All published articles of this journal are available on ScienceDirect.
Comparison of Ropivacaine-Fentanyl with Bupivacaine-Fentanyl for Labour Epidural Analgesia
Abstract
Background:
Bupivacaine with opioid is commonly used for labour epidural analgesia. Ropivacaine is considered as an alternative to bupivacaine due to its lower cardiovascular complications. However, there is a controversy regarding the efficacy of these drugs as some studies suggest equivalent action, whereas others report that ropivacaine produces less motor blockade. The study aimed to compare the effect of ropivacaine-fentanyl and bupivacaine-fentanyl for labour analgesia.
Materials and Methods:
The prospective randomized study was performed on 60 parturients, divided into two groups of 30 subjects each. Group I received 10ml of bupivacaine 0.1% + fentanyl 2µg/ml and Group II received 10ml of ropivacaine 0.1% + fentanyl 2µg/ml by epidural catheter. Pre-anaesthetic evaluation was performed on all the participants and all were administered metoclopramide 0.25mg/kg and ondansetron 0.08-0.1mg/kg intravenously as premedication. The baseline and post anaesthesia systolic, diastolic blood pressure, heart rate, VAS score, degree of motor block, sedation and APGAR score of the baby were recorded. The data were tabulated and statistically analyzed.
Results:
When compared, there was no significant difference in systolic/diastolic blood pressure in two groups except at 360 min where diastolic pressure was low in group II. Significantly higher heart rate at 30 min (P=0.0003), 120 min (0.006), and 300 min (P=0.001) was observed in group I subjects. VAS score was significantly less at 180 min (P=0.019) and 300 min (P=0.019) in group II. Adverse effects such as fetal bradycardia, nausea/vomiting and hypotension observed were clinically insignificance when compared in two groups.
Conclusion:
Bupivacaine and ropivacaine produce an equal degree of analgesia and hemodynamic stability in 0.1% of concentration when added with 2µg/ml fentanyl . However, heart rate was well maintained with lower VAS scores in group II receiving ropivacaine. No significant difference in the side effects between the two groups. Hence, Ropivacaine can be used as a safe alternative to bupivacaine for labour epidural analgesia.
1. INTRODUCTION
Maternal stress response induced by labour pain is neither beneficial for the mother nor for the foetus [1] Inability to bear the pains of labour is one of the reasons for elective caesarean sections [2, 3]. Additionally, it causes maternal sympathetic activation leading to uncoordinated uterine activity and compromises the foetal oxygenation. Hence, pain relief is important in preventing maternal and perinatal morbidity and reducing the chances of caesarean section due to maternal anxiety [4]. Neuroaxial technique of epidural analgesia is the most popular and effective method of pain relief in labour [5]. The major advantages are no risk of gastric aspiration, avoidance of depressant general anaesthetic drugs and allows the mother to be awake to participate in the delivery. Ideal analgesic drugs should have a long duration of action with less motor blockade, limited perinatal transfer, and no adverse effects on the mother and fetus. So combination of opiods with Local Anaesthetic (LA) was shown to be more effective compared with LA alone [6, 7]. For this reason, LA bupivacaine is commonly used. Despite wide spread utility and relative safety of bupivacaine, ropivacaine and levobupivacaine were developed to decrease cardiac risks and CNS toxicity. Moreover, these agents cause less motor blockade compared to bupivacaine. Ropivacaine being 40% less potent than bupivacaine and having a tendency for differential blockade, is preferred for labour analgesia [8]. Along with LA, opioids (fentanyl or sufentanil) are used to reduce the dose and adverse effects of the anaesthetic agents [9]. The purpose of the study was to evaluate and compare the effect of bupivacaine –fentanyl and ropivacaine-fentanyl in the control of labour pain, effects on hemodynamics and fetus as well as observe the side effects or complications.
2. MATERIALS AND METHODS
This prospective randomized study was performed at a tertiary care centre in Kolhapur, India, after approval by the Institutional Ethics and Review board (DYPMCK/PG-14/ 1721/15-16). Subjects were allotted to one of the two groups (Group I & II) by computer generated number criteria, each consisting of 30 subjects. On obtaining written informed consent, 60term parturients (primigravida and gravida 2nd or 3rd) of ASA grade I and II, aged between 19-40 years who had mild pregnancy-induced hypertension or requested epidural labour analgesia were included in the sample. Parturients with severe pregnancy-induced hypertension, eclampsia, severe anaemia, previous caesarean section, cephalopelvic disproportion, breech presentation, allergy to anesthetics, bleeding disorders, psychological/neurological disease and severe spine deformities were excluded from the study. All parturients were thoroughly assessed and investigated for routine blood counts, PT-INR, blood sugar, urea, creatinine. Liver function test, uric acid and ECG was done in cases of pre-eclampsia. The treating obstretician monitored the uterine contractions and cervical dilatation and effacement every half an hour or when deemed necessary and informed us for the institution of labour analgesia. With the onset of first stage of labour (having regular painful contractions in latent phase) with cervical dilatation of 3-4 cm epidural analgesia was instituted. Group I patients received 10ml of bupivacaine (0.1%) + fentanyl 2µg/ml and Group II received 10ml of ropivacaine (0.1%) + fentanyl 2µg/ml. Pre-anaesthesia evaluation was performed on all the participants and all were administered metoclopramide 0.25mg/kg and ondansetron 0.08-0.1mg/kg by intravenous route as premedication. The baseline heart rate (HR) systolic blood pressure (SBP) and diastolic blood pressure(DBP) were recorded. Intravenous infusion of ringer’s lactate solution was given following which patients were placed in a flexed sitting or lateral position. The epidural space at L2-3 or L3-4 was identified using an18G Touhy’s needle by “loss of resistance to air” technique. An epidural catheter was inserted through the needle and kept at about 4-5cm inside the epidural space and secured. Administration of 10ml of drug (bupivacaine or ropivacaine) in concentrations of 0.1% with fentanyl 2µg/ml was given to achieve T10-L1 sensory level. Top-up doses (bupivacaine in Group I and ropivacaine in Group II) in concentrations of 0.1%with fentanyl 2µg/ml were given after 1 hour of progression of labour or according to parturient demands, whichever was earliest, till the baby’s delivery. The efficacy of the study drugs was assessed using visual analog scale (VAS scale) along with mother’s vitals like HR,SBP, DBP, were measured every 5 min till 30 min then at 60 min and later every hour for six hours. The degree of motor blockade was assessed using a modified Bromage scale (grade I=complete motor blockade-unable to move feet, knees and hip flexion, grade II= able to move feet only, grade III=partial block-just able to move knees, grade IV=detectable weakness in hip flexion but full flexion of knees, grade V =no detectable weakness of hip flexion)and sedation score with four point sedation scale (1=awake, 2=asleep, brisk response to verbal command, 3=asleep, sluggish response to verbal command, 4=deeply sedated) every one hourly after institution of labour analgesia and upto six hours post delivery. Post-delivery APGAR score was assessed at 1, 2, 3 and 5 minutes. Baby was monitored for any respiratory distress or neurological symptoms after delivery. Observation of mother was done for any early complications like itching, rash, bradycardia, hypotension, bronchospasm, retention of urine, fever, as well as late complications like postdural pucture headache (PDPH),backache and any neurological symptoms. Vital monitoring was continued of the parturient regularly for 24 hours post-delivery.
3. STATISTICAL ANALYSIS
The sample size was calculated using R Studio V 1.2.5001 software. The calculated sample size was 23 for both the groups and the power of the study was 90%. Data were analyzed using R Studio V 1.2.5001 software. Categorical variable (cervical dilation, VAS score Bromage score, sedation score) were expressed as mean frequency. Whereas continuous variables (demography) were represented in mean±SD. The Students’t-test and Wilcoxon signed rank test was used to find mean difference between variables such as demography, blood pressure and duration of epidural top-up of both the groups. P<0.05 was considered as statistically significant.
| Demography |
Group I Bupivacaine (mean±SD) |
Group II Ropivacaine (mean±SD) |
P-value |
|---|---|---|---|
| Age (years) | 22.87±3.2 | 22.23±2.5 | 0.6372 |
| Height (cm) | 152.5±5.08 | 151.36±6 | 0.4836 |
| Weight (kg) | 68.06±6.93 | 66.9±6.3 | 0.4964 |
| Gestational age (weeks) | 39.94±0.7 | 39.45±0.78 | 0.0191* |
4. RESULTS
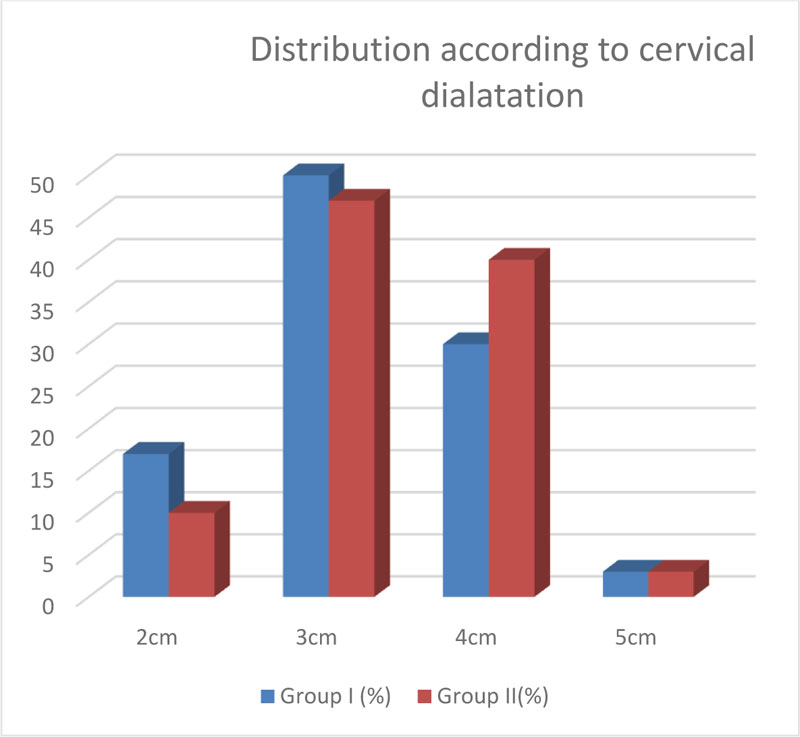
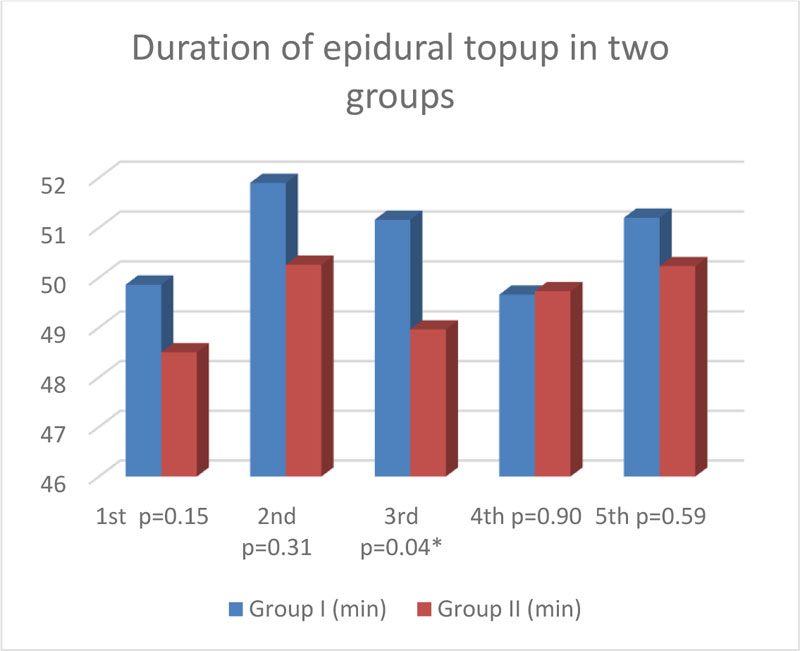
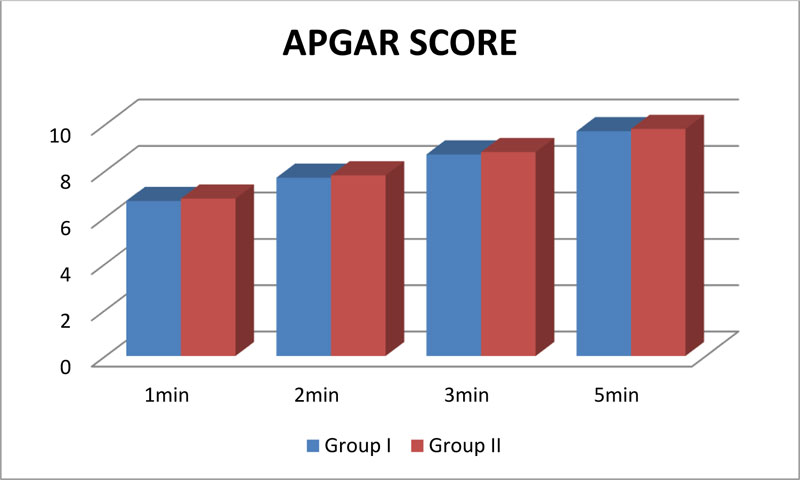
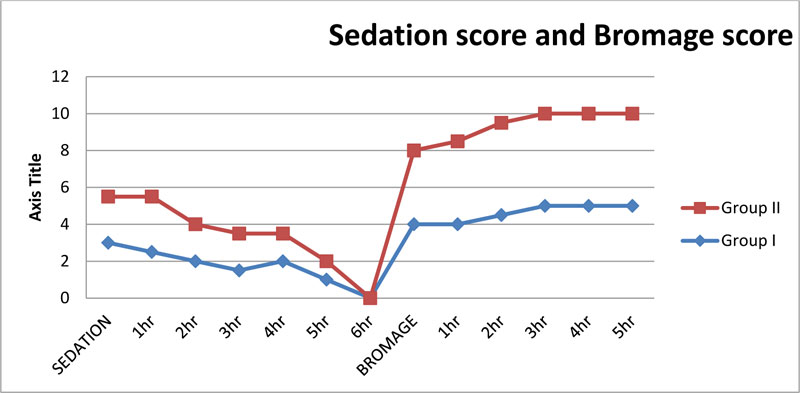
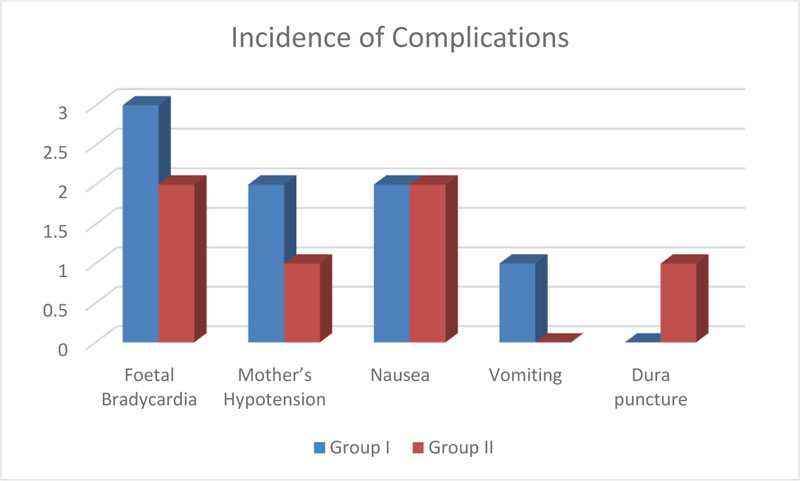
The demographic characteristics of both groups are shown in Table 1. The characteristics like (age, height and weight) were similar in both the group. However, a significant difference was observed in the gestational age of the subjects (P=0.019, P<0.05).In Group I (60%) and Group II (63%) parturients were primigravida. The dilatation of cervix at which labour analgesia was instituted is shown in Fig. (1). 50% parturients in Group I & 37% parturients in Group II had cervical dilatation 3cm. 30% parturients in both groups had cervical dilatation 4 cm. In Groups I and II, no significant difference was observed in systolic blood pressure at all time intervals. However, a statistically significant difference was observed in diastolic blood pressure at 6 hours (360 min) that was less in Group II than in group I(P=0.02) Table 2. Significantly higher heart rate at 30 min (P=0.0003), 120 min (0.006), and 300 min (P=0.001) was observed in Group I subjects when compared with Group II. VAS score was significantly different between the groups at 180 min and 300 min which was lesser in Group II than in Group I. Table 3. Although a statistically significant difference was seen in the 3rd top-up duration but it was clinically insignificant. Time for epidural top-ups is shown in Fig. (2). In Group I, 87%(n=26) of the parturients had normal vaginal delivery, forceps were applied in 7% (n=2) of the cases and caesarean section was required in 7% (n=2) of the cases. In Group II normal vaginal delivery, forceps application and caesarean section were observed in 83% (n=25), 7% (n=2) and 10% (n=3) of the cases, respectively. No significant difference was observed in the APGAR. Scores were taken at one, two, three and five minutes after the birth of the baby in both the groups (P>0.05) Fig. (3). Fig. (4) shows level of sedation (=/ <3) and degree of motor blockade (=/ >grade IV) observed, which was not significantly different when compared between the groups (P>0.05). In Group I, complications such as fetal bradycardia in 10% (n=3) and nausea (6.7% (n=2)) vomiting (3.3%.(n=1)), hypotension were present in 6.67% of the parturient. Complications in Group II included were nausea (6.7%, (n=2)), hypotension (3.7%,(n=2)) and dura puncture (3%,(n=1))in mother and fetal bradycardia in (7%) of the delivered babies. The difference in two groups was not statistically significant (P=0.123367, P>0.05) Dura puncture was not observed in any patients. Fig. (5).
| Time interval |
Systolic blood pressure (In mm of Hg) |
P-value |
Diastolic blood pressure (In mm of Hg) |
P-value | ||
|---|---|---|---|---|---|---|
| Group I | Group II | Group I | Group II | |||
| 0 min | 120.2 | 118.73 | 0.681 | 75.8 | 73.93 | 0.4225 |
| 5 min | 112.2 | 107.26 | 0.2092 | 72.66 | 70.86 | 0.2839 |
| 10 min | 111.53 | 108.6 | 0.484 | 72.33 | 68.73 | 0.07148 |
| 15 min | 114.26 | 109.33 | 0.3439 | 74.36 | 71.93 | 0.2787 |
| 30 min | 114.33 | 108.33 | 0.1629 | 74.13 | 71.6 | 0.2242 |
| 60 min | 111.33 | 106.4 | 0.1298 | 71.4 | 70.66 | 0.8682 |
| 120 min | 111.13 | 106.86 | 0.2358 | 71.93 | 70.33 | 0.2677 |
| 180 min | 112.7 | 106.2 | 0.09353 | 72.73 | 71.53 | 0.6197 |
| 240 min | 110.4 | 105.86 | 0.2182 | 73.2 | 70.33 | 0.08562 |
| 300 min | 109.66 | 105.33 | 0.2339 | 72.93 | 69.73 | 0.1383 |
| 360 min | 109 | 104 | 0.1105 | 70.66 | 68.06 | 0.02057* |
| Time Interval | Heart Rate | P-Value | VAS Score | P-Value | ||
|---|---|---|---|---|---|---|
| Group I | Group II | Group I | Group II | |||
| 0 min | 103.86 | 98.73 | 0.1195 | 9.66 | 9.63 | 0.8213 |
| 5 min | 98.46 | 92.2 | 0.06892 | 6.9 | 6.63 | 0.296 |
| 10 min | 98.73 | 92 | 0.05972 | 2.1 | 2.4 | 0.3163 |
| 15 min | 96.73 | 93.26 | 0.1707 | 1.1 | 1.06 | 0.8655 |
| 30 min | 102.46 | 89.73 | 0.000314*** | 0.83 | 0.7 | 0.6043 |
| 60 min | 96.73 | 94.46 | 0.4204 | 1.13 | 1.16 | 0.8655 |
| 120 min | 102.13 | 92.06 | 0.006593** | 1.56 | 1.43 | 0.6624 |
| 180 min | 95.2 | 93.06 | 0.4823 | 1.7 | 1.2 | 0.01927* |
| 240 min | 96.33 | 95.26 | 0.4418 | 0.96 | 0.9 | 0.8925 |
| 300 min | 104.06 | 92.73 | 0.001216** | 0.6 | 1.26 | 0.01984* |
| 360 min | 98.13 | 93.8 | 0.08038 | 1.5 | 1.6 | 0.6819 |
5 . DISCUSSION
Epidural analgesia is considered as a “Gold standard” technique and commonly accepted procedure for pain relief in labour. The use of epidural drugs such as ropivacaine is increased as it produces fewer cardiovascular complications compared with bupivacaine [9, 10]. The study was conducted to compare the efficacy of ropivacaine-fentanyl and bupivacaine-fentanyl in the alleviation of labour pain. Among studied parturients of both groups, the demographical characteristics such as age, weight, height were similar and most of the parturients of both groups were primigravida. These findings were comparable with previous reports [5, 10]. Tsen et al. concluded that early labour in parturients treated with spinal-epidural analgesia is associated with rapid cervical dilation [11]. The dilation of cervix may be due to decrease in mediators such as PG2α, responsible for uterine activity [12-14]. In this study, most of the cases of both the groups had 3-4cm of cervical dilation. Similar results were found in the study by Chora andHussain [15]. Bupivacaine possess potent cardiotoxicity, while ropivacaine has the advantage of differential sensory and motor blockade, without prominent cardio and neurotoxicity. It also stabilizes hemodynamic with minimal effect on heart rate and blood pressure [16]. An experimental study on rabbits by Bariskaner et al. showed that high doses of bupivacaine (5 and 10 mumol/kg) significantly reduce heart rate, systolic and diastolic blood pressure while 10mumol/kg ropivacaine can produce the same effect hence less cardio- depressant than bupivacaine [17]. This property of ropivacaine ensures the minimal effects on hemodynamic variables along with lesser cardiotoxicity profile as compared to bupivacaine, thus can be considered as agent of choice in patients with cardiovascular compromise /comorbidities so also in parturients especially with preeclampsia. In many previous reports, no difference was observed in systolic and diastolic blood pressure of parturients treated with ropivacaine and bupivacaine [5, 10, 15, 18]. In contrast, the study of Yadav and Jaiswal showed a significant difference in systolic blood pressure at 12 and 24-hour post anaesthesia wherein bupivacaine and fentanyl treated subjects significant decrease in diastolic blood pressure was observed at 15min, 30 min, 1hr, 2hr, 6hr, 12hr, and 24hr [19]. In our study, no significant difference was found in systolic blood pressure in both groups. However, a significant decrease in diastolic blood pressure was seen in Group II cases (P=0.020) when compared with Group I. The fluctuating values of blood pressure may be due to variations in the dose of drugs used and the time of blood pressure monitoring. Comparative studies with different volumes and concentrations of drugs such as 2ml 0.125% drug (bupivacaine or ropivacaine) with 5µg of fentanyl (2ml+0.125%+5µg), 20ml+0.125%+50µg, and 3ml+0.125 %+2µg showed no difference in heart rates [5, 10, 18]. In a study, 10ml 0.1% of drug with 2µg of fentanyl showed a significant difference in heart rates of parturients. Pain scores in bupivacaine and ropivacaine (0.1%) treated subjects in the first and second stages of labour showed comparable levels of analgesia [20]. In contrast with these findings, a significant difference was seen in VAS scores of both groups at 180 and 300 min with ropivacaine demonstrating better efficacy at 180 minutes and at 300 minutes. Bolus on-demand epidural doses may be the reason for lower VAS scores in patients. In this study, no significant difference in bolus requirement in both groups except 3rd top-up suggests equal efficacy in both groups. Similar results were shown by the study of Bawdaneet et al. using the same doses of the drugs [20]. Rate of vaginal delivery may get influenced by the type of epidural analgesia [10]. A combination of local anaesthetics with lower doses of opioids resulted in lower rates of instrumental deliveries [21, 22]. Chetty et al. in their study evaluated 0.125% vs 0.2% ropivacaine for epidural labor analgesia regarding sensory and motor block characteristics and found comparable maternal expulsive efforts, instrumental delivery and fetal outcome in both the groups [23]. Chethananand et al. evaluated efficacy of 0.0625% racemic bupivacaine and 0.1% of ropivacaine with 2 μg/ml of fentanyl and observed no significant difference in maternal satisfaction, mode of delivery, incidence of instrumentation and fetal outcome in two groups [24]. Thus studies by