All published articles of this journal are available on ScienceDirect.
Correlation between Antibiotic Consumption and Hand Hygiene Compliance Among Anesthesia and Intensive Care Healthcare Professionals
Abstract
Aims:
The aim of this study was to investigate the correct use of gloves and alcohol-based products for hand hygiene and identify opportunities for hand hygiene replacement with gloves among healthcare professionals working in the Department of Anesthesia and Intensive Care of a tertiary care University Hospital.
Background:
Two centuries have passed since the discovery of Semmelweis that the “puerperal fever” was due to an infection transmitted by the hands. Currently the hand hygiene is still not well performed, rather it is often replaced by the improper use of gloves. Microbial transmission is estimated to occur in one-fifth of all contact cases.
Objective:
To investigate the correct use of gloves and alcohol-based products for hand hygiene and identify opportunities for hand hygiene replacement with gloves among healthcare professionals. Furthermore, to correlate the consumption data of the hydroalcoholic solution and the amount of antibiotics used for the treatment of hospital-acquired infections.
Method:
The study was conducted over six months period (from January to June 2018); during this period, 20 monitoring sessions were performed. The following indicators were evaluated: a) Non-adherence to hand hygiene with concomitant use of gloves; b) Adhesion to alcoholic friction of hands; c) Hand-washing adhesion. Instead, the consumption data, provided by the hospital ward itself, were used for the evaluation of d) The antibiotics used in the treatment of hospital-acquired infections; e) The hydro-alcoholic solution used by the healthcare professionals for hand hygiene.
Results:
The frequency of non-adherence to hand hygiene was very high at the beginning of the study, subsequently it decreased to about a half percent to that at the initial stage. The adhesion to alcoholic friction of hands increased during the study period. Otherwise, the hand-washing adhesion slightly reduced, especially in March probably due to the recruitment of new inadequately trained nursing staff. The trend of antibiotic consumption was similar to handwashing. The consumption of hydro-alcoholic solution was very low, however over time, it increased considerably until the end of the study.
Conclusion:
In light of the findings from this work, it is necessary to make the hospital staff increasingly aware of the correct practice of hand hygiene and to organize training and informative sessions to promote the health of the individual and the community.
1. INTRODUCTION
For a long time, washing hands with soap and water was the only measure of hygiene not only for personal use but also for public health. Beginning in the nineteenth century, there was awareness that the use of antiseptic agents in health care institutions for hand cleaning could prevent the transmission of pathogens. In the middle of the last century, the Hungarian doctor Semmelweis noted that the “puerperal fever” with its associated high mortality rate was due to an infection transmitted by the hands of medical students who went directly from the autopsy tables to women giving birth without washing their hands. Semmelweis, therefore, introduced a scrupulous protocol for handwashing and disinfection with calcium hypochlorite and the mortality rate of 25% was reduced to 1% over several years [1]. Almost two centuries have passed since the discovery of Semmelweis, and in the meantime, the processes of sterilization of the materials and disinfection of the hands have undergone a remarkable evolution. In 1961, the US Health Service produced and distributed a training video concerning the correct procedure for hand hygiene. The video noted the correct indications for scrupulous handwashing with soap and water, limiting the use of antiseptic agents instead only in cases of emergency or for use in areas without running water and washbasins. In 1995, the Association for Infection Control (APIC) published guidelines for washing and antisepsis of the hands in which it was stressed that washing with water and natural soap carries out only a mechanical removal of microorganisms, within certain levels, towards microbes, while it is necessary to use an antiseptic product to inactivate or kill the microorganisms [2]. Also in 1995 and then in 1996, the Center for Disease Control and Prevention (CDC) and the Advisory Committee on Health Infection Control Practices (HICPAC) recommended the use of both antimicrobial soap and antiseptics for the cleansing of the hands after the treatment of patients infected by multiple drug-resistant bacteria (MDR) [3]. More recently, the CDC and HICPAC stated that hand friction with alcohol-based products is the standard for sanitary hand hygiene practices. Although the aforementioned guidelines have been adopted in most hospitals, many health professionals still do not pay attention to hand-washing practices [4]. Therefore, the spread of diseases related to the hospitalization of patients continues to be a problem affecting public health with a consequent impact on both public health and economics [5, 6]. The European Center for Disease Prevention and Control (ECDC) in 2008 estimated that in Europe, the number of people with hospital-acquired infection (HAI) is increasing and as a result, there are about 37,000 deaths directly due to HAI and around 110,000 indirectly caused by them [7]. In 2009, the World Health Organization (WHO) published the Guidelines for hand hygiene which contain recommendations for proper hand hygiene and which focus on the five main moments in which the hygiene of the hands is essential in hospitals: before contact with the patient, before an aseptic maneuver/procedure, after exposure to a body fluid, after touching a patient and after touching everything that surrounds a patient [8]. The APIC guidelines also focus on the use of gloves as a barrier to contaminating microorganisms. The quality of the gloves was also evaluated based on the material they are made of (e.g., latex, vinyl) and the benefits noted for ‘double gloving’ [2]. But above all, it is known that the improper use of gloves or an error during their change can be a vehicle of contamination [2]. As part of the “Choosing Wisely” project promoted by Slow Medicine in collaboration with the National Association of Hospital Management Doctors (ANMDO) and with the Italian Hygiene Society (SItI), a report describing the 5 practices deemed at risk of appropriateness, including the improper use of gloves was published. It clarified that the use of gloves is the first and the most important preventive measure against the transmission of microorganisms, but this does not completely eliminate the need to wash hands since the gloves could have small defects not visible to the naked eye or tear during the change, this is why the use of gloves is included in the list of five practices to be monitored. Moreover, linked to the practice of wearing gloves, there is also the use of alcohol-based products. These assist in handwashing and, for the most part, contain ethanol, isopropanol, and n-propanol. Alcohol-based products have advantages over hand cleansing with soap and water alone, as they eliminate most of the germs and do not require dedicated infrastructures such as, for example, washbasins and running water. However, even alcohol-based solution could not replace handwashing, especially when the hands are obviously very dirty or when potential contamination with sporogenic bacteria, such as Clostridium difficile, is suspected.
2. PURPOSE OF THE RESEARCH
Microorganisms can be transmitted from the hands of patients to the hands of the hospital staff and then to another patient because gloves may have minor defects or because proper hand hygiene is not performed when changing gloves. The continuous changing of gloves is therefore not an indication of correct hygiene but is mistakenly considered to be such and, therefore, as various scientific evidences demonstrate, causes as a consequence a drastic reduction in the practice of hand hygiene. Girou et al. in their study conducted in five departments of a French university hospital found that in 64.4% of observations, hand hygiene was not performed because it was replaced by the clearly improper use of gloves and that microbial transmission it could have occurred in 18.3% of all contact cases since the used gloves had not been removed before performing the activities that required instead an act of scrupulous hygiene [9]. Pan et al. (2007), in a study carried out at the Cremona Hospital, reported compliance of health workers with hand hygiene by 19.6% while a 44% adhesion to the use of gloves was reported [10]. The aim of this study was to investigate the correct use of gloves and alcohol-based products for hand hygiene and identify opportunities for hand hygiene replacement with gloves among healthcare professionals working in the Department of Anesthesia and Intensive Care of a tertiary care University Hospital in Salerno (Italy). Furthermore, compliance with the practice of hand hygiene, which includes both the washing and the friction with the alcohol solution, was also evaluated. The ultimate aim was to correlate the data obtained for the hydroalcoholic solution consumption and the amount of antibiotics used for the treatment of HAI, in order to establish a possible correlation between incorrect hand hygiene and the HAI development [11].
