All published articles of this journal are available on ScienceDirect.
The Effect of Use of Anidulafungin on Failure of Weaning Due to Ventilator-associated Pneumonia which Complicates Contused Lungs
Abstract
Introduction:
Failure of weaning is considered as one of the most difficult challenges for any intensivist, especially in the devitalized lung due to infected lung contusion. Unsatisfactory results with prolonged treatment with the proper broad-spectrum antibiotics raise the point of exclusion of candidemia or suspected pulmonary candidiasis which is considered a major problem not only because of its increasing rate (2-10 per 1000 ICU admission) but also because of its difficult diagnosis. Patients with failure of weaning due to unresolved VAP (Ventilator-associated Pneumonia) after receiving broad-spectrum antibiotics for more than 10 days, especially in preexisting severe lung contusion should be put on empirical systemic antifungal. Echinocandins are a new class of antifungal drugs used as a reliable class for empirical systemic antifungal treatment.
Aim of Work:
The study aims to evaluate and compare the effect of the use of anidulafungin on weaning from the ventilator due to VAP which complicates traumatized contused lungs after 2 weeks from ventilation.
Patients and Methods:
This was a prospective double-blind study done on 200 patients admitted to King Abdulaziz Specialized Hospital, Taif, KSA between March 2015 and August 2018 in surgical ICU with the failure of weaning due to Ventilator Associated Pneumonia (VAP) which complicated contused lungs. Group (A) 100 patients started on antibiotics regimen according to qualitative culture for 2 weeks, while group (B) 100 patients received anidulafungin with the antibiotics regimen.
In this study, diagnosis of lung contusion was made by Computerized Axial Tomography (CT) chest, while VAP was diagnosed by a modified Clinical Pulmonary Infection Score (CPIS). A score of 6 or more was considered to be VAP.
Results:
Comparing the data of the patients in the 3 studied periods (1st 5 days, 2nd 5 days and last 4 days) controlled tracheal secretion was recorded in 15, 38 and 46 patients in group A, respectively in the 3 studied periods compared to 28, 75 and 83 in group B. Less parenchymatous lung infiltration in the chest X-ray found was in 12, 40 and 48 patients in group A compared to 24, 88 and 91 patients in group B. Improvement of the hypoxic index in 48, 76 and 85 patients in group A was compared to 66, 90 and 98 patients in group B. Normalization of temperature in 16, 36 and 54 patients in group A, while 40, 76 and 90 patients in B and reduction of total leucocytic count in 18, 35 and 57 patients in group A, while 38, 70 and 87 patients in group B were observed. There were 15 out of 98 patients in Group A who did not weaned, while only 5 out of 100 patients in group B failed to be weaned from mechanical ventilation within the study period (2 weeks).
Conclusion:
The use of anidulafungin with proper antibiotics in patients with failure of weaning due to VAP which complicated the contused lung was efficiently treated and reduced the morbidity by accelerating the weaning from the ventilator compared to the use of proper antibiotics alone.
1. INTRODUCTION
Failure of weaning patients from the ventilator is a major problem in the Intensive Care Units (ICU). More than 3% are due to unresolved pneumonia [1-3] which can be defined and diagnosed by the persistence of all parameters of Clinical Pulmonary Infection Score (CPIS) [4], (Table 1). This problem can be aggravated by preexisting devitalized lung parenchyma as in contused lung due to severe chest trauma. The cause of unresolved pneumonia can be attributed to many factors e.g. dose, duration, type of antibiotics or emergence of resistant bacteria that can deteriorate the lung condition, tuberculosis, atypical bacteria. etc. Moreover, Candida infections are one of the most common causes of failure of weaning. Invasive fungal infections account for 70-90% of all invasive mycoses [5, 6]. Among the causes of nosocomial bloodstream infections Candida ranks number four in the United States. The incidence of candidemia varies between 0.5 and 1.4 per 10,000 patient-days in the hospital and between 2 and 6.9 per 1,000 admissions in the Intensive Care Unit (ICU). Invasive candidiasis is associated with high mortality, especially in ICUs. Prompt initiation of appropriate antifungal therapy is essential for the control of invasive Candida infections and has been shown to reduce mortality [7].
| CPIS | 0 | 1 | 2 |
|---|---|---|---|
| Tracheal secretion | Rare | Abundant | Abundant & purulent |
| Chest X-ray infiltrate | No infiltrate | Diffuse | Localized |
| Temperature ºC | > 36.5 and < 38.4 | > 38.5 and < 38.9 | > 39 or < 36 |
| Leucocytic count per mm3 | > 4000and < 11000 | < 4000 or > 11000 | < 4000 or > 11000 +band form > 500 |
| Hypoxic index PaO2/FIO2 mmHg | >240 or ARDS | -- | < 240 and no evidence of ARDS |
| Microbiology | Negative | -- | Positive |
Unfortunately, early diagnosis of invasive candidiasis or pulmonary candidiasis remains a challenge, and criteria for starting empirical antifungal therapy in ICU patients are poorly defined [7-12]. Recent Infectious Disease Society of America (IDSA) guidelines suggest that empirical antifungal therapy should be considered in critically ill patients with risk factors for invasive candidiasis e.g. (failure of weaning, prolonged use of broad-spectrum antibiotics, presence of persistent leucocytosis and no other known cause of fever) [13]. However, these are so diverse that most ICU patients could be considered to exhibit risk factors for invasive candidiasis. Obviously, widespread use of antifungal agents would be associated with substantially increased overall health care costs and emergence of resistance.
To both ensure appropriate and timely antifungal therapy and to avoid unnecessary use of antifungal agents, some authors have developed clinical prediction rules to identify ICU patients at high risk of candidiasis and for whom initiation of empirical antifungal therapy could be justified. However, there are many concerns about these rules: high specificity but low sensitivity, no prospective validation, and complicated use [7-16]. So the decision to start systemic antifungal still depends on the clinical experience of an intensivist and the clinical course and the background history of the patient [17].
The failure of weaning from the ventilator due to unresolved pneumonia raise the possibility of candidemia or pulmonary candidiasis. Especially in those patients who received full antibiotics covering for a long period. This makes the use of empirical systemic antifungal mandatory to save the life of those patients. Waiting till confirmation can affect the morbidity and mortality of patients; moreover, it can increase the cost due to prolonged time of ventilation and use of more antibiotics for longer duration and leading to the emergence of resistant bugs as culturing the fungus from the blood is very difficult and needs equipped centers which may not be available in all casualty centers [14-17].
Choosing the proper antifungal agent is again a point of debate as the age, preexisting medical diseases of the patient, interaction with other drugs received by the patient, all should be considered before starting a particular systemic antifungal agent.
Echinocandins are a new class of antifungal drugs that inhibit the synthesis of glucan in the cell wall, via noncompetitive inhibition of the enzyme 1,3-β glucan synthase and are thus called “penicillin of antifungals” (a property shared with papulacandins) as penicillin has a similar mechanism against bacteria but not fungi. Beta glucans are carbohydrate polymers that are cross-linked with other fungal cell wall components (The bacterial equivalent is peptidoglycan) [18].
Anidulafungin is a semisynthetic echinocandin used as an antifungal drug. It was previously known as LY303366 . It may also have application in treating invasive Aspergillus infection [19].
Any patient having score of 6 or more is considered having VAP [4].
2. PATIENTS AND METHODS
This was a prospective double-blind study done on 200 patients admitted to King Abdulaziz Specialized Hospital, Taif, KSA between March 2015 and August 2018 in surgical ICU. King Abdulaziz research and ethical committee approved the project.
A written consent for all the patients was taken either from the patient before intubation or from the first-degree relative if a patient came to our ICU intubated. All patients were having severe chest trauma with contused lungs either with or without severe head trauma.
2.1. Inclusion Criteria
- Age group selected between 18-50 years.
- All patients intubated and ventilated either due to respiratory failure from severe lung contusion or severe head trauma with Glasgow Coma Scale (GCS) 8 or less.
- Respiratory failure diagnosed by Arterial Blood Gases (ABG) with partial pressure of oxygen (PaO2) ≤ 60 mmHg and partial pressure of carbon dioxide (PaCO2) ≥ 60 mmHg.
- Lung contusion diagnosed in our study by Computerized Axial Tomography (CT) chest.
