All published articles of this journal are available on ScienceDirect.
Preoperative Concerns of Older Patients Undergoing Non-cardiac Surgery: A Systematic Review and Meta-analysis
Abstract
Background
Older adults (≥ 50 years) possess unique preoperative concerns influenced by age-related needs, perceptions, and health status. When left unaddressed, these concerns are risk factors for postoperative morbidity and mortality. Despite the aging demographic, these concerns in older patients have not been systematically examined. This systematic review and meta-analysis aims to summarize the preoperative concerns of older patients.
Methods
Five databases were searched from January 1, 2000 to March 26, 2023. Studies with 1) patients ≥ 50 years undergoing non-cardiac surgery; 2) concerns identified preoperatively with validated instruments; 3) at least one preoperative concern reported (mean, degree or incidence of concern); 4) randomized controlled trials, prospective cohort, or cross-sectional studies were included. Concerns were classified into domains and subdomains. Meta-analysis was performed when two or more studies assessed concerns utilizing the same instrument.
Results
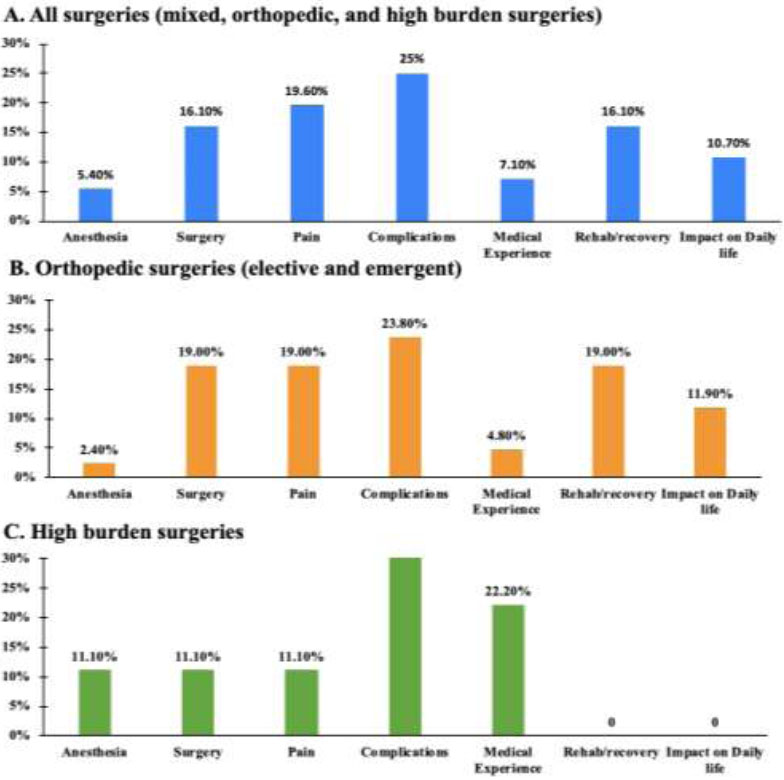
Seventeen studies with 1,777 patients were included. The mean age was 68.3 ± 9.9 years, with 51.4% female. Surgeries were classified as mixed, orthopedic (elective or emergent), and high-burden (abdominal, vascular, oncological). Concerns were categorized into domains: 1) anesthesia, 2) surgery, 3) pain, 4) complications, 5) medical experience, 6) recovery and rehabilitation, and 7) impact on daily life. Patients reported a greater degree of anxiety relating to surgery than anesthesia: 1.54 (95% CI: 1.12-1.95, P<0.00001). The top three concerns across all surgeries (mixed, orthopedic, and high-burden) were complications, pain, and rehabