All published articles of this journal are available on ScienceDirect.
The Effect of Fiberoptic Bronchoscopy-guided Technique for Placement of a Left-sided Double-lumen Tube on the Intubation Performance Compared with the Conventional Method Using a Macintosh Laryngoscope
Abstract
Background:
The accurate placement of the double-lumen endotracheal tube is imperative for effective one-lung ventilation in thoracic surgery. Malpositioning and repositioning of a misplaced tube may cause excessive trauma.
Objective:
We hypothesized that the fiberoptic bronchoscope-guided method for double-lumen endotracheal tube placement would reduce the incidence of malpositioning as compared to the conventional method using the Macintosh laryngoscope.
Methods:
Fifty patients scheduled to undergo elective thoracic surgery were recruited and randomly assigned to the fiberoptic bronchoscope-guided [n=25; Group F] and conventional [n=25; Group C] method groups, according to the method of double-lumen endotracheal tube placement. The primary outcome was the incidence of double-lumen endotracheal tube malpositioning observed under the fiberoptic bronchoscope after initial placement. Secondary outcomes included the times for placement, confirmation, and total procedure of double-lumen endotracheal tube intubation.
Results:
The incidence of malpositioning after initial double-lumen endotracheal tube placement was significantly lower in Group F than in Group C (20.0% vs 68.0%). In addition, the time for placement was significantly higher in Group F than in Group C, and that for confirmation was significantly lower in Group F than in Group C.
Conclusion:
The fiberoptic bronchoscope-guided method for double-lumen endotracheal tube placement can reduce the incidence of malpositioning after initial placement and expedite the intubation process with a double-lumen endotracheal tube in thoracic surgery.
1. INTRODUCTION
Proper placement of a left-sided Double-Lumen endotracheal Tube (DLT) within the Left Mainstem Bronchus (LMB) is imperative for appropriate tube functioning and allows the operative lung to collapse while providing excellent visualization of the surgical field for thoracic surgeons [1, 2]. However, previous papers reported a relatively high incidence of DLT misplacement (32%-83%) immediately after blind intubation [3-5]. Even in the studies reporting a lower rate, clinical confirmation techniques, such as inspection and auscultation, missed a significant number of DLT malpositioning cases [6-8], which could critically affect both the patients’ safety and surgical outcomes. In addition to malpositioning per se, the repeated action of repositioning the misplaced tube could injure the airway, and increased manipulation of the DLT in the bronchus may also lead to excessive trauma [5].
In current anesthetic practice, visual confirmation of correct DLT placement by using a Fiberoptic Bronchoscope (FOB) is considered the gold standard and, therefore, an FOB has been considered as an essential tool for the thoracic anesthesiologist [1, 4, 9]. If the FOB is routinely used in thoracic surgery for checking the DLT position, DLT placement under the initial guidance of an FOB may be a useful option for achieving appropriate intubation with a DLT. Recently, several works focusing on DLT intubation have reported the usefulness of various Videolaryngoscope (VL) types compared with Macintosh laryngoscope [10-12]. Interestingly, a recent meta-analysis reviewing these studies showed that VL has unfavorable results compared to Macintosh laryngoscope in terms of DLT malpositioning incidence. Especially, VL resulted in difficulty in advancing the DLT past the vocal cords, and a sequential rotation maneuver to overcome difficulty may have increased the incidence of malpositioning [10, 12]. In addition, the improvement of view, which is the advantage of VL, is effective up to the glottis level and, therefore, FOB is considered to be more suitable than VL as equipment capable of taking responsibility for a definite view under the glottis level. Therefore, we intended to compare FOB and Macintosh laryngoscope by focusing on an aspect of DLT malpositioning.
However, only two randomized controlled studies have compared FOB guidance for DLT placement during intubation with the conventional method for DLT intubation [13, 14]. In both studies, even the FOB-guided technique used the conventional direct laryngoscopy during insertion of the DLT into the trachea, and FOB guidance was only used when advancing the DLT into the LMB [13, 14]. Unlike the existing FOB-guided technique described in the two previous studies, we designed an FOB-guided method in which tracheal intubation was performed under initial FOB guidance via the bronchial lumen with subsequent selective left bronchial intubation. Then, we hypothesized that this method would guarantee definite placement of the bronchial tip of the DLT within the LMB and ensure less frequent malpositioning of the DLT, in comparison with the conventional intubation method. Thus, this process was also expected to reduce the time required to confirm and correct the position of the DLT, thereby expediting the entire process of DLT intubation. To date, no previous randomized trials have been reported using the method we designed.