Selected patients were ventilated for 5 days initially without both antibiotics and antifungal. During this period, sputum culture sent from the 2nd day of ventilation for qualitative culture to be collected at the end of these 5 days. After those 5 days from ventilation, 200 patients selected those who scored 6 or more on CPIS (considered VAP) and could not be weaned from the ventilator. Those 200 patients allocated randomly in two groups (100 patients in group A & 100 patients in group B) Randomization sequence was created using Excel 2007 (Microsoft, Redmond, WA, USA) with a 1:1 allocation using random block sizes of 2 and 4 by an independent doctor [20]. In this way, sequence generation and type of randomization can be expressed at the same time. Patients of group A started on broad-spectrum antibiotics according to culture collected at the end of the 5 days and revised weekly by the results of tracheobronchial lavage (BAL) culture. While patients of group B given anidulafungin 100 mg slowly by intravenous infusion once daily in the first day then 50 mg slowly by intravenous infusion once daily for 2 weeks with the proper antibiotics according to culture collected at the end of the 5 days and revised weekly by BAL culture.
The two groups were compared all over the period of the study (first 5 days, second 5 days and last 4 days) for all items of CPIS illustrated in Table 1.
The planned duration of the study is two weeks so any patient who failed to be weaned within this period was considered morbid and recorded.
2.2. Exclusion Criteria
- Age less than 18 years or more than 50 years.
- Any patient with liver or renal impairment.
- Any patient acquiring or congenital immunodeficiency syndrome.
- Any ischemic or congenital heart disease.
- Any patients receiving corticosteroid.
- Pregnant or lactating females
All ventilated patients put on intravenous analgesia; fentanyl (from 50 microgram to 100 microgram/hour) and intravenous sedation (midazolam 3-5 mg/hour) till we achieved Ramsay score -2 to -3 and the routine survey was done to all patients according to our hospital policy in the form of:
- Chest X-ray, Abdominal ultrasound, and CT brain as a routine in our hospital policy.
- Full laboratory work (CBC, complete chemistry & coagulation profile).
- APACHE II score was done for all patients.
- Temperature was documented every 3 hours for 2 weeks.
- ABG was done every 8 hours for 2 weeks.
- CBC including white cell count was done daily and for 2 weeks.
- Complete liver and renal functions daily (urea, serum creatinine level transaminase, bilirubin total and direct level).
- Chest X-ray for all the patients taken after intubation and with starting of ventilation and every 24 hours for 2 weeks.
- All patients received anti-stress medication (Omeprazole injection 20 mg intravenous every 12 hours).
- Orogastric tubes were applied to all patients & feeding was started within 24 hours after patient discharged from general surgery care.
- Daily evaluation for consciousness level and sedation and ventilation were done for all patients.
- Broncho-Alveolar Lavage (BAL) was obtained by bronchoscopy weekly and sent for culture.
- Blood culture also taken weekly for two weeks.
- Patients were tracheostomized within the first 5 days from ventilation and disconnection from the ventilator and putting the tracheostomy tube of these patients on T- piece was considered weaning of these patients.
-
The 5 points of the bundle for VAP prevention were strictly applied to all patients in both groups A&B:
- Elevation of the head 30º to 45º
- Daily evaluation for possible extubation
- Daily evaluation of the need for sedation
- The use of an endotracheal tube with subglottic secretion drainage
- Oral care with oral antiseptics
Two patients were excluded from group A as they had triple rising transaminase level 5 days and 7 days from starting antibiotics.
2.3. Statistical Analysis
Sample size calculation was conducted using Epi-save software to conduct a comparative study. The estimated sample size was made based on the assumption of 95% confidence level and 80% power of the study.
The data was collected and entered into the personal computer. Statistical analysis was done using Statistical Package for Social Sciences (SPSS/version 20) software.
The statistical tests used were as follows:
Number, percent, arithmetic mean and standard deviation. For categorized parameters, Chai square test was used. While for two groups, t-test was used for parametric data. The level of significance was 0.05.
3. RESULTS
Results are presented in Figs. (1 to 7).The demographic data of both groups are shown in Table 2.
| - | Group A 98 Patients | Group B 100 Patients | P | ||
|---|---|---|---|---|---|
| Age Group | No. | % | No. | % | |
| 18-22 years | 35 | 35.7 | 32 | 32 | 0.817 |
| 23-35 | 26 | 26.5 | 28 | 28 | |
| 36-45 | 28 | 28.6 | 27 | 27 | |
| 46-50 | 9 | 9.2 | 13 | 13 | |
| Sex | |||||
| Male | 60 | 61.2 | 84 | 84 | 0.0032* |
| Female | 38 | 38.8 | 16 | 16 | |
| Surgical causes of ventilation | |||||
| Severe head trauma with severe lung contusion | 28 | 28.6 | 35 | 35 | 0.102 |
| Moderate head trauma with severe lung contusion | 10 | 10.2 | 4 | 4 | 0.089 |
| Severe lung contusion without flail chest | 43 | 43.9 | 45 | 45 | 0.465 |
| Severe lung contusion with flail chest | 17 | 17.3 | 16 | 16 | 0.551 |
Two patients were excluded from Group A as they had triple rising liver enzymes 5 days and 7 days from starting broad-spectrum antibiotics, respectively.
