All published articles of this journal are available on ScienceDirect.
Clinical Early Warning Scores: New Clinical Tools in Evolution
Abstract
Clinical Early Warning Scores are tools intended to alert clinical staff to possible future clinical deterioration, often related to the onset of sepsis. Since their introduction, they have increased greatly in popularity. Their operation is conceptually simple: an elevated early warning score triggers a formal assessment by the responsible clinician. While the best-known system is the Royal College of Physicians National Early Warning Score (NEWS), a number of other scores are in use, such as an adaptation known as the Modified Early Warning System (MEWS) or warning systems for pediatric patients (PEWS). However, while promising, such instruments need to be studied in more detail to better characterize their eventual role in monitoring hospital patients. In particular, a central question concerns the identification of the best system (NEWS, MEWS, PEWS etc.) for a given clinical population (pediatric, trauma, prehospital etc.).
1. INTRODUCTION
Early Warning Scores are clinical instruments designed to alert medical staff to impending clinical deterioration. This deterioration is often but not exclusively in relation to the onset of sepsis. Since their introduction about a decade ago, they have increased greatly in popularity. The application of Early Warning Systems is simple: an elevated early warning score triggers a formal assessment by a caregiver; sometimes the warning is even delivered automatically via a page or SMS sent to the responsible clinician. Although the best-known system is the Royal College of Physicians National Early Warning Score (NEWS) [1], a number of others are available for special situations, such as for pediatric patients.
2. THE NEWS SYSTEM
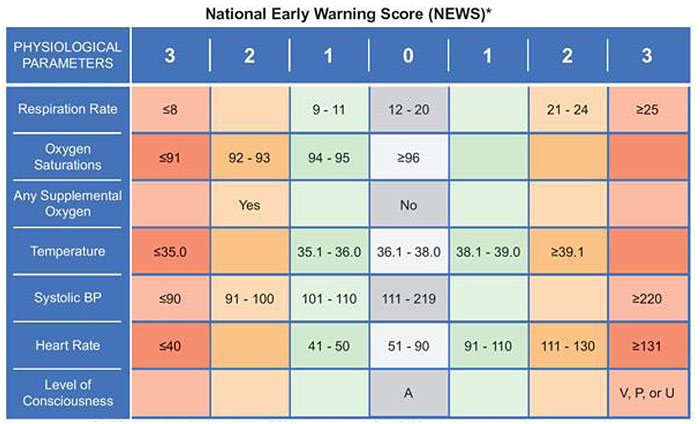
Fig. (1) illustrates the NEWS system, the best known clinical early warning scheme. It is based on seven clinical parameters (6 vital signs as well as the AVPU scale (“alert, voice, pain, unresponsive”) and produces an aggregate score between 0 and 20. Patients are considered to be at “low risk” with aggregate scores of 4 and under, at “medium risk” with aggregate NEWS scores of 5 or 6 or if an individual parameter scores at 3. A patient with a NEWS score of 7 or more is said to be at “high risk” and merits continuous vital sign monitoring as well as possible transfer to an acute care unit / high dependency unit or Intensive Care Unit (ICU). Finally, note that NEWS scores well under 7 can still be predictive of clinical trouble. For example, Kellett and Murray (2014) [2] noted that “patients admitted with a score of 0-2 who raise their score to >=3 have a ten-fold increase in-hospital mortality.”
The definitions used in the NEWS are as follows:
- Alert: The patient is fully awake, but not necessarily fully oriented), will spontaneously open his or her eyes, will respond to voice, and will have intact motor function.
- Voice: The patient makes some kind of response (via eyes, voice or movement) when you talk to them, although the response could be as little as a moan, or slight limb movement.
- Pain: The patient makes a response (again, via eyes, voice or movement) following the application of a noxious stimulus, such as sternal rub.
- Unresponsive: The patient provides no eye, voice or motor response to either voice or pain. Note also that a new onset of confusion merits clinical evaluation even if it is not formally part of the NEWS system [3].
