All published articles of this journal are available on ScienceDirect.
A Comparative Study of Three Nebulized Medications for the Prevention of Postoperative Sore Throat in the Pediatric Population
Abstract
Background:
The delivery of aerosolized drugs is a vital component of treatment for many respiratory disorders. We used this mode of medication delivery as a pre-emptive strategy to alleviate a Postoperative Sore Throat (POST) in children receiving general anesthesia.
Objectives:
The primary aim of the study was to compare the effects of prophylactic ketamine, magnesium sulfate and dexamethasone nebulization, on the intensity of POST.
Methods:
Through a prospective, randomized, double-blind study, data were collected from children (6-16 years) undergoing surgeries from March 2018 to May 2018. The patients were allocated into 3 equivalent groups (36 patients each). Preoperative nebulization was performed for all patients. Group M received 40 mg/kg magnesium sulphate, group K received 1 mg/kg ketamine, and group D received 0.16 mg dexamethasone. The primary outcome of the study was the incidence and intensity of POST at the 4th postoperative hour. The secondary outcomes included evaluation of adverse effects specifically nausea, vomiting, postoperative cough and postoperative sedation.
Results:
Patients in the K group had the lowest incidence of POST compared to patients in groups M and D, specifically, at the 4th - postoperative hour (p-value = 0.003).
Conclusions:
Preoperative nebulization with ketamine was more effective in reducing the intensity of POST in pediatric patients postoperatively without systemic adverse effects.
1. INTRODUCTION
Postoperative Sore Throat (POST) is ranked by the American anesthesiologist as the 8th most undesirable subjective complaint following General Anesthesia (GA) [1]. The severity of POST is categorized on a 4-point scale as described by Stout et al. [2]. The severity of POST is at its peak two to four hours after extubation and decreases gradually in 24 hours [3]. POST may affect up to 42% of postoperative pediatric patients [4]. The etiology of POST is multifactorial, including the choice of airway device, high Endotracheal Tube (ETT) cuff pressure, surgical manipulation of the airway, airway suctioning and the type and length of surgery [5]. Preoperative risk factors such as asthma or a dry cough increase the probability of developing POST [6]. The highest POST incidence was observed after tracheal intubation (45.4%) when compared to laryngeal mask (17.5%) and open mask (3.3%) [5].
It is necessary to search for pre-emptive strategies to relieve POST. Different approaches attenuating POST, including non-pharmacological or pharmacological approaches have been evaluated. The non-pharmacological techniques include: using supraglottic airway devices and cuffed oral tracheal tubes. Likewise, gentle esophageal suctioning, minimizing intracuff pressure to be less than 20 cm H2O and extubation when the tracheal cuff is fully deflated; have the advantage of decreasing POST occurrence [7]. The pharmacological methods include various pre-, intra-, and postoperative drugs such as corticosteroids [8], local anesthetic agents [9], Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) [10], α2 agonists [11] and ketamine [12]. The ease of administration, ability to reach distal airways and safety; make nebulization a good method of drug delivery [13].
In this study, we investigated the preoperative nebulization of 3 medications; steroids, ketamine and magnesium. The inhaled corticosteroids deliver the drug to the site of action without systemic effects. It has been described that dexamethasone was effective for relieving of sore throat [14]. Ketamine and MgSO4, on the other hand, are N-methyl-D-aspartate (NMDA) receptor antagonists. Experimental studies showed that peripherally administered NMDA receptor antagonists were involved in anti-nociception and anti-inflammatory cascades, thus preventing POST [15]. Subsequently, ketamine gargle [16] and ketamine nebulizer [17] were investigated in reducing the incidence and intensity of Sore Throat (ST). Also, magnesium has also been used in the form of nebulization to prevent ST. Nebulization could be considered better than gargle for the following reasons: nebulization is an easy way to administer the drug, a smaller volume of drug is required, the patient is spared the pungent taste of gargled medications, better patient cooperation is likely, and there is no risk from aspiration [18].