Therefore, in this study, we aimed to compare the two DLT placement methods our FOB-guided method and conventional intubation method using a Macintosh laryngoscope in terms of the incidence of DLT malpositioning and their impact on the time required to achieve DLT intubation.
2. MATERIALS AND METHODS
This prospective, single-center, single-blind (participant), randomized, controlled pilot trial was conducted in a tertiary university hospital from January to April 2018. The trial was approved by the Institutional Review Board of Daegu Catholic University Medical Center (CR-17-177-L, December 2017), and the protocol was registered at cris.nik.go.kr (KCT0002663) and published [15]. Informed consent was obtained in writing from all participating patients during preoperative visits.
Fifty patients aged 18-70 years with an American Society of Anesthesiologists physical status of 1 or 2 who were scheduled to undergo elective thoracic surgery requiring a left-sided DLT were enrolled in this study. Patients were excluded if they met one of the following criteria: (1) required a right-sided DLT; (2) showed an intraluminal lesion in the LMB; (3) showed an anatomical problem in the tracheobronchial tree on chest radiography; (4) had a body mass index greater than 30 kg/m2; (5) showed limited neck motion; (6) had reduced mouth opening (less than 3 cm); (7) showed a poor dental status; (8) had Mallampati class IV (soft palate not visible at all while sitting up straight, mouth open, and tongue maximally protruded) [16]. Equal numbers of eligible patients were randomly allocated to the conventional method group (Group C) or the FOB-guided method group (Group F) using random numbers generated by Microsoft Excel 2010 (Microsoft Corp., Redmond, WA, USA). The patients were blinded to their group allocation, which was concealed in an opaque envelope and managed by an anesthesia nurse who was not involved in the perioperative care. Immediately before induction of anesthesia, an anesthesiologist opened the sealed envelope and prepared the intervention technique as indicated. However, the investigators could not be blinded to the patients’ group allocations because the intubation methods in the two groups were obviously different.
2.1. Anesthesia Protocol
All patients received midazolam 0.05 mg/kg intramuscularly 30 minutes before induction of anesthesia. On arrival in the operating room, standard monitoring, including electrocardiography, non-invasive blood pressure measurement, and pulse oximetry, were applied. A disposable bispectral index sensor (BIS™, Aspect Medical Systems, Newton, MA, USA) was used to monitor the depth of anesthesia. Anesthesia was induced and maintained with propofol and remifentanil using target-controlled infusion (Orchestra® Base Primea; Fresenius Kabi, France) based on bispectral index monitoring of the depth of anesthesia, and rocuronium 0.8 mg/kg was administered for tracheal intubation. A disposable polyvinyl chloride left-sided DLT (Broncho-Cath®, Mallinckrodt Medical Ltd., Athlone, Ireland) was used to allow the One-Lung Ventilation (OLV) for thoracic surgery. The size of the DLT was chosen according to patients’ LMB diameters, which were measured by chest Computed Tomographic (CT) scanning [17].
2.2. DLT Intubation Protocol
In both groups, the patient’s head was placed in a sniffing position and the laryngeal view was graded under direct laryngoscopy by using a Macintosh laryngoscope according to the modified Cormack-Lehane (C/L) classification [18]. The best laryngeal view, obtained with or without the BURP (backward, upward, rightward pressure) maneuver, was recorded. In our study, a C/L grade 1 and 2a denoted an “easy laryngoscopy” and grades 2b, 3, and 4 denoted a “difficult laryngoscopy.” All tracheal intubations were performed with a left-sided DLT by either the conventional method or the FOB-guided method. In both groups, all these intubation processes, which were collectively termed DLT placement, were followed by subsequent confirmation processes performed by the same anesthesiologist to determine whether the DLT was positioned optimally within the LMB.