3. MATERIALS AND METHODS
In this study, the frequency of gloves used in place of hand hygiene where required was measured according to WHO (opportunity) indications, through the direct observation method. Observers followed the operators during normal ward operations, without hindering their work. Opportunities for hand hygiene have been observed, and the occasions in which health workers replaced hand hygiene with the use of gloves and those in which, they adhered to washing and hand rubs have been identified. The concomitant use of antibiotics outside normal perioperative practice was then evaluated with an indirect method for the analysis of consumption data. Twenty monitoring sessions were conducted over a six-month period (January-June 2018) in the Department of Anesthesia and Intensive Care. The data collection tool was the observation form developed by the WHO.
The indicated instances of hand hygiene are mentioned below:
- before contact with the patient
- before a clean/aseptic maneuver
- after the risk of exposure to a body fluid
- after contact with the patient
- after touching what surrounds the patient
For each indication, there are five alternative actions:
- rub
- wash
- no hand hygiene
- use of gloves
- gloves not used
Evaluations were reported for each individual category of hospital staff: Doctor, Nurse and Health Social Care Worker (OSS).
The following final indicator was used for the evaluation of non-adherence to hand hygiene with concomitant use of gloves:
Non-adherence to hand hygiene with concomitant use of gloves; b) Adhesion to alcoholic friction of hands; c) Hand-washing adhesion. Instead, the consumption data, provided by the hospital ward itself, were used for the evaluation of d) The antibiotics used in the treatment of hospital-acquired infections; e) The hydro-alcoholic solution used by the healthcare professionals for hand hygiene.
Non-adherence to hand hygiene with concomitant use of gloves (%) =
 |
To estimate hand hygiene compliance, the final indicators used are as follows:
Adhesion to alcoholic friction of hands (%) =
 |
Hand washing adhesion (%) =
 |
A method of indirect analysis was added to the direct method, namely the observation carried out for hand hygiene opportunities (hand hygiene actions required, according to WHO indications) and activities. The latter was based on the detection of the consumption of alcohol-based hand hygiene products using data provided by the hospital department itself, using the electronic consumption registers. The data relating to the consumption of the hydro-alcoholic solution were collected through the form provided by the WHO. The consumption data of the antibiotics, explicitly used for HAI in the same period, was also evaluated as indirect data of good hygiene practices.
4. RESULTS AND DISCUSSION
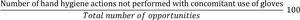
The first parameter evaluated was non-adherence to hand hygiene with concomitant use of gloves. The elaboration of the survey forms provided the number of actions, compared to the number of opportunities, to calculate the indicator used for the valuation over time. The following graph shows the total number of actions (Fig. 1).
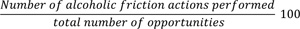
As can be seen from the graph, at the beginning of the observation time, the non-adherence to hand hygiene, with concomitant use of gloves, was very high; and for the following months, it even increased, with a peak in March. Subsequently, the number of actions decreased over time until the end of the monitoring session. Subsequently, the progress of adhesion to hand hygiene over time was evaluated. As previously explained, adherence to hygiene included both alcohol-based products and correct hand washing. The following graph shows the trend of adhesion to the practice of friction over time (Fig. 2).
As can be deduced from the figure, the number of actions at the beginning of the study was low and, in the following months, it increased until it reached a peak in May and then stabilized until the end of the observation. So over time, there has been an increase in this practice. The graph below shows the trend of handwashing over time (Fig. 3).