However, no study has compared these 3 medications together. Hence, in this study, we aimed to investigate and compare the efficacy of preoperative nebulization with ketamine, dexamethasone and magnesium in attenuating the risk of POST at the most critical time (4th postoperative hour) in the pediatric age group.
2. METHODS
After obtaining approval from the Ain Shams University local ethics committee and written informed consent from representative of patients, 108 patients were enrolled in our study. This study was conducted in accordance with the current Declaration of Helsinki. The age ranged from 6 to 16 years in ASA physical status I and II patients of either sex undergoing surgeries in the supine position under general anesthesia lasting for > one hour. Patients with Mallampati class > 2, preoperative ST, upper respiratory tract infection, an allergy to the study drug, surgeries requiring nasogastric tube or throat pack insertion, surgeries with a duration > 3 hours and surgeries in the lateral and prone position were excluded from the study. Legally acceptable presentative of patients not willing to provide their voluntary written informed consent also led to their exclusion from the study.
Patients were randomized into three groups (36 patients each). Patients’ randomization was performed with the help of computer-generated random number tables in opaque sealed envelopes prepared by an anesthesiologist who was not part of the study. The envelopes (which were prepared by an anesthesiologist who was not part of the study) were opened by the staff nurse who was not involved in the study, and nebulization solution was prepared. Preoperative nebulization was performed for all patients. Group K (ketamine group) received 1 mg/kg ketamine nebulization, group M (magnesium group) received 40 mg/kg magnesium sulphate and group D (dexamethasone group) received a fixed dose of dexamethasone: 0.16 mg and the volume of each drug was brought up to 5 mL by normal saline [19-21]. The 5 mL preparations were prepared and administered by the staff nurse who did not participate in subsequent assessment according to the envelope assigned. The study drug was administered to patients via a nebulization mask connected to a wall-mounted oxygen driven source (8 L/min) for 15 minutes before induction of anesthesia. POST intensity score was taken by an anesthesiologist who was blinded to study drugs.
Patients were blinded to the tested drugs. Assessment of the acceptability of nebulized drugs was performed with the acceptability score (Score 0: Acceptable, Score 1: Not acceptable due to either nebulization or taste of the drug, Score 2: Not acceptable due to both nebulization and taste). Patients showing no difficulty during nebulization indicated an acceptable outcome and were given a score of 0. If the patients complained of any difficulty during nebulization or of the pungent taste of the drug, they were given a score of 1. Patients complaining of both difficulties during nebulization and the pungent taste of the drug were given a score of 2.
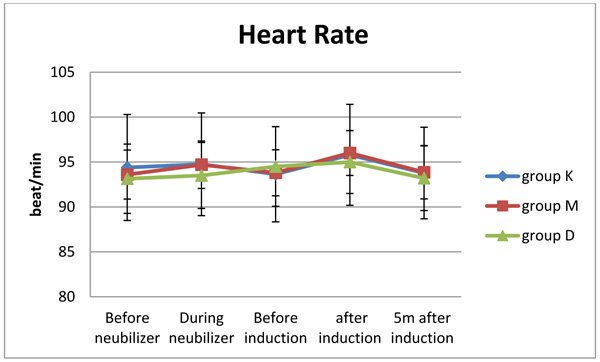
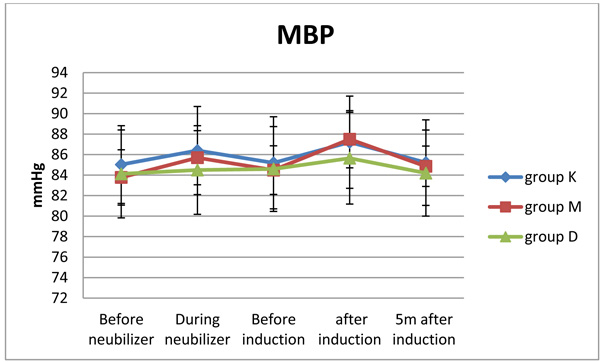
Patients were then transferred to the operation theatre; standard monitors were applied (non-invasive blood pressure, electrocardiogram, capnography and pulse oximetry) before the induction of anesthesia. Intravenous access was secured and Ringer Lactate (RL) drip was started at the rate of 5mL/kg/hr. The infusion rate was tailored to each patient according to intraoperative requirements. Patients were preoxygenated with 5 L/min 100% O2 for 3-5 min. and premedicated with 0.02 mg/kg midazolam intravenously (i.v.). Induction was performed with 2µ/kg fentanyl i.v., 2 mg/kg propofol i.v., endotracheal intubation using the correct size tube according to patients' weight (internal diameter = weight (kg) / 10 + 3.5 mm) [22]. The endotracheal tubes were made of sterile polyvinyl chloride (ULTRAMED® endotracheal tube, Made in Egypt). Direct laryngoscopy was performed using Macintosh laryngoscope blade size 2 or 3 (based on the patient body weight) by an experienced anesthesiologist. Intubation was facilitated with 0.5 mg/kg atracurium intravenously (i.v.). Heart Rate (HR) and mean blood pressure (MAP) were recorded: before nebulization, during nebulization then before and just after induction and 5 minutes after induction. GA was maintained with 50% oxygen in air and 1.2 MAC isoflurane and 0.1 mg/kg iv atracurium (given every 20 minutes). At the end of surgery, neuromuscular blockade was reversed with a combination of 0.05 mg/kg neostigmine i.v. and 0.03 mg/kg atropine i.v. Gentle oral suctioning was performed under direct vision and then extubation was performed on the return of spontaneous ventilation and when the patient could follow commands. In the recovery room, patients received O2 at 2.5 L/min via a face mask.
The Ramsay sedation score was calculated at the time of extubation and 1 hr. postoperatively for sedation assessment [23]. 1 = Awake; agitated or restless or both; 2 = Awake; Cooperative, oriented, and tranquil; 3 = Awake but respond to commands only; 4 = Asleep; brisk response to light glabellar tap or loud auditory stimulus; 5 = Asleep; sluggish response to light glabellar tap or loud auditory stimulus; and 6 = Asleep; no response to glabellar tap or loud auditory stimulus.
Regarding our primary aim “POST”; its intensity was recorded specifically at the 4th postoperative hour. ST was scored on a four-point scale (0–3) [24]. 0 = No ST; 1 = mild ST (complains of ST only on asking); 2 = moderate ST (complains of ST on his/her own); and 3 = severe ST (change in voice or hoarseness, associated with throat pain). The protocol for pain management was prescribed as 15 mg/kg paracetamol i.v. every 6 hours started from arrival to the PACU. The secondary outcomes included (in addition to postoperative sedation): evaluation of other adverse effects, such as nausea, vomiting and cough specifically during the first postoperative hour.
2.1. Statistical Analysis
The incidence of POST at the 4th postoperative hour was the primary outcome in this study and was compared using Chi-square test with 2 degrees of freedom. A sample size of 108 achieved 80% power to detect an effect size (W) of 0.30 using a 2 degrees of freedom Chi-square test with a significance level (alpha) of 0.05.
Data were analysed using SPSS 21.0 for Windows (SPSS, Chicago, IL, USA). Analysis of variance was used to compare the quantitative parametric data of three groups with post hoc Tukey’s test that was performed if there was a significant difference among the groups and a Kruskal- Wallis test that was used for quantitative non-parametric data. The Chi-square test or Fisher Exact test was used to compare the qualitative data as appropriate. Continuous parametric data were presented as the mean ± SD; non-parametric data were presented as the median (IQR) and categorical data were presented as the number of patients. P-values of < 0.05 were considered significant
3. RESULTS
All patients completed the study. No differences in patient characteristics were observed among the 3 groups. Additionally, the satisfaction score was not significantly different among the 3 groups, showing excellent satisfaction (Table 1). Moreover, no significant differences in the MAP and HR were observed among the 3 groups at any of the examined time points (Figs. 1 and 2).