In Group C, the DLT was preformed over the stylet and bent to approximately 90 degrees at the point of the tracheal balloon. The bronchial tip of the DLT passed beyond the vocal cords under direct laryngoscopy, after which the stylet was removed. The DLT was rotated 90 degrees to the left and then advanced until slight resistance was encountered. Successful endotracheal intubation was confirmed by a capnography curve. The subsequent confirmation processes were performed using an FOB to identify three sequential points [1], which are described as follows. First, when the FOB was passed through the tracheal lumen of the DLT, an unobstructed view of the Right Mainstem Bronchus (RMB) should be identified and the fully inflated blue-colored bronchial cuff should be positioned below the carina without herniation. Second, when the FOB was advanced further into the RMB, an unobstructed view of the right upper bronchus with the three segments should be identified. Third, when the FOB was introduced into the LMB via the bronchial lumen of the DLT, an unobstructed view of the left upper and lower bronchi should be verified.
In Group F, an FOB was prepared and passed through the bronchial lumen of the DLT in advance. After grading the laryngeal view under direct laryngoscopy according to the modified C/L classification, an anesthesiologist introduced the FOB into the patient’s mouth while standing at the head of the bed, while a jaw-thrust maneuver was applied to provide sufficient space for FOB passage by an experienced assistant anesthesia nurse. When positioning the FOB in the midline of the pharynx during advancement, the tip was angulated up and down to direct it toward the glottis opening and advanced through the vocal cord. Once it entered the trachea, the FOB was advanced further into the LMB and the previously loaded DLT was inserted into the LMB, guided by the FOB, with the maintenance of jaw-thrust. During withdrawal of the FOB through the bronchial lumen, the position of the DLT was checked and corrected to ensure that the bronchial cuff was not advanced beyond the secondary carina, similar to the third point in the conventional method described previously. When the bronchial tip was approximately 1 cm above the secondary carina, it was considered as the proper position. Because the third point of the conventional method could be omitted in Group F, the confirmation process was performed using an FOB to identify only two sequential points that could be checked through the tracheal lumen of the DLT: an unobstructed view of the RMB, the bronchial cuff positioned below the carina without herniation, and an unobstructed view of the right upper bronchus with the three segments should be verified.
Malpositioning, which can be detected when the FOB is passed via the tracheal lumen first after the placement of the DLT, may manifest as three situations [19]: (1) the bronchial cuff herniation is discovered; (2) the bronchial balloon is not visible under FOB and the DLT is suspected to be advanced more distally than usual into the left bronchus; (3) the tracheal lumen view is obstructed and the carina and the distinctive orifices of the three segments of the right upper lobe could not be recognized, and the displacement of the DLT into the RMB is suspected. In these situations, the DLT has to be repositioned. To summarize the two principles of the repositioning process, when the DLT needs to be advanced more deeply into the LMB while observing via the tracheal lumen or withdrawn while observing via the bronchial lumen, its position should always be rechecked through the opposite tracheal or bronchial lumen. If the DLT was repositioned while observing via the bronchial lumen (as in the FOB-guided technique), only two points should be rechecked through the opposite tracheal lumen (as in Group F), even in Group C. Since we aimed to investigate which method would expedite the entire process of DLT intubation, the anesthesiologist performing the DLT intubation aimed to reduce the time taken for the placement and confirmation without wasting time unnecessarily but also without missing key processes. In both groups, after placing the DLT and before confirming the position, the DLT was fixed temporarily and mechanical ventilation was started. After verifying the proper position of the DLT within the LMB, the DLT was fixed firmly at the patient’s mouth using tape. The interventions, including placement and confirmation (or correction if necessary), were performed by two experienced anesthesiologists who were skilled in the use of both a conventional laryngoscope and an FOB, and had more than five years of experience.
