60 years, weighting 30-90 kg with mallampatti grade (MPG) I and II scheduled to undergo elective surgery under GA. Exclusion criteria exercised were emergency surgery, increased risk of aspiration, abnormal or distorted anatomy of the pharynx, obstruction of the airway beyond the larynx and decreased compliance of the lungs. During preoperative visit demographic data and detailed history was recorded; general physical and systemic examinations and routine investigations were carried out. All patients were kept fasting as per institutional protocol (2 h for clear liquid and 6 h for semisolid and solid).
Out of 173 patients screened 80 patients fulfilling the inclusion and exclusion criterion were randomly allocated by a computer generated random table to one of the two groups either i-gel group (n=40) or ILMA group (n=40) (Fig. 1). Selected patients were shifted to the operation room (OR). Intravenous (IV) line was secured with 18G IV cannula. All patients received premedication with ranitidine 50 mg and metoclopramide 10 mg IV 30 minutes before induction. ASA standard monitor e.g. electrocardiograph (ECG), Noninvasive blood pressure (NIBP) and Arterial oxygen saturation (SpO2) were attached and all patients received IV glycopyrrolate 0.2mg, IV fentanyl 2mcg /kg and IV midazolam 0.03 mg/kg, 10 minutes before induction of anaesthesia. After preoxygenation with 100% oxygen for 3 minutes induction was done with propofol 2.5 mg/kg. After assessing adequate mask ventilation, muscle relaxation was facilitated with atracurium 0.5 mg/kg, mask ventilation was continued for 3 minutes. Then according to allocated group proper size SAD and ET tube (LMA Fastrach™ ETT) were selected according to weight (Table 1). The standard pre use tests for both devices were performed prior to insertion. Both devices were lubricated using 2% lignocaine jelly and the ILMA™ was fully deflated prior to insertion. ILMA™ was inserted in neutral neck position while i-gel® was inserted in extended neck position. If insertion of SAD was unsuccessful at first attempt, second attempt was done using recommended maneuvers (Brain et al. [4]; Gatward et al. [5] for ILMA™ and i-gel® respectively) and if unsuccessful, third attempt was done using larger size SADs. After SAD insertion, confirmation of successful ventilation was determined by chest wall movement, auscultation of breath sounds and continuous waveform capnography. The numbers of attempt required for SAD insertion were recorded. A failed attempt was defined as removal of the SAD from the mouth before reinsertion. If successful ventilation couldn’t be achieved even after third attempt this was recorded as failure of SAD insertion. Duration of SAD insertion was defined as the time taken from removal of face mask till the confirmation of successful ventilation. The time was measured with the help of a stopwatch. After achieving successful ventilation with SAD, blind ET intubation was attempted using LMA Fastrach™ ETT through both devices. If no resistance was felt ET tube was advanced fully into the SAD. When resistance was felt during ET tube insertion, following maneuvers were tried in i-gel group: 1) Twisting of the ET tube to align the bevel, up and downward movement of the ET tube gently within the SAD. 2) Application of cricoid pressure (Bhandari G et al. [6]). If resistance was felt during insertion of ET tube in ILMA group, a standardized algorithm [4] was followed on the basis of the distance at which the resistance was felt and other maneuvers were used including: optimizing the airway, rotating the ET tube bevel, adjusting head neck position and adding air to the cuff. If ET intubation was unsuccessful at first attempt even after using maneuvers, second attempt was done with smaller size ET tube and if unsuccessful third attempt was done using maneuvers with small size ET tube. In both the groups, maximum three attempts were allowed for SAD insertion and ET intubation. If ET intubation through the device was unsuccessful, it was performed using DLS. Duration of successful ET intubation through SAD was defined as the time elapsed from passing the ET tube through SAD until confirmation of successful ventilation, which was determined by chest rise, auscultation of breath sounds and waveform capnography. In all patients, procedure was performed by the same anaesthesiologist having experience in using both types of SADs.
Showing selection of SAD and ETT based on the weight of the patients.
| SAD | Body Weight (kg) | SAD Size | ET Tube Size |
|---|---|---|---|
| i-gel | 30-50 | 3.0 | 7.0 |
| 50-70 | 4.0 | 7.5 | |
| >70 | 5.0 | 7.5 | |
| ILMA | 30-50 | 3.0 | 7.0 |
| 50-70 | 4.0 | 7.5 | |
| >70 | 5.0 | 7.5 |
Anaesthesia was maintained with sevoflurane (2 vol%) in oxygen/nitrous oxide (40%/60%) mixture. Intermittent bolus of atracurium for muscle relaxation and fentanyl for analgesia was used. Patients were ventilated using volume control mode with tidal volume of 8 ml/kg. At the end of surgery, neuromuscular blockade was reversed with a mixture of glycopyrrolate (0.01 mg/kg) and neostigmine (0.05 mg/kg) and extubation was done after recovery of adequate muscle power, consciousness and spontaneous respiration. Complications like lip trauma, dental injury and blood mixed secretions over SAD and ET tube at the time of its removal were observed and recorded. In post-operative period, at two hours, an investigator asked the patients about throat pain, dysphonia, dysphagia and hoarseness which were assessed as present or absent.
Sample size was calculated by conducting a pilot study. We find a difference of 10.6 s in the mean time to ET intubations through i-gel and ILMA with a standard deviation of 13.58. A minimum of 39 patients in each group were required to reject a null hypothesis of no difference in mean time to ET intubations between the 2 groups with 80% power. The type-I error (α- error) probability associated with this 2-sided test of this null hypothesis was 0.05. Data were analyzed using SPSS (IBM SPSS statistics for windows, version 20.0. Armonk, NY: IBM Corp).The qualitative data were compared using Chi Square test and for comparison of the continuous variable independent t-test was used. p value <0.05 was considered statistically significant.
RESULTS
Both the groups were comparable regarding demographic profile (Table 2). Comparison of baseline and intraoperative vitals (mean HR, MAP and SpO2) at various time intervals didn’t show any significant difference between the groups (p value >0.05) (Table 3).
Demographic profile of the patients in both the groups.
| Demographic Parameter | Group i-gel (n=40) | Group ILMA (n=40) | p-value |
|---|---|---|---|
| Age (yrs) Mean±SD | 38.65±11.67 | 42.00±11.12 | 0.14 |
| Sex (M/F) | 14/26 | 22/18 | - |
| ASA (I/II) | 27/13 | 28/12 | - |
| Weight (Kg) Mean±SD | 61.68±7.92 | 62.78±8.12 | 0.54 |
| MPG (I/II) | 22/18 | 25/15 | - |
SAD insertion first attempt success rate was 90% and overall success rate was 100% in both groups. Mean±SD insertion time at successful first attempt was 21.0±3.30 sec for group i-gel and 26.69±2.89 sec for group ILMA, and the difference was statistically significant (p value <0.0001). The overall insertion time was significantly higher for group ILMA (31.15±5.52 sec) than for group i- gel (22.52±5.64 sec) (p value <0.0001) (Table 4).
Success rate of ET intubation through SAD at first attempt and overall was 57.5% and 75% respectively for group i-gel and 52.5% and 65%respectively for group ILMA. Mean±SD ET intubation time at successful first attempt was 20.95±3.61sec for group i-gel and 27.85±3.11sec for group ILMA, and the difference was statistically significant (p value <0.0001). The overall ET intubation time was significantly higher for group ILMA (33.53±13.13sec) than for group i-gel (26.30±11.35) (p value <0.0001) (Table 4).
Comparison of baseline and intraoperative vitals (HR, MAP and SpO2) between the groups.
| TIME | Group i-gel (Mean±SD) | Group ILMA (Mean±SD) | ||||
|---|---|---|---|---|---|---|
| HR (bpm) | MAP (mmHg) | SpO2 (%) | HR (bpm) | MAP (mmHg) | SpO2 (%) | |
| Baseline | 81.57±11.89 | 92.52±8.86 | 98.87±0.70 | 76.77±10.85 | 94.57±6.55 | 98.77±0.86 |
| After SAD insertion | 81.57±11.87 | 92.55±9.14 | 100±0.00 | 78.10±11.59 | 94.80±6.81 | 100±0.00 |
| After ET intubation | 83.22±12.17 | 93.55±8.90 | 100±0.00 | 79.47±11.79 | 97.05±8.34 | 100±0.00 |
| At 1 min | 83.80±11.80 | 95.45±8.70 | 100±0.00 | 79.20±12.36 | 98.02±8.31 | 100±0.00 |
| At 3 min | 83.15±11.90 | 94.10±8.98 | 100±0.00 | 79.47±11.80 | 96.72±7.24 | 100±0.00 |
| At 5 min | 81.45±11.03 | 93.25±8.63 | 100±0.00 | 77.87±11.44 | 95.57±6.13 | 100±0.00 |
Success rate Time required for SAD insertion and ET intubation in both groups.
| Group i-gel | Group ILMA | p value | ||
|---|---|---|---|---|
| SAD Insertion Success Rate [n(%)] | 1st Attempt | 36 (90%) | 36 (90%) | - |
| 2nd Attempt | 04 (10%) | 04 (10%) | - | |
| 3rd Attempt | 00 (00%) | 00 (00%) | - | |
| Overall | 100% | 100% | - | |
| SAD Insertion Time (Mean±SD) | Successful 1st Attempt | 21.0±3.30 | 26.69±2.89 | <0.0001 |
| Overall | 22.52±5.64 | 31.15±5.52 | <0.0001 | |
| ET Intubation Success Rate [n(%)] | 1st Attempt | 23 (57.5%) | 21 (52.5%) | - |
| 2nd Attempt | 05 (12.5%) | 04 (10%) | - | |
| 3rd Attempt | 02 (5%) | 01 (2.5%) | - | |
| Overall | 30 (75%) | 26 (65%) | - | |
| Et Intubation Time (Mean±SD) | Successful 1st Attempt | 20.95±3.61 | 27.85±3.11 | <0.0001 |
| Overall | 26.30±11.35 | 33.53±13.13 | <0.0001 | |
Both the groups were comparable regarding complications. None of patient complained of lip trauma, dental injury, dysphonia, dysphagia and hoarseness in both groups. 17.5% in group i-gel and 20% in group ILMA complained throat pain (Table 5).
Comparison of postoperative complication between the groups.
| Complication |
Group i-gel n (%) |
Group ILMA n (%) |
|---|---|---|
| Throat pain | 07(17.5%) | 08(20%) |
| Dysphonia | 00 | 00 |
| Dysphagia | 00 | 00 |
| Hoarseness | 00 | 00 |
DISCUSSION
ET intubation by Macintosh laryngoscope is the gold standard method for securing airway and for providing oxygenation and ventilation but it leads to undesirable haemodynamic stress response due to stimulation of oropharyngeal structures. The haemodynamic stress response can precipitate adverse cardiovascular events in patients with and without cardiovascular diseases. The laryngeal mask airway (LMA; LMA North America, San Diego, CA) was one of the first SAD invented by Dr. Archie Brain in 1981 [7], since then a large number of different types of SADs have come into the anaesthetic practice. These devices circumvent many of problems associated with laryngoscopy and intubation. They are helpful in managing anticipated and unanticipated difficult airway and can be used as a ventilating device and as a conduit for tracheal intubation.
ILMATM offers a new approach for ET intubation. It eliminates need for anatomical distortion of oropharyngeal structures and manipulation of head and neck and thus increases its utility in the patients with cervical spine pathology [8]. The i-gel®) is a relatively new SAD anatomically designed to conform the hypopharynx without using an inflatable cuff. The mask surface is made of a gel-like thermoplastic elastomer, which is soft and conforms to the larynx. A second lumen runs along the entire length of the device to the distal tip to accommodate a nasogastric tube for drainage of potential regurgitant gastric contents [9, 10]. The use of these SADs as a conduit for ET intubation has been documented in several studies and case reports [4, 6, 11-17].
The present study was conducted to evaluate ease and success of ET intubation through i-gel® and ILMA™ in patients with normal airway. Both the groups (i-gel and ILMA) in our study had similar demographic profile that helped us to alleviate a point of controversy regarding selection of SAD. The present study demonstrated 100% overall success rate of SAD insertion for i-gel® and ILMA™. However, first attempt success rate of SAD insertion was 90% in both groups and rest of the patients required second attempt with adjustment (Neck extension or flexion, Chin-lift, Jaw-thrust and gentle pushing and pulling of the device) for i-gel® and (in situ manipulation) for ILMA™. The number of airway manipulations required to establish the airway were not recorded. Third attempt was not required in any of the patients in both the groups. ILMA™ required significantly more time (at first attempt and overall) for successful SAD insertion than i-gel® (p<0.0001) (Table 4). These results were similar to a study conducted by Bhandari G et al. [18] They found higher first attempt success rate in group i-gel than group ILMA (95% vs. 90%) and similar overall success rate in both groups (100%). In their study i-gel® required significantly lesser time compared to ILMA™ (20.52±1.44 sec vs. 30.69±1.73 sec) at successful first attempt (p value <0.0001) and overall insertion time (20.92±2.25 sec vs. 31.75±3.62 sec) (p value <0.0001). Halwagi AE et al. [19] found higher first attempt success rate in group i-gel than group ILMA (84% vs. 80%) but lower overall success rate in group i-gel than group ILMA (96% vs. 100%). In their study time required for SAD insertion when first attempt was successful in group i-gel and group ILMA were 26±24 sec and 36±28 sec respectively(p value =0.03). Similarly i-gel® required significantly lesser overall insertion time compared to ILMA™ (19±8 sec vs. 29±16 sec)(p value <0.0001).The easier and quicker insertion of i-gel® as found in our study was probably due to non-inflatable cuff and moreover, the rigid structure of ILMA™ causes delay in insertion as compared to i- gel®.
The present study demonstrated that i-gel® and ILMA™ are effective aids for blind ET intubation. The first attempt and overall success rate of ET intubation through SAD was higher in group i-gel than group ILMA (57.5% vs. 52.5%) and (75% vs. 65%) respectively (Table 4). Similar results were found in a study conducted by Bhandari G et al. [18], in their study they found that first attempt and overall success rate of ET intubation through SAD was higher in group i-gel than in group ILMA (62.5% vs. 52.5%) and (77.5% vs. 65%) respectively. In contrast Halwagi AE et al. [19] found higher first attempt and overall success rate of ET intubation in group ILMA than group i-gel (69% vs. 74%) and (91% vs. 73%) respectively. More number of patients in each group, use of conventional PVC ET tube and different insertion technique of ET tube (with a reverse orientation in group ILMA and posteriorly pointed bevel in group i-gel) could have resulted in higher success rate with ILMA™. Michalek et al. [20] also found that success rate of blind ET intubation through i-gel® was less compared to ILMA™ (51% vs. 88% respectively), as they used conventional PVC ET tube with i-gel® and soft tip, wire reinforced ET tube with ILMA™.
In the present study, time required for ET intubation (at first attempt and overall) was significantly shorter in group i-gel than group ILMA (20.95±3.61 sec vs. 27.85±3.11 sec) and (26.30±3.61 sec vs. 33.53±13.13 sec) respectively (p value <0.0001). Similarly Bhandari G et al. [18] found that ET intubation time (at first attempt and overall) was significantly lesser in group i-gel than group ILMA (18.73±1.41 sec vs. 29.63 ±1.39 sec) and (20.41±3.79 sec vs. 30.68 ±3.197 sec) respectively (p value <0.0001). Halwagi AE et al. [19] found that overall ET intubation time in group i-gel was significantly lesser than group ILMA (22±13 sec vs. 30±31 sec) (p value =0.04). However, ET intubation time when first attempt was successful in group i-gel and group ILMA were comparable (19±4 sec vs. 18±3 sec) (p value =0.37).
There was a similar hemodynamic response (increased HR and MAP) to SAD insertion and ET intubation through SAD in both groups. HR and MAP return to baseline at 5 minute in both the groups. Similar haemodynamic response in both the groups can be attributed to comparable sympatho-adrenal stimulation in response to both SADs. Kavitha J et al. [21] in their study found nonsignificant rise in HR and MAP after ILMA insertion and after ET intubation through ILMA, followed by return to baseline at 5 min Both the devices are equally effective in maintaining SpO2 as there was no episode of desaturation in both the groups .
There was no incidence of lip trauma, dental trauma and blood tinged secretions over the SAD or ETT in any of the patient in both the groups. None of the patient in both the groups complained of dysphonia, dysphagia and hoarseness while 7 (17.5%) patient in group i-gel and 8 (20%) patient in group ILMA complained of throat pain in postoperative period. Gel filled cuff in i-gel causing less trauma or pressure damage to the oropharyngeal mucosa explain lesser number of patient with throat pain in group i-gel.
Hence, we conclude that both the SADs i.e. i-gel® and ILMA™ are useful alternative to conventional laryngoscopy for ET intubation, both can maintain the airway and oxygenation of the patient without significant adverse haemodynamic changes. i-gel® is better in terms of success rate and time required for ET intubation as compared to ILMA™.
Limitation
As this was not a blinded trial, risks of biases including reporting and diagnostic bias were possible. The etiology of unsuccessful intubation was not assessed systematically. Such information would help many readers to interpret the findings correctly.
Implication
Our study is able to demonstrate that the use of i-gel® and ILMA™ could be an alternative to direct laryngoscopy for endotracheal intubation in patient with normal airway. Use of fiberoptic for intubation could improve the success rate of ET intubation through these devices. However, there is need for further RCT with proper sample size to replicate the findings of our study. So that both the SADs can become standard of care for securing the airway in patients with normal airway.
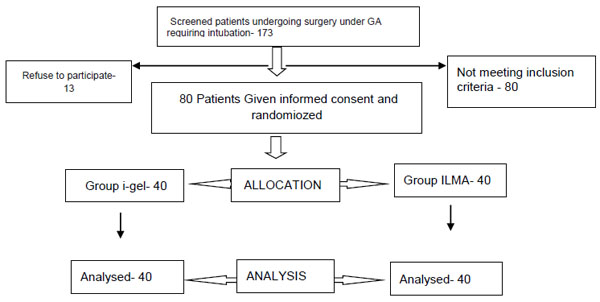
Study flow chart.
CONCLUSION
Both the SADs i.e. i-gel and ILMA were proved to be useful alternative to conventional laryngoscope for tracheal intubation, although i-gel had better success rate in tracheal intubation and less time required as compared to ILMA.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