Chetty et al. and Chethananand et al. observed lesser incidences of instrumental deliveries and LSCS with 0.1%, 0.125%, 0.2% of ropivacaine and 0.625% of bupivacaine. Whereas, the study of Halpern et al. showed that bupivacaine was associated with an increased rate of motor block but the rate of spontaneous vaginal delivery was similar regardless of anaesthetic drug used. [25]. In our study, the rate of normal vaginal delivery was similar in both groups. There were no motor blockade instances in either group, possibly due to limited concentrations of anaesthetics used and these findings are similar to the study by Gündüz et al. [10] High rates of spontaneous delivery without incidence of motor blockade, may be due to low and titrated concentrations of the drug and the addition of opioids [10]. In both, the group incidences of adverse effects such as foetal bradycardia, nausea vomiting, sedation and hypotension were observed but similar which may be due to the use of opioids. The performance of bupivacaine and ropivacaine (0.1%) was found to be clinically very similar. There were no significant differences in pain score, sedation scores, motor blockade, blood pressure, mode of delivery and side effects. However, significant differences were found in heart rates at different time intervals. Limitations of the study are small sample sized. There is a need to add more cases to confirm the findings of our study statistically.
CONCLUSION
From our study we conclude that bupivacaine and ropivacaine were comparable in terms of quality of analgesia, hemodynamic stability, degree of motor blockade, requirement of top-up doses, incidence of instrumental delivery and side effects. Considering the safety profile and characteristic differential blockade, ropivacaine can be considered as a better alternative to bupivacaine for labour epidural analgesia.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This prospective randomized study was performed at a tertiary care centre in Kolhapur, India, after approval by the Institutional Ethics and Review board (DYPMCK/PG-14/1721/15-16).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All patients participated on a voluntary basis and gave their informed consent.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We acknowledge the support of Department of Obstetrics and Gynaecology for directing cases for this study, providing data and help in analysis for the preparation of the manuscript.


