All published articles of this journal are available on ScienceDirect.
Likely Local Anaesthetic Toxicity Following Dorsal Penile Nerve Block in an Adult. Early detection and Treatment with Lipid
Abstract
Local Anesthetic Systemic Toxicity (LAST) should be considered after Local Anesthetic (LA) injection when patients experience Central Nervous (CNS) or Cardiovascular (CV) systems signs or symptoms. While LAST is a potentially fatal complication affecting both the CNS and CV, it can present as isolated CV toxicity. We report LAST presenting as isolate CV toxicity following bilateral penile block which responded to Intravenous Lipid Emulsion (ILE).
1. INTRODUCTION
Local Anesthetic Systemic Toxicity (LAST) should be considered in any patient receiving a Local Anesthetic (LA) injection and experiencing (CNS) or Cardiovascular (CV) systems signs or symptoms. While LAST is a potentially fatal complication affecting the above systems, it can also present as isolated CV toxicity. The time course of the deterioration of initial dysrhythmias to asystole or malignant arrhythmias is not known. This potential progression may be amenable to early treatment with supportive measures, specifically Intravenous Lipid Emulsion (ILE).
The most common anesthetic techniques associated with LAST during three study review periods, 1979 -2009, 2010-2014 and 2014-2016 were epidural blocks, interscalene blocks and penile blocks respectively [1-3].The penile blocks reported were in pediatric cases only [3], with none occurring in adults. We would like to report an adult likely atypical presentation of isolated cardiac arrhythmia following bilateral dorsal penile block which responded to ILE.
2. CASE PRESENTATION
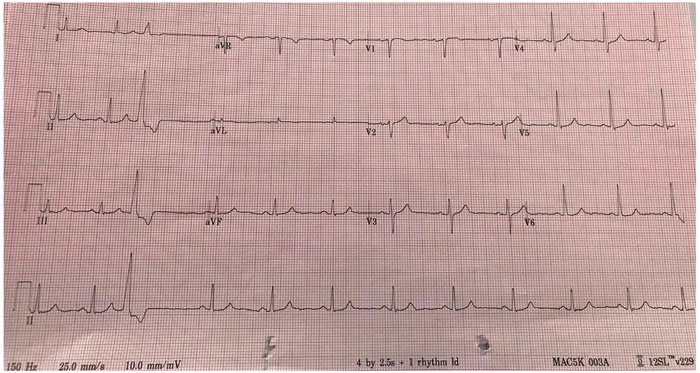
A 54-year-old man was admitted to our day surgery unit for a circumcision. His past medical history was significant for obesity (weight 112 kilograms, BMI-33), anxiety, hiatus hernia and reflux. His ECG showed occasional Ventricular Premature Contractions (VPC), but was otherwise normal (Fig. 1). His past surgical history included a tonsillectomy and colonoscopy. During a colonoscopy, under propofol sedation; the patient had myoclonic jerks followed by an episode of gastric reflux leading to airway obstruction and bradycardia. This responded to suction and placement of a nasopharyngeal airway, while the procedure was expedited. The patient was subsequently worried about another possible anesthetic reaction, and after discussion, the anaesthetic plan was to avoid propofol and use a combination of alternate intravenous induction and inhalational agents.
After attaining Intravenous (IV) access and standard monitoring, antibiotic (cefazolin 2 gms IV) was administered. Induction of anesthesia was performed with fentanyl 100 mcg, midazolam 2 mg, thiopentone 50 mg and a mixture of O2 and sevoflurane. Laryngeal mask airway (I-gel size 4) was inserted easily. Maintenance of anaesthesia was with O2, sevoflurane 1.7% and supplemental intermittent fentanyl. The surgeon requested a penile block, for perioperative analgesia that we placed under sterile conditions by inserting a 23 gauge needle at 10.30 and 13.30 hour positions at the base of the penis. The LA was injected deep into Buck's fascia following a negative aspiration for blood. A total of 16 ml of 0.5% bupivacaine (80 mg) was administered (8 ml on each side) and surgery commenced. 5 minutes after LA injection, the patient developed tachycardia with multiple VPCs. After 2 minutes, the rhythm changed to broad-based QRS complexes, with occasional VPC (Fig. 2).