2.3. Outcome Variables
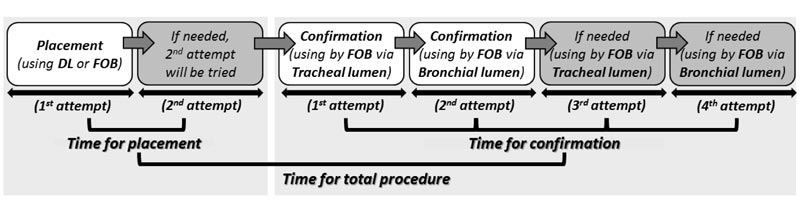
The primary outcome was the incidence of DLT malpositioning, including herniation of the bronchial cuff over the tracheal carina, more distal advancement into the LMB than usual, or misplacement into the RMB in FOB observation via the tracheal lumen after initial placement of the DLT. The secondary outcomes included the time variables, which were defined as follows (Fig. 1). The total procedure time was defined as the time required to perform the entire process of intubation using a left-sided DLT, which was the sum of the times for placement and confirmation. The time for placement was the time from insertion of the laryngoscope blade or FOB tip into the patients’ mouth to the removal of these devices from the mouth during DLT placement within the LMB. The time for confirmation was defined as the sum of the duration between FOB insertion and its removal through the elbow connector of the DLT during each attempt for confirmation of proper DLT positioning. Up to two tracheal intubation attempts were allowed with the assigned technique. If the second attempt also failed, subsequent attempts were performed at the discretion of the anesthesiologist using other devices required for successful intubation after a few minutes’ mask ventilation. The duration of each attempt was aggregated to determine the time for placement. All these time points were recorded by an assistant anesthesiologist. Failed tracheal intubation on the first and second attempt and complications of the intubation process, such as injuries of the lip, teeth, or oropharyngeal tissues, were also recorded as secondary outcomes.
2.4. Statistical Analysis
The sample size was not calculated statistically because this study was designed as a pilot study, and a total of 50 patients was arbitrarily targeted. There are several guidelines for choosing an appropriate sample size for a pilot study; however, recent work has shown that at least 50 participants are recommended for a pilot study [20]. The Kolmogorov-Smirnov test was used to determine the normality of the distribution of data. Normally distributed data were expressed as mean ± standard deviation values and analyzed by an independent Student’s t-test. Non-normally distributed data were presented as median (range) and analyzed using a Mann-Whitney U-test. Categorical data were expressed as the number of patients (percentage) and analyzed using the Chi-squared test or Fisher’s exact test. All comparisons were two-sided and p-values <0.05 were considered to be statistically significant. Statistical analyses were performed using IBM SPSS Statistics version 19.0.0 (IBM Corp., Armonk, NY, USA).
3. RESULTS
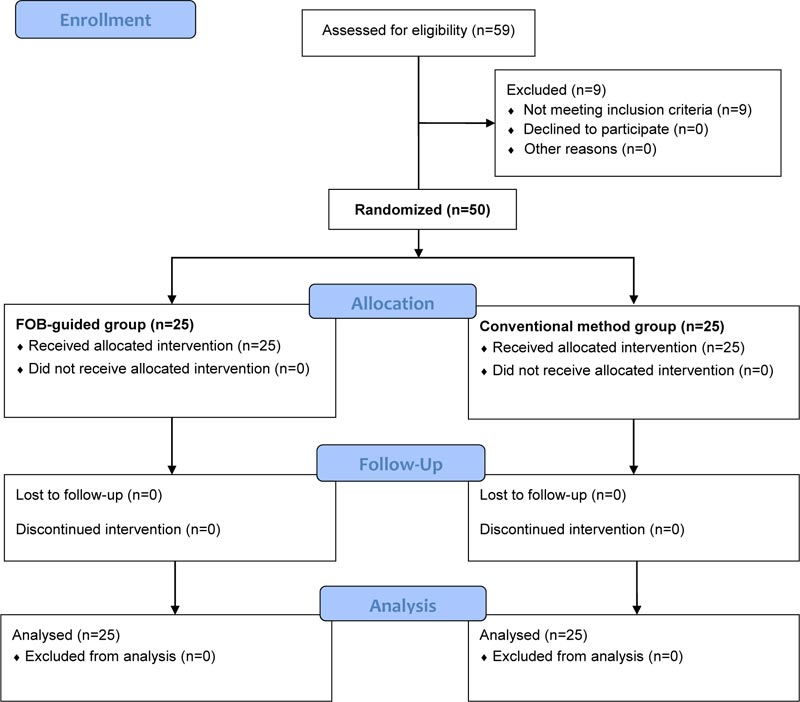
Fifty patients scheduled to undergo elective thoracic surgery between January and April 2018 participated in this study, and none of these patients were excluded from the analysis (Fig. 2). No significant intergroup differences were noted in patient demographic characteristics (Table 1).