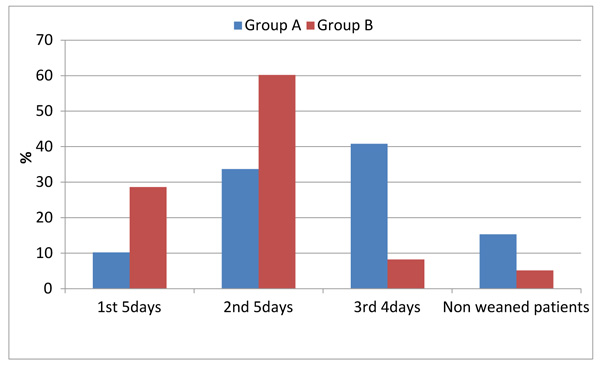
After 2 weeks (duration of the study): patients failed to be weaned from the ventilator were 15 patients from group A compared to only 5 patients from group B as shown in Table 3.
|
No. of Patients Weaned from Ventilator |
Group A “n = 98” |
Group B “n = 100” |
p | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| 1st 5days | 10 | 10.2 | 28 | 28 | 0.042* |
| 2nd 5days | 33 | 33.7 | 59 | 59 | 0.002* |
| 3rd. 4days | 40 | 40.8 | 8 | 8 | 0.001* |
| No. of Patients Failed to be Weaned | 15 patients | 15.3 | 5 patients | 5 | 0.098 |
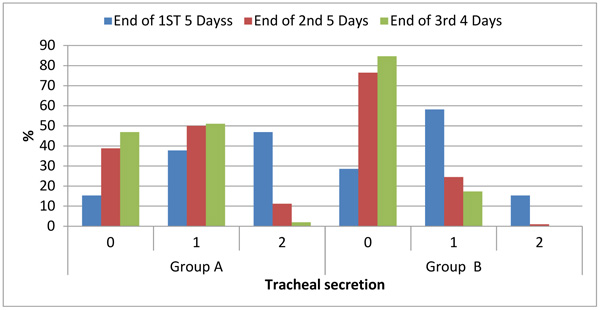
About the control of local signs of unresolved VAP in contused lung:
Table 4 compares nature and amount of tracheal secretion in both groups all over the duration of the study and showed that a significantly higher number of patients had normal tracheal secretion in group B compared to group A. As 28,75 and 83 patients in group B had normal tracheal secretion in the 1st 5 days, 2nd 5 days and last 4 days consecutively compared to 15, 38 and 46 patients in group A who had the same results in the same duration.