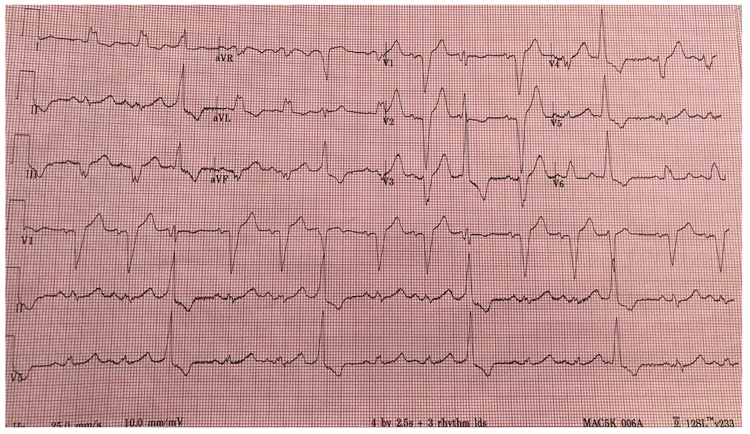
Though hemodynamically stable with BP of 130/80 mmhg, the rapidly changing rhythm was a cause of concern. Assistance (from the senior consultant) was requested to rule out possible complication from LA block leading to LAST. Other possible causes such as inadequate depth or conversely excessive anesthetic depth were ruled out. Since the patient’s clinical condition was stable, the decision was made to continue with the surgery. To avoid possible further deterioration of arrhythmias and for the benefit of cardiac protection, we thought to treat it as a LAST event and commenced ILE as per the American Society of Regional Anesthesia (ASRA) guidelines [4]. A 100 mL bolus of a 20% lipid emulsion was given over 2-3 min followed by infusion of 200 mL over 20 min. This didn’t change the arrhythmias and we commenced infusion to 0.5 mL/kg/min over 10 min with the total dose of 1000 ml. There was a minimal change in the QRS size over the period.
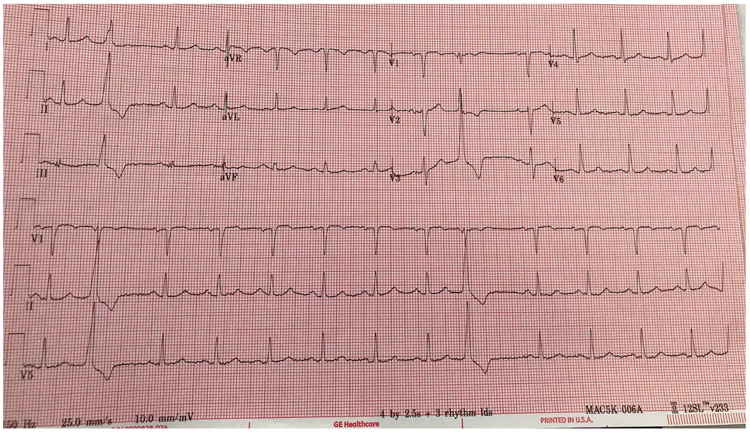
The surgeons were informed of the possible LAST event and surgery was completed swiftly and uneventfully. An arterial line was inserted to closely monitor BP and blood sample sent to rule out metabolic and electrolyte imbalance. LMA was removed once the patient was fully awake and there were no hemodynamic instability or seizures observed. During GA if any neurologic symptoms occurred that could not be evaluated. An arterial blood gas and cardiac troponin levels were reported, within normal limits. Blood was to be sent for serum bupivacaine levels, but there was no provision to do the assay either onsite or in the research lab. A cardiologist was consulted and requested to evaluate the patient in the recovery room. At this time, the patient’s cardiac rhythm had returned to baseline narrow complexes (Fig. 3). The cardiac consultant opined the event as unexplained broad complex tachycardia and advised overnight telemetry monitoring. The patient was stable overnight and discharged the next day. Echocardiography was done on outpatient basis, which showed no structural abnormality.
3. DISCUSSIONS AND RESULTS
We believe our patient had a likely LA toxicity event with atypical presentation and responded to lipid emulsion administration. An atypical presentation is said to have an onset that is delayed 5 mins or more and/or occurring with isolated CV symptoms [1]. According to the recommended classification by De Gregorio, our case falls into the IB category [1]. It is important to consider LAST following LA injection even in a low-risk group with no pre-existing cardiac or renal disease.
Atypical presentation of LAST is rare, poorly documented, rarely published and the true incidence is unknown. Most of the descriptions involve case reports, case series from registry studies and retrospective reviews on very small numbers of LAST events. Irrespective of the style of presentation, as with all cases of LAST, early recognition and treatment may help in avoiding potential fatal complications. The information on the validity of lipid use to reduce mortality is limited but available data from the lipid rescue registry with a 100% survival rate in 11 cases is encouraging [5].
The clinical response to ILE in the LAST event may be delayed and variable and it has been reported to take up to 30 minutes [6]. In our case, the patient’s ECG reverted to sinus rhythm after 45 minutes of the event. We continued prolonged monitoring as the late recurrence of LAST is possible, but this option may not be available in all institutions. Inability to measure the bupivacaine blood concentration was one of the limitations of this case report.
CONCLUSION
LAST is a potential complication which can present as classical or atypical presentations. Our case demonstrates the successful use of ILE in an atypical presentation of LAST with an isolated arrhythmia.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Consent was obtained from the subject. The study was performed using the American Society of Regional Anesthesia (ASRA) guidelines.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patients involved in the study.
CONFLICT OF INTEREST
The authors declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