In one of the early NEWS studies, Groarke et al. [4] followed 225 consecutive hospital medical admissions, and divided patients into four categories based on their NEWS score. Primary endpoints were length of hospital stay, Intensive Care Unit (ICU) / Coronary Care Unit (CCU) admission, death, and cardiac arrest. Higher admission scores were found to be correlated with the last three endpoints independent of patient age. They also found that a score improvement within 4 h of presentation to hospital predicted an improved outcome.
Alam et al. [5] collected data for 274 patients on arrival at the Emergency Department (ED) as well as one hour after arrival and at transfer to the general ward or ICU. In this study, the authors found that the NEWS score “was significantly correlated with patient outcomes, including 30-day mortality, hospital admission, and length of stay at all-time points.” The authors concluded that the system was of value to “longitudinally monitor patients throughout their stay in the ED and in the hospital.”
The applicability of the NEWS score to the prehospital setting has also been studied. For example, a study by Silcock et al. [6] examined the performance of the NEWS system in the prehospital setting with respect to primary endpoints of 48-hour and 30-day mortality, Intensive Care Unit (ICU) admission; all were associated with higher NEWS scores. The authors concluded that “elevated NEWS among unselected prehospital patients is associated with a higher incidence of adverse outcomes” and that use of the NEWS in the prehospital setting “may facilitate earlier recognition of deteriorating patients” while encouraging earlier involvement of senior staff.
While the above studies and a number of others are encouraging, some cautionary notes are worth mentioning. For example, Kolic et al. [7] studied whether NEWS compliance for identifying patient deterioration might vary out of hours. In a sample of 370 patients, the authors found that in 18.9% of patients the score was calculated incorrectly. Of special interest to administrators planning for weekend staffing, the authors found that the clinical response to deteriorating NEWS scores was “significantly worse at weekends”, with patients admitted on the weekend being “more likely to receive an inadequate response.” This study raises an important safety concern about weekend clinical staffing that hopefully will lead to further studies to help establish optimal off-hour staffing models.
Another example: NEWS escalates care to a doctor with scores over 4 or when the score for any single parameter is 3. However, not everyone agrees that this is reasonable. In a workload study by Jarvis et al. [8] the authors compared the clinical workloads generated by this escalation protocol and found that aggregate NEWS values are more important than high single parameter scores for predicting adverse outcomes, noting that “escalating care to a doctor when any single component of NEWS scores 3 compared to when aggregate NEWS values ≥5, would have increased doctors' workload by 40% with only a small increase in detected adverse outcomes from 2.99 to 3.08 per day (a 3% improvement in detection).” The authors also cautioned that such an escalation policy risks distorting the patient safety focus and additionally risks generating alarm fatigue.
As the NEWS system gained popularity, a number of disparate studies involving the original NEWS system as well as various adaptations were conducted to assess its performance. We briefly discuss this issue next.
3. MODIFIED EARLY WARNING SYSTEM
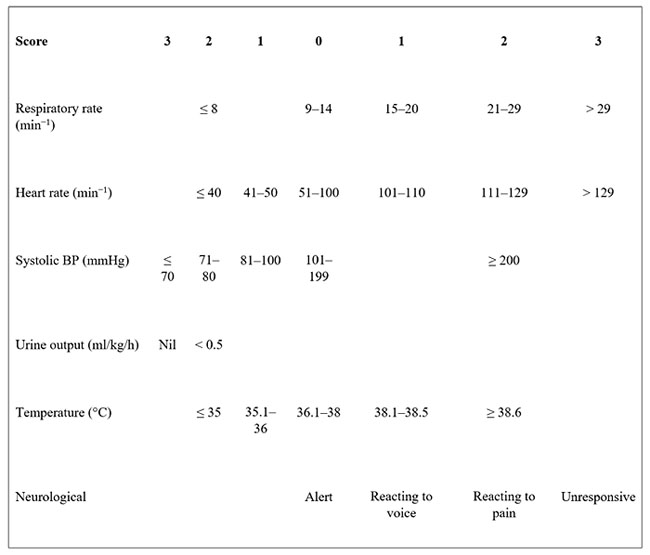
The Modified Early Warning System (MEWS) (Fig. 2), a modification of the NEWS, adds urine output as a clinical parameter but removes oxygenation parameters from the mix [9]. In a study of 334 patients the authors found that with a threshold of four or more as a trigger for action the system was 75% sensitive and 83% specific for predicting which patients required transfer to a higher level of care. Fig. (3) summarizes their approach.
Peris et al. [10] described the use of the Modified Early Warning Score may help anesthesia providers select the appropriate level of postoperative care in patients undergoing emergency abdominal surgery. In the study emergency surgical patients admitted before the introduction of MEWS in their hospital served as the control group (N= 604 patients), while emergency surgical patients admitted after the introduction of MEWS served as the experimental group (N= 478 patients). In this latter group patients with a MEWS of 3 or 4 were transferred to the hospital’s High Dependency Unit (HDU) while patients with a MEWS score of 5 or more were considered for ICU admission. The authors found that after the introduction of the MEWS system, HDU admissions increased from 14% to 21% while ICU admissions decreased from 11% to 5 without any deterioration in patient mortality. The authors concluded that the MEWS system “may help in reducing ICU admissions after emergency surgery.”
Suppiah et al. [11] studied the use of MEWS as a physiological prognostic indicator in patients with acute pancreatitis. A special feature of this study is that sensitivity, specificity, Negative Predictive Value (NPV), and Positive Predictive Values (PPV) as well as Receiver Operator Curves were calculated based on a cohort of 142 patients. The authors found that on hospital admission, sensitivity, specificity, NPV, PPV, and accuracy of diagnosing severe acute pancreatitis based on the highest MEWS score of 3 or more was 95.5%, 90.8%, 99.0%, 65.6% and 92.0% respectively. The authors concluded that “MEWS provides a novel, easy, instant, repeatable, reliable prognostic score that may be superior to existing scoring systems” but cautioned that a larger sample size would be required to validate their findings.

Fullerton et al. [12] retrospectively compared the MEWS score against clinician judgement in detecting critical illness in the pre-hospital environment. Their study was based on a cohort of 3504 adult emergency department admissions over a two-month period where the outcome of interest was the whether an adverse event occurred in the 24-hour period following admission. The authors found that clinical judgment alone had a low sensitivity for predicting critical illness in the pre-hospital environment but that the addition of the MEWS score as an adjunct to clinical judgment improved the prediction of future adverse events, although unfortunately this performance improvement occurred at the expense of reduced specificity.
In a retrospective cohort study of nontrauma adult patients who had experienced in-hospital cardiac arrest while in the emergency department, Wang et al. [13] explored the use of the MEWS score in the periarrest setting to predict the outcome of in-hospital cardiac arrest. The authors found that the periarrest MEWS was lower in the survival-to-discharge group and that an increase in periarrest MEWS reduced the chance of survival to discharge. The authors concluded that the periarrest MEWS score might be considered “as an independent predictor of mortality after in-hospital cardiac arrest.”
Kruisselbrink et al. [14] studied the possible use of the MEWS score to identify critically ill patients in ward patients in resource poor settings, as exemplified by Mulago Hospital in Kampala, Uganda. This was a prospective observational study of 452 patients, a quarter of which were HIV positive. The authors found that the median MEWS score for their patient sample was 2 and that a multivariable analysis found that mortality was independently associated with a MEWS score over 4. The authors concluded that the MEWS score “could provide a useful triage tool to identify patients at greatest risk of death.”