| Score | Group A (n = 98) | Group B (n = 100) | p | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 0 | 1 | 2 | ||||||||
| End of 1ST 5 Days | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Tracheal secretion | 15 | 15.3 | 37 | 37.8 | 46 | 46.9 | 28 | 28 | 57 | 57 | 15 | 15 | 0.013* |
| Chest X-ray infiltrate | 12 | 12.2 | 54 | 55.1 | 32 | 32.7 | 24 | 24 | 28 | 28 | 48 | 48 | 0.027* |
| Temperature | 16 | 16.3 | 67 | 68.4 | 15 | 15.3 | 40 | 40 | 50 | 50 | 10 | 10 | 0.001* |
| Leucocytic count/mm3 | 18 | 18.4 | 65 | 66.3 | 15 | 15.3 | 38 | 38 | 51 | 51 | 11 | 11 | 0.0159* |
| PaO2/FIO2 mmHg | 48 | 49.0 | ---- | 0.0 | 50 | 51.0 | 66 | 66 | ---- | 0.0 | 34 | 34 | 0.102 |
| Microbiology | 33 | 33.7 | ---- | 0.0 | 65 | 66.3 | 49 | 49 | ---- | 0.0 | 51 | 51 | 0.215 |
| End of 2nd 5 Days | |||||||||||||
| Tracheal secretion | 38 | 38.8 | 49 | 50.0 | 11 | 11.2 | 75 | 75 | 24 | 24 | 1 | 1.0 | 0.0224* |
| Chest x-ray infiltrate | 40 | 40.8 | 50 | 51.0 | 8 | 8.2 | 88 | 88 | 12 | 12 | 0 | 0.0 | 0.003* |
| Temperature | 36 | 36.7 | 54 | 55.1 | 8 | 8.2 | 76 | 76 | 24 | 24 | 0 | 0.0 | 0.015* |
| Leucocytic count/mm3 | 35 | 35.7 | 61 | 62.2 | 2 | 2.0 | 70 | 70 | 30 | 30 | 0 | 0.0 | 0.025* |
| PAO2/FIO2 mmHg | 76 | 77.6 | ---- | 0.0 | 22 | 22.4 | 90 | 90 | ---- | 0.0 | 10 | 10 | 0.096 |
| Microbiology | 45 | 45.9 | ---- | 0.0 | 53 | 54.1 | 69 | 69 | ---- | 0.0 | 31 | 31 | 0.016* |
| End of Last 4 Days | |||||||||||||
| Tracheal secretion | 46 | 46.9 | 50 | 51.0 | 2 | 2.0 | 83 | 83 | 17 | 17 | 0 | 0 | 0.001* |
| Chest x-ray infiltrate | 48 | 49.0 | 48 | 49.0 | 2 | 2.0 | 91 | 91 | 9 | 9 | 0 | 0 | 0.001* |
| Temperature | 54 | 55.1 | 42 | 42.9 | 2 | 2.0 | 90 | 90 | 10 | 10 | 0 | 0 | 0.001* |
| Leucocytic counts/mm3 | 57 | 58.2 | 39 | 39.8 | 2 | 2.0 | 87 | 87 | 13 | 13 | 0 | 0 | 0.0025* |
| PAO2/FIO2 mmHg | 85 | 86.7 | ---- | 0.0 | 13 | 13.3 | 98 | 98 | ---- | 0 | 2 | 2 | 0.625 |
| Microbiology | 78 | 79.6 | ---- | 0.0 | 20 | 20.4 | 100 | 100 | ---- | 0 | 0 | 0 | 0.002* |
| Morbidity (failure of weaning within 2 weeks) | 15 patients out of 98 failed to be weaned within the period of the study | 5 patients out of 100 failed to be weaned within the period of the study | 0.098 | ||||||||||
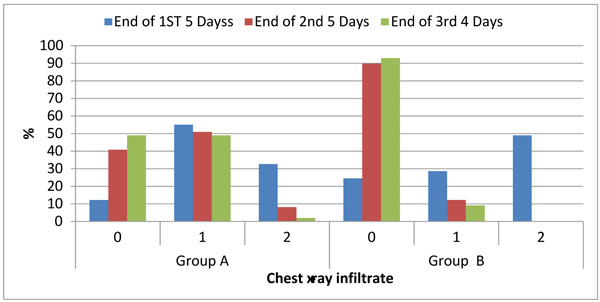
3.2. Chest X Ray
Table 4 compares parenchymatous lung infiltration in the chest X-ray of both groups all over the duration of the study and showed that significantly higher number of patients had normal chest X ray in group B compared to group A. As 24,88 and 91 patients in group B had normal chest X ray in the 1st 5 days, 2nd 5 days and last 4 days consecutively compared to 12, 40 and 48 patients in group A who had the same results in the same duration.
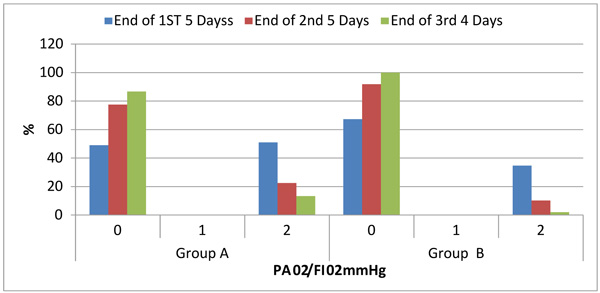
3.3. Hypoxic Index PaO2/FIO2
Table 4 compares hypoxic index in both groups all over the duration of the study and showed that a significantly higher number of patients had hypoxic index more than 240 in group B compared to Group A. As 66, 90 and 98 patients in group B had these results in the 1st 5 days, 2nd 5 days and last 4 days consecutively compared to 48, 76 and 85 patients in group A who had the same results in the same duration.