Just after extubation, sedation was more prominent in the ketamine and magnesium groups than in the dexamethasone group, but the difference was statistically non-significant (p-value = 0.67). The dexamethasone group showed no sedated cases (Table 2). One hour later, all patients in the 3 groups were fully awake.
| Parameters | Group K (n=36) | Group M (n= 36) | Group D (n=36) | p-value |
|---|---|---|---|---|
| Age (Years) | 11.08±2.66 | 10.9±2.39 | 10±2.59 | 0.056 |
| Sex (Male / Female) | Males=23(64%) Females=13(36%) |
Males=24(67%) Females=12(33%) |
Males=22(61%) Females=14(39%) |
0.94 |
| Weight (Kg) | 31.14±5.4 | 29.4±4.06 | 29.56±6.2 | 0.316 |
| ASA (I / II) | ASAI=35(97%) ASA II=1(3%) |
ASAI=34(94%) ASA II=2(6%) |
ASAI=33(92%) ASA II=3(8%) |
0.487 |
| Duration of the procedure (minutes) | 74.8±11.5 | 74.03±7.25 | 73. 26±6.24 | 0.768 |
| Mallampati (I / II) | I =30(83%) II= 6(17%) |
I =32(89%) II=4(11%) |
I=29(81%) II=7(19%) |
0.729 |
| Intubation attempts (1 / 2) | 1=36(100%) 2=0(0%) |
1=34(94%) 2=2(6%) |
1=32(89%) 2=4(11%) |
0.221 |
| Type of surgery: | 0.745 | |||
| - Unilateral Inguinal hernia | 18(50%) | 18(50%) | 18(50%) | |
| - Bilateral inguinal hernia | 7(19%) | 5(14%) | 6(17%) | |
| - Fracture upper limb | 3(8%) | 4(11%) | 3(8%) | |
| - Skin graft | 2(6%) | 3(8%) | 3(8%) | |
| - Hydrocele | 4(11%) | 4(11%) | 3(8%) | |
| - Undescended testis | 2(6%) | 2(6%) | 3(8%) | |
| Satisfaction score | 0(0-1) | 0(0-1) | 0(0-1) | 0.48 |
| Time |
Group K (n=36) |
Group M (n= 36) |
Group D (n=36) |
p-value |
|---|---|---|---|---|
| At extubation | 2 (2-3) | 2 (2-3) | 2 (2-2) | 0.67 |
| 1hour after extubation | 2 (2-2) | 2 (2- 2) | 2 (2-2) | 0.125 |
On the other hand, POST incidence at the 4th hour after the operation was significantly less in the ketamine group than in the magnesium and dexamethasone groups (p-value = < 0.003) (Table 3).
| Patients & Score |
Group K (n=36) |
Group M (n= 36) |
Group D (n=36) |
p-value |
|---|---|---|---|---|
| Number of patients with Score 0 | 8 (22.22%) | 1 (2.78%) | 1 (2.78%) | 0.003* |
| Number of patients with Score 1 | 13 (36.11%) | 6 (16.67%) | 8 (22.22%) | |
| Number of patients with Score 2 | 15 (41.67%) | 25 (69.44%) | 24(66.67%) | |
| Number of patients with Score 3 | 0 (0%) | 4 (11.11%) | 3 (8.33%) |
Side effects in the form of vomiting appeared more often in the magnesium group (3 cases) and ketamine group (2 cases). While on the other hand, the dexamethasone group showed no cases of vomiting (p-value= 0.238) (Table 4). That was statistically non-significant although clinically significant.
| Symptoms |
Group K (n=36) |
Group M (n= 36) |
Group D (n= 36) |
p-value |
|---|---|---|---|---|
| Vomiting | 2 | 3 | 0 | 0.238 |
| Cough | 5 | 5 | 2 | 0.478 |
The incidence of cough was lower in the dexamethasone group (2 cases) than in the ketamine (5 cases) and magnesium groups (5 cases), but this difference was also statistically non-significant although clinically significant (p-value = 0.478) (Table 4).
4. DISCUSSION
In this study, we evaluated the effect of using three different nebulized medications preoperatively on the incidence of POST in pediatric patients: ketamine, magnesium sulphate and dexamethasone. We found that patients in the ketamine group had the lowest incidence of POST compared with patients in group M and group D specifically at the 4th postoperative hour. The 4th postoperative hour was selected as it was found that the peak incidence of POST was at 2 to 4 hours [25]. Additionally, we reported a lower incidence of postoperative cough in group D (only 2 cases) than in group K and group M, but the difference among the three groups was non-significant.
The side effects of the nebulized drugs used (including nausea, vomiting, and sedation) were minimal and non-significant among the three groups. This result may be attributed to the inhaled drugs displaying minimal systemic absorption, hence resulting in reduced systemic side effects. Additionally, the hemodynamic effects of nebulized medications were minimal and non-significant. This result was in concordance with the results of multiple studies [26-28]
The anti-sore throat effect of nebulized ketamine and magnesium was achieved by their topical effect on NMDA receptors present peripherally together with their anti-nociception and anti-inflammatory actions [29]. A study performed by Reddy and Fiaz [19] compared three different doses of nebulized ketamine and concluded that nebulized ketamine at 1 mg/kg and 1.5 mg/kg was more effective than nebulized ketamine at a dose of 0.5 mg/kg in preventing POST. This result was in concurrence with our study which used nebulized ketamine at a dose of 1 mg/kg. Another study performed by Amingad and Jayaram [30] compared preoperative ketamine via nebulization versus ketamine gargle in attenuating POST. The researchers concluded that the incidence of ST was lower in the nebulized ketamine group than in the gargle group, but there was no statistically significant difference between the groups. Jain et al. [17] compared ketamine nebulization with ketamine clonidine mixture nebulization and found greater attenuation of POST by ketamine clonidine mixture nebulization than by ketamine nebulization only but the difference between the two groups was not statistically significant. The serum ketamine level was measured in a study performed by Chan et al. [31] on adult patients undergoing elective gynecological procedures and the results showed a low serum level of ketamine after preoperative ketamine gargle, suggesting a potent topical effect from ketamine effect. However, ketamine gargle was not advised for children due to its bitter taste, the large volume needed, the increased risk of aspiration and the need for patient cooperation.
Regarding magnesium, Gupta et al. [13] investigated the effect of preoperative magnesium sulphate nebulization and found a significant reduction in the incidence of POST during rest and during swallowing. Borazan et al. [32] studied the use of preoperative magnesium lozenge (MgCL2, 610 mg) for the attenuation of POST and concluded that there was a significant reduction in the incidence of POST at 2 hours and 4 hours, but not at 24 hours.
Lastly, dexamethasone is a prophylactic inhaled corticosteroid that can be used preoperatively as an anti-inflammatory to treat reactive airway diseases such as bronchial asthma and pharyngitis. The inhalational route had the advantage of reduced systemic side effects compared to the parenteral route because of limited systemic absorption. A study performed by Chen et al. [33] concluded that the use of prophylactic inhaled budesonide can decrease the incidence and severity of POST and hoarseness of the voice after general anesthesia among patients undergoing thyroid surgery.
There were many limitations to our study. First, we did not continuously measure the intracuff pressure throughout the operation. Second, the serum level of drugs used in the study was not estimated, so we cannot exclude the systemic effect of these drugs on attenuating POST. Third, the scale used for the assessment of POST was subjective. Therefore, there may be bias. Fourth, analgesics given to patients for surgical analgesia can interfere with our assessment. Finally, there was no ideal method for estimating the dose of nebulized drugs given to children.
CONCLUSION
Preoperative nebulization with ketamine was effective in reducing the incidence and severity of POST in pediatric patients specifically at the 4th postoperative hour without systemic side effects.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The work was approved by the Ethics Committee of Ain Shams University (FMASU R 14/2018).
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent from all representative of patients were obtained.
CONFLICTS OF INTEREST
We have no affiliations with or involvement in any organization or entity that we have any financial interests.
ACKNOWLEDGEMENTS
This study was done in the pediatric surgical department of Ain Shams university educational hospital, Cairo, Egypt.