4. PEDIATRIC EARLY WARNING SCORE
Another modification of the NEWS system is aimed at the pediatric population [15]. Known as PEWS, the system focuses on behaviors (playing, sleeping, irritable, lethargic etc.) as well as on cardiovascular and respiratory and “output” (urine, feces, emesis) parameters. A study from Thailand [16] validated the PEWS score in predicting hospitalization in children visiting the ED and concluded that “EWS can be helpful in predicting patient disposition in pediatric ED with acceptable validity and can serve as a potentially excellent screening tool for prediction of ICU admission.” On the other hand, a study by Breslin et al. [17] noted that while the PEWS score was helped predict the level of care at ED disposition it did not provide adequate sensitivity and specificity to be used on its own.
Similarly, Lillitos et al. [18] retrospectively studied the sensitivity and specificity of the PEWS system in predicting significant illness in 1921 children brought to two UK emergency departments. The authors found that a PEWS score over 2 had “good specificity but poor sensitivity for predicting hospital admission and significant illness” and concluded that a high PEWS score merits serious consideration but that a low PEWS score was poor at ruling out serious underlying illness.
Such limitations in the PEWS scoring system has led some investigators to ask if an alternative pediatric early warning system might be possible. One alternative that has been proposed is known as Children's Hospital Early Warning System (CHEWS) [19, 20]. In a study by McLellan et al. [19] the CHEWS system “demonstrated higher discrimination, higher sensitivity and longer early warning time than the PEWS for identifying children at risk for critical deterioration.”
In the CHEWS Score patients are scored on a scale from 0-3 based on physiologic parameters (respiratory, cardiovascular, neurological) and additionally patients receive an additional point for staff concern and/or family concern. If the CHEWS Score is 0, 1 or 2, clinicians are advised to continue routine assessment. If the CHEWS Score is 3 or 4, clinicians are advised to notify the charge nurse and resident, to increase the assessment frequency, and consider a higher level of care. If the CHEWS Score is 5 or above, consideration should be given to calling the Rapid Response Team.
Readers wishing more information on the various pediatric early warning systems may wish to consult a systematic review by Lambert et al. [21].
5. EARLY WARNING SYSTEMS FOR OBSTETRICS
The success of early warning systems in other domains has contributed to an interest amongst obstetricians and neonatologists to develop systems applicable to maternal-fetal medicine.
The idea of such initiatives would be to facilitate the early detection of conditions such as hemorrhage, thromboembolic events, or hypertension in addition to classical obstetrical concerns such as arrested labor or preeclampsia/eclampsia [22, 23]. At the 2017 Society for Maternal-Fetal Medicine Annual Meeting a series of presentations devoted to possible early warning methods for the obstetrical setting were documented in a report by Friedman et al. [24].
6. ONGOING CHALLENGES
While the use of clinical early warning systems appears to be helpful overall (the caveats mentioned above notwithstanding), a number of challenges remain. In a systematic review, Alam et al. [25] cautioned against the use of various NEWS modifications, which “together with different thresholds, and poor or inadequate methodology” made it difficult to draw comparisons between various implementations. They pointed out that general conclusions cannot “be generated from the lack of use of a single standardized score and the use of different populations” and recommended that future large multi-center trials use one standardized score in order to allow study comparisons.
Another issues is that there is a lack of consensus as to what might constitute an 'ideal' clinical early warning score system, in part because various health care systems will vary in case mix as well as in available resources (such as rapid response teams) to deal with patients identified to be at elevated clinical risk [26]. For example, oliguria, while obviously a clinically important finding, is not part of the NEWS score but is part of some other systems.
CONCLUSION
Clinical early warning systems are a potentially significant addition to the clinician’s clinical toolkit, but while immensely promising, they need to be investigated much further to determine their optimal role in monitoring patients at risk of clinical deterioration. A fundamental question that awaits a definitive answer concerns the identification of the best early warning system (NEWS, MEWS, PEWS etc.) to use for a particular clinical population (surgical, pediatric, trauma, prehospital etc.)
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