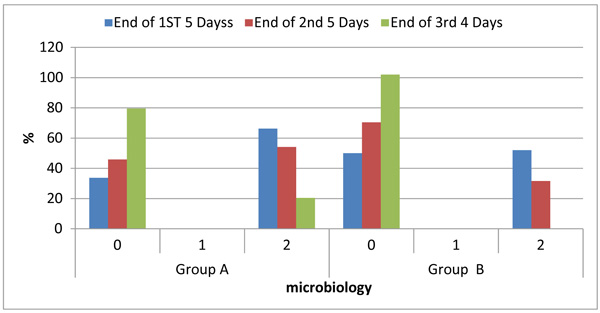
3.4. Qualitative Sputum Culture from BAL
Table 4 compares qualitative BAL culture in both groups all over the duration of the study and showed that a significantly higher number of patients had negative qualitative BAL culture in Group B compared to group A. As 49, 69 and 100 patients in group B achieved these results in the 1st 5 days, 2nd 5 days and last 4 days consecutively compared to 33, 45 and 78 patients in Group A who had the same results in the same duration.
The control of systemic signs of unresolved VAP in contused lung through.
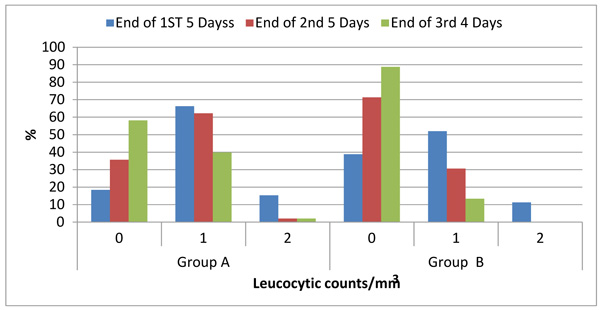
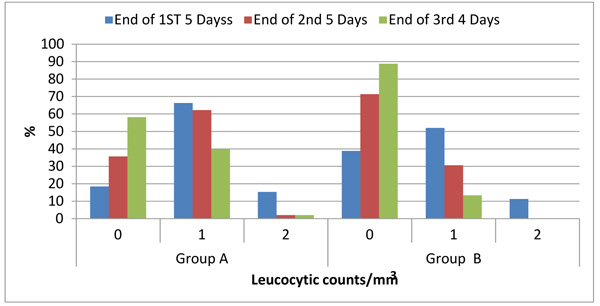
3.5. Leucocytic Count
Table 4 compares leucocytic count in both groups all over the duration of the study and showed that a significantly higher number of patients had normal leucocytic count (> 4000 and < 11000) in group B compared to Group A. As 38,70 and 87 patients in Group B had normal leucocytic count in the 1st 5 days, 2nd 5 days and last 4 days consecutively compared to 18, 35 and 57 patients in group A who had the same results in the same duration.
3.6. Temperature
Table 4 compares recorded core temperature in both groups all over the duration of the study and showed that a significantly higher number of patients had normal core temperature (> 36.5 and < 38.4) in group B compared to group A. As 40,76 and 90 patients in group B achieved normal temperature in the 1st 5 days,2nd 5 days and last 4 days consecutively compared to 16, 36 and 54 patients in group A who had the same results in the same duration.
Table 3 compares the number of patients weaned from the ventilators in both groups all over the duration of the study and showed the non-significant higher number of weaned patients in group B (95 patients) compared to group A (85 patients) at the end of the studied period. This was considered morbidity in our study.
4. DISCUSSION
All patients of group B completed the course of anidulafungin without any reported abnormality in the liver or kidney function tests. This is because anidulafungin significantly differs from other antifungal medications in that it undergoes chemical degradation to inactive forms at body pH and temperature. Since it does not rely on enzymatic degradation or hepatic or renal excretion, the drug is safe to use in patients with any degree of hepatic or renal impairment. The control of both the systemic and local signs of VAP is considered the cornerstone in the management even before complete bacteriological cure as rapid weaning from the ventilator depends on controlling both local and systemic signs of VAP.