With respect to the primary outcome, the incidence of DLT malpositioning just after tube placement was significantly lower in the Group F than in the Group C (20.0% [5/25] vs. 68.0% [15/25], odds ratio [95% confidence interval]: 0.118 [0.032–0.428]; p=0.001; Table 2). The major cause of malpositioning was more distal advancement into the LMB in Group C (12 of 17 patients; 70.6%) and herniation of the bronchial balloon over the tracheal carina in Group F (4 of 5 patients; 80.0%).
The total procedure time was slightly shorter in Group F than in Group C, although the difference was not significant (p=0.12). In Group F, the time for placement was significantly higher (p<0.001), but the time for confirmation was significantly shorter than that in Group C (p<0.001) (Table 2).
Although tracheal intubation was successfully performed at the first attempt in all patients in Group C, the first attempt failed in one patient in Group F because of the difficulty in inserting the DLT into the trachea over the FOB. However, in this patient, the DLT showed proper positioning immediately after successful intubation and the time required for confirmation was only 18s; thus, although the time required for placement was 63s, the time for the total procedure was only 81s.
No patient in either group experienced lip or teeth injury, while oropharyngeal injuries occurred in one patient in Group C and two patients in Group F. The incidences of such complications showed no significant intergroup differences (p=1.000).
| - | FOB-guided Group (n=25) |
Conventional Group (n=25) |
P-value |
|---|---|---|---|
| Sex (M/F) | 19/6 | 17/8 | 0.529 |
| Age (years) | 45.2 (21.9) | 47.4 (19.5) | 0.704 |
| Weight (kg) | 59.9 (10.2) | 61.9 (11.4) | 0.525 |
| Height (cm) | 169.5 (8.1) | 167.8 (8.5) | 0.482 |
| BMI (kg/m2) | 20.9 (3.6) | 22.0 (3.6) | 0.295 |
| Mallampati classification (1 or 2/3) | 22/3 | 24/1 | 0.609 |
| Modified Cormack-Lehane grade (1/2a/2b/3/4) |
10/10/2/3/0 | 7/15/3/0/0 | 0.193 |
| Laryngoscopy difficulty (Easy/Difficult) | 20/5 | 22/3 | 0.702 |
| Type of surgery (lobectomy/wedge resection /mediastinal mass excision) |
5/16/4 | 6/15/4 | 0.606 |
| - | FOB-guided Group (n=25) |
Conventional Group (n=25) |
p-value | |
|---|---|---|---|---|
| DLT malposition | 5 (20%) | 17 (68%) | 0.001 | |
| Herniation over the tracheal carina | 4 | 3 | - | |
| Advancement distally into the LMB | 1 | 12 | - | |
| Advancement into the RMB | 0 | 2 | - | |
| Failed intubation | - | - | - | |
| on first attempt | 1 (4%) | 0 (0%) | 0.312 | |
| on second attempt | 0 (0%) | 0 (0%) | 1.000 | |
| Time for total procedure (s) | 48 (36-99) | 62 (38-86) | 0.091 | |
| Time for placement (s) | 26 (21-63) | 15 (12-23) | <0.001 | |
| Time for confirmation (s) | 20 (13-60) | 43 (23-71) | <0.001 | |
4. DISCUSSION
Our study showed that in comparison with the conventional method performed using a Macintosh laryngoscope, the FOB-guided method could reduce the incidence of DLT malpositioning observed via the FOB during the confirmation process after initial DLT placement. This result could help reduce the number of attempts made to reposition the DLT and reconfirm its position, thereby significantly reducing the time required for the confirmation process.