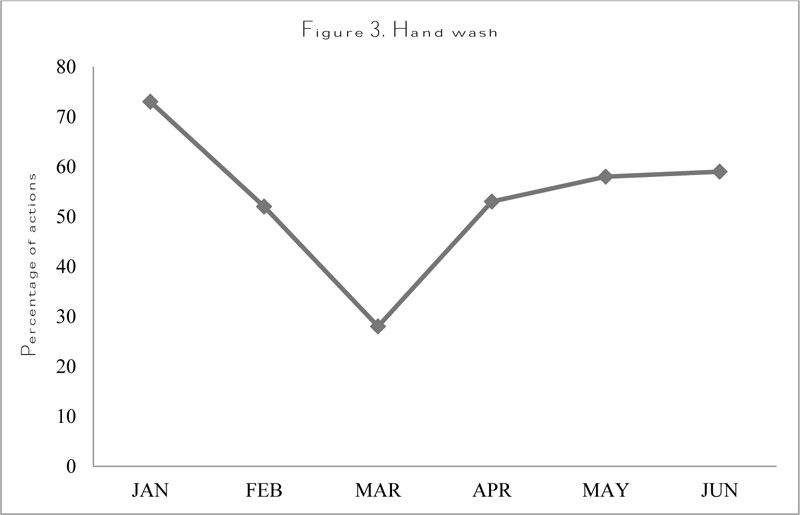
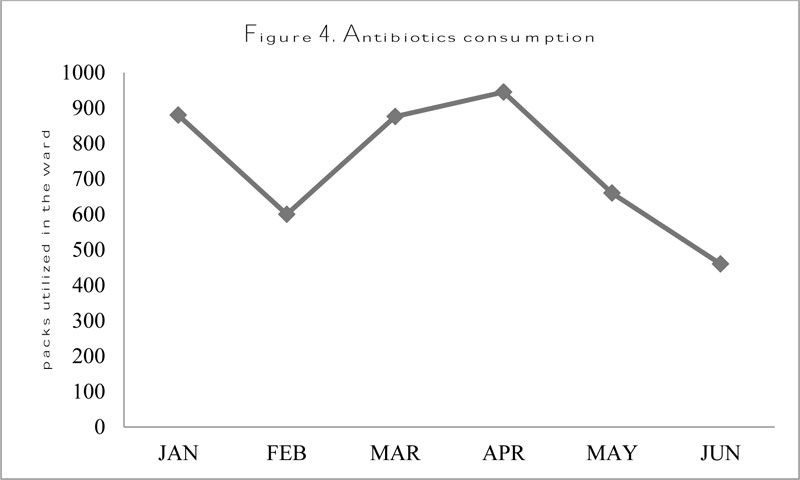
In the first part of the observation, the progress of adhesion to washing has drastically reduced, especially in March probably due to the recruitment of new inadequately trained nursing staff. The consumption data of antibiotics used in the treatment of HAIs was also analyzed (Fig. 4).
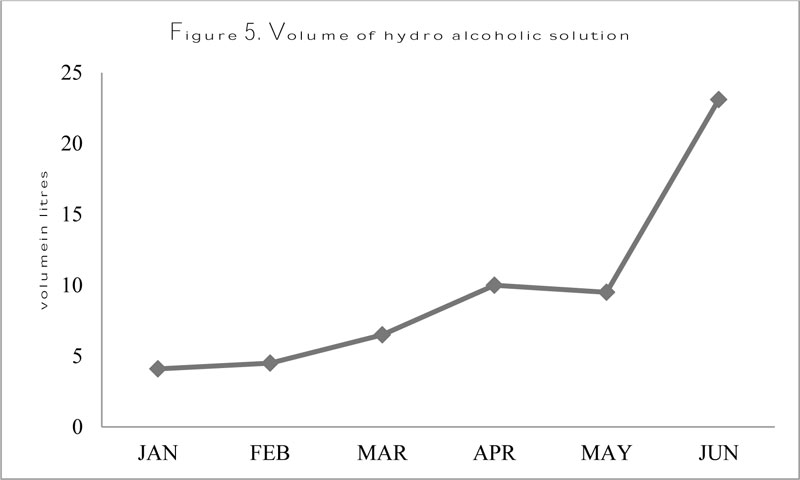
The consumption of antibiotics, initially decreased, only to increase again until a maximum peak in April, after which it decreased again until the end of the study. By comparing the trend of antibiotic consumption with the performance of the three practices, we can see that a high non-adherence to hand hygiene corresponds to a rather high consumption of antibiotics and instead shows a correspondence between a reduced non-adherence to the hygiene of the hands and reduced consumption of antibiotics. Another evaluation, with an indirect method, considered the distribution of the water-alcohol solution. The distribution pattern of the hydroalcoholic solution, in our specific case SEPTAMAN GEL in 100 mL bottles, was calculated as volume expressed in liters in relation to the six months of observations (Fig. 5).