The control of local signs of unresolved VAP through:
- Tracheal Secretion:
A number of patients had normal tracheal secretion which was significantly higher in group B compared to group A all over the duration of the study which was divided into three periods (end of the 1st 5 days, end of the 2nd 5 days and end of the last 4 days). This proved the better clinical improvement of groupe B compared to group A. This could be due to better control of pulmonary candidiasis which might be present but not diagnosed because of difficult isolation of candida or other fungi species from the broncho-alveolar lavage and blood.
- Negative Qualitative Bacteriological Culture from BAL:
A number of patients had negative qualitative BAL culture which was significantly higher in group B compared to group A. This proved the better bacteriological improvement of group B which could be explained by the tight control of both broad-spectrum antibiotics with anidulafungin for the pulmonary infection compared to broad-spectrum antibiotics alone and proved that pulmonary candidiasis should be suspected in any patient with prolonged ventilation especially with compromised lung like the contused one.
- Hypoxic index PaO2/FIO2: Number of patients had hypoxic index more than 240 which was significantly higher in group B compared to group A. This proved the better tissue oxygenation of group B which could be explained by the rapid control of both local and systemic signs of VAP inflammation.
- Chest X-ray: Number of patients had normal chest X-ray which was significantly higher in group B compared to group A. This proved that the improvement of patients in group B was not only on the clinical level but also there was a significant radiological improvement.
The control of systemic signs of unresolved VAP in contused lung through:
- Leucocytic Count:
The number of patients having normal leucocytic count (> 4000 and < 11000) was significantly higher in group B compared to group A. This proved the better control of systemic manifestation of VAP in patients of group B compared to patients of group A and could be explained by the tight control of the highly suspected candidemia in prolonged ventilated patients by both broad spectrum antibiotics with anidulafungin compared to broad spectrum antibiotics alone.
- Temperature:
The number of patients having core temperature between 36.5 to 38.4 °C was significantly higher in group B compared to group A throughout the duration of the study. This could be explained by the former explanation.
The unique effective action of anidulafungin on both candida and aspergillus species including those resistant to fluconazole or amphotericin B explained the excellent control of both systemic and/or pulmonary fungus infection which might be present in those patient who had contused lungs and ventilated for long duration but difficult to isolate. This also explained the rapid control of both local and systemic signs of VAP and early weaning of patients of group B.
So the use of systemic antifungal is helpful either with local deterioration in the immunity (devitalized contused lung) or with systemic immuno-compromised patients as renal failure, cancer patients and patients on corticosteroids etc.
The results of our study support a study conducted in 2011 by Ostrosky-Zeichner et al. [21] about candidemia in intensive care units and stated that approximately 15% of health-care associated infections are caused by fungi and Candida accounts for 70-90% of all invasive infections.
Candida spp. is included in the 10 most common microorganisms causing Bloodstream Infections (BSI). North American and European studies showed that yeasts belonging to genus Candida ranged from the fourth to the tenth most common cause of pulmonary fungal infection [22].
Eggimann P, Pittet D. in 2014 found that one third of candidemia in any hospital occurs in the ICU and since it is difficult to isolate and diagnose, it is responsible for 50% to 60% mortality rate in ICU [23].
Chen Li et al. in 2015 published in internal medicine that candidemia is the fourth most common nosocomial bloodstream infection in the United States and the seventh in Europe in Intensive Care Units (ICUs) and its mortality is high among prolonged ventilated patients [7, 24].
Thierry Calandra et al. published in critical care 2016 that Candida species account for 70-90% of invasive fungal infections especially in critical care patients and they stated that the use of broad-spectrum antibiotics, parenteral nutrition, hemodialysis, and mechanical ventilation were the most important risk factors for candidemia [25].
The end result is that usage of empirical systemic antifungal depends on clinical experience of the intensivist and understanding the background problems of the patient. In some practical situations it could be useful and decrease the cost on the patients by early weaning and shortening the ICU stay.
CONCLUSION
The use of anidulafungin with proper antibiotics in patients with failure of weaning due to VAP which complicates the contused lung, efficiently treats VAP and lessens the morbidity by accelerating the weaning from the ventilator compared to the use of proper antibiotics alone.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was conducted under the guidelines of the Ethical Committee of King Abdul Aziz Hospital, Taif, Saudi Arabia.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
A written consent for all the patients was taken.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