The FOB-guided method offered another advantage in that it could essentially prevent misplacement towards the RMB since it was designed to definitely guide the DLT into the LMB. In fact, no patient in Group F showed misplacement into the RMB, whereas two patients in Group C showed malpositioning into the RMB and required three attempts for the confirmation process, making this the most time-consuming issue with respect to the total time required for confirmation (Table 3). A higher number of confirmation attempts imply a longer procedure time. Confirmation attempts could be performed only once in Group F, but two attempts were required in Group C, and the total duration of the confirmation process was lower in Group F than in Group C.
There was a discrepancy in the criteria used to describe DLT malpositioning between the two methods, i.e., the criterion “advancement more distally into LMB” seemed to be stricter in Group C than in Group F. The conventional method could not assure that the DLT was properly placed within the LMB, unless the actual depth was checked via the bronchial lumen. Therefore, we decided to consider lack of visibility of the bronchial cuff via the tracheal lumen as a sign of excessively deep advancement in Group C and withdrew the DLT until the bronchial cuff was visualized just below the carina in such cases in Group C. This strategy is expected to be more efficient than keeping the DLT in place without withdrawal, even though the DLT might not be actually beyond the secondary carina in some cases with an invisible bronchial cuff. This is because keeping the DLT in place might be problematic in cases with actual “advancement more distally beyond the secondary carina.” In contrast, the FOB-guided method always ensured that the DLT position was definitely not in the position of advancement beyond carina during the placement process; thus, the DLT position could be confirmed as proper regardless of the visibility of the bronchial cuff.
The choice of an appropriately sized DLT has been a matter of debate, and the size of the DLT could influence tube placement within the LMB. A relatively smaller DLT for the size of the airway is likely to be placed deeply into the bronchus [21, 22], whereas a larger DLT is relatively difficult to intubate, and both excessively large and small DLTs have the potential to cause airway injury [23]. Given that it is generally recommended to use the largest DLT that can be atraumatically advanced into the bronchus [24], we determined the size of the DLT according to the LMB diameter measured on chest CT. However, CT measurements cannot completely prevent the possibility of selecting an incorrectly sized DLT because the real sizes may differ from the CT measurements and the external diameter may be inconsistent even in DLTs of the same size [25]. When using the conventional method with a slightly smaller DLT, such inevitable limitations should be considered, although a slightly larger DLT can enter and fit the bronchus due to the elasticity of the bronchi rather than causing problems with DLT malpositioning. In contrast, the FOB-guided method can guarantee appropriate DLT positioning and, therefore, would not cause the malpositioning associated with slightly inappropriately sized DLTs.
Although the FOB-guided method showed these benefits, the time required for DLT placement when using the FOB was significantly longer than that with the conventional method. Even in comparisons of patients successfully intubated on the first attempt, the median (range) time for placement in Group F was also significantly longer than that in Group C (26 (21-40) s vs. 15 (12-23) s; p < 0.001). This unfavorable characteristic of the FOB-guided method was attributed to the possibility that manipulation of the FOB may not be as familiar as that of a Macintosh laryngoscope, and the process could be especially much more challenging for novice physicians. Identification of the vocal cord through a narrow oropharyngeal route under the FOB view and introduction of the FOB into the trachea at an appropriate angle could be difficult unless the operators and assistants had sufficient experience and training. Even with the successful entry of the FOB into the trachea, the advancement of the tube over the FOB in the next step could be complicated by several factors [26]. The DLT is larger and stiffer than a conventional endotracheal tube, and it could be more difficult to achieve successful advancement of the DLT beyond the vocal cord. For these reasons, the first attempt to perform tracheal intubation actually failed in one patient in Group F. To overcome these difficulties, studies have suggested methods such as reducing the gap between the tube and FOB [26] or performing a jaw-thrust properly [27-29]. In the present study, we used a 3.5 mm FOB and 35, 37, or a few 39-Fr DLTs (inner diameter of the bronchial lumen: 4.3, 4.5, or 4.9 mm, respectively), and we intended to avoid using extremely large DLTs (41 Fr) to minimize the gap between them. Using the jaw-thrust maneuver properly to maintain the width of the oropharyngeal cavity and opening the laryngeal inlet helped rescue the patient in whom the first attempt failed. Because of these difficulties in FOB manipulation, the FOB-guided method should be performed after gaining sufficient experience and practicing coordination between the operator and assistant in easy cases. In our study, the significantly longer time for placement with the FOB could be offset by the time reductions in the confirmation process, and the findings suggested that the FOB-guided method may be suitable for DLT intubation.