As can be seen from the graph at the beginning of the study, the consumption of hydro-alcoholic solution was very low, however over time, it increased considerably until it reached a peak in June.
CONCLUSION
The purpose of this work was mainly to evaluate the progress of the practice of non-adhesion to hand hygiene with concomitant use of gloves. In fact, replacing hand hygiene with numerous changings of gloves nullifies the use of the gloves itself. Excessive use of gloves is therefore useless for the purpose of preventing transmission of pathogenic microorganisms from the hands of hospital staff to patients and vice versa . The trend of adherence to the practice of washing and friction of hands, consumption of the hydro-alcohol solution, and consumption of antibiotics was then evaluated. The results show that at the beginning of the study, the frequency of non-adherence to hand hygiene was very high for all three categories analyzed. During the six months of monitoring, there had been a reduction in non-adherence to hand hygiene with concomitant use of gloves and adhesion to washing and hand friction increased. The increase in hand hygiene was also confirmed by the increase in the consumption of hydro-alcohol solution. The trend of the three practices was then related to the consumption data of antibiotics, and from the results, it is clear that a reduced adherence to hand hygiene with concomitant use of gloves corresponds to higher consumption of antibiotics for the treatment of HAIs. This confirms that the use of gloves without the practice of washing or friction during the change is useless which may lead to the transmission of pathogenic microorganisms. The reversal of the trend for all three practices could be attributed to the presence of the monitoring operators and the constant training to which they were subjected. It is desirable to continue the observation period to confirm, if necessary, the correlation between excessive use of gloves without proper hand hygiene when changing gloves and the consumption of antibiotics used for the treatment of infections related to care. In light of the findings from this work, it is necessary to make the hospital staff increasingly aware of the correct practice of hand hygiene and to organize informative training sessions to promote the health of the individual and the community. Public health would benefit from different points of view: it would lead to the reduction in morbidity and mortality rates occurring due to the spread of infections, the limitation of inappropriate care practices for excessive use, such as the use of gloves, would lead to a better allocation of resources in the hospital environment. Another assessment, using an indirect method, considered the distribution of the water-alcohol solution. The distribution pattern of the hydroalcoholic solution (in our specific case SEPTMAN GEL, in 100 mL bottles) was calculated as volume expressed in liters in relation to the six months of observation. As can be seen from the graph, at the beginning of the study, the consumption of hydroalcoholic solution was very low, however over time, it increased considerably until it reached a peak in June.
LIST OF ABBREVIATIONS
| ANMDO | = National Association of Hospital Management Doctors |
| APIC | = the Association for Infection Control |
| CDC | = Center for Disease Control and Prevention |
| ECDC | = European Center for Disease Prevention and Control |
| HAI | = hospital-acquired infection |
| HICPAC | = Advisory Committee on Health Infection Control Practices |
| MDR | = multiple drug-resistant bacteria |
| MRSA | = methicillin-resistant Staphylococcus aureus |
| OSS | = Health Social Care Worker |
| SItI | = Italian Hygiene Society |
| VRE | = Enterococci resistant to vancomycin |
| WHO | = World Health Organization |
AUTHOR CONTRIBUTIONS
Developed the idea ES and GB; original draft preparation, M.F, S.L. and A.M.; writing—review and editing, R.M., M.G. and G.L.; statistical analysis—figures preparation, M.R., V.D.O. and M.C.; all authors revised the paper for final approval.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not Applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICTS OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDEGEMENTS
Declared none.