| - | Time for Confirmation (s) | Number of Cases |
|---|---|---|
| FOB-guided Group | - | n=25 |
| Herniation over the tracheal carina | 52.5 (34-60) | 4 |
| Advancement distally into the LMB | 44 | 1 |
| Advancement into the RMB | - | 0 |
| Proper position | 18.5 (13-30) | 20 |
| Conventional Group | - | n=25 |
| Herniation over the tracheal carina | 48 (37-54) | 3 |
| Advancement distally into the LMB | 52.5 (34-63) | 12 |
| Advancement into the RMB | 68.0 (65-71) | 2 |
| Proper position | 27 (23-40) | 8 |
There were some limitations in our study. First, researchers who performed the intervention, including placement and confirmation, were not blinded to the group allocation. Moreover, another factor was the skill level of the clinicians performing the intervention. When placing DLT using the FOB-guided technique or checking the DLT malpositioning using FOB, the researchers who were not familiar with this process could have influenced the results of this study. Therefore, in this work, both methods were performed by two experts and a standardized protocol was made to minimize these human factors. Secondly, several factors that could cause airway difficulty were excluded from our study. This was because the difficulty factor included situations where the intervention of the control group involving the conventional laryngoscope could not even be applied (e.g., limited mouth opening or poor dental status) or could not be used alone. For investigating the usefulness of the FOB-guided method depending on the patients’ airway status, it is necessary to analyze the patients classified in more detail using various factors for airway difficulty. The sample size of the present study was insufficient to analyze subgroups according to airway difficulty classified according to modified C/L classification. Third, DLT displacement often occurs during lateral positioning, and our study did not include the period after completion of DLT intubation. Although we focused on the events during DLT intubation and aimed to determine which method was better in reducing malpositioning during the study period, additional strategies would be required to resolve the additional malpositioning that could have occurred after the study period. However, increased DLT manipulation in the bronchus for repositioning the malpositioned DLT may cause excessive trauma and time-wasting [5], and the reduction of these unnecessary actions during the intubation period can reduce the burden of the entire period of operation. This may be helpful not only in preventing excessive injuries but also in decreasing the delay in surgery preparation [5]. Finally, our study did not include the postoperative period and it did not compare postoperative complications such as sore throat between two groups because of the wide variation in the procedure durations of patients undergoing Video-Assisted Thoracoscopic Surgery (VATS) lobectomy in our institution and the influence of these variations on the postoperative outcome. Further trials are required to compare the postoperative outcomes between the two methods using patient groups treated under identical conditions.
CONCLUSION
In conclusion, in comparison with the conventional method using a Macintosh laryngoscope, our FOB-guided method for DLT placement could reduce the incidence of DLT malpositioning after initial placement and the time required to confirm and adjust the position of the DLT. In addition, the time required to perform the entire process of DLT intubation can be expedited using this method, although there was no significant difference between the two methods. Therefore, this method can be a useful option for achieving DLT intubation and is expected to be beneficial, especially in patients who need to avoid multiple movements of the tube or in a busy operating-room setting.
LIST OF ABBREVIATIONS
| BURP | = Backward, Upward, Rightward Pressure |
| C/L | = Cormack-Lehane |
| CT | = Computed Tomography |
| DLT | = Double-Lumen endotracheal Tube |
| FOB | = Fiberoptic Bronchoscope |
| LMB | = Left Mainstem Bronchus |
| OLV | = One-Lung Ventilation |
| RMB | = Right Mainstem Bronchus |
| VATS | = Video-Assisted Thoracoscopic Surgery |
| VL | = Videolaryngoscope |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The trial was approved by the Institutional Review Board of Daegu Catholic University Medical Center, South Korea (CR-17-177-L, December 2017) and registered at cris.nik.go.kr (KCT0002663).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All patients participated on a voluntary basis and gave their informed consent.
AVAILABILITY OF DATA AND MATERIALS
The data used to support the findings of this study are available from the corresponding author [S.H.B.] upon request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


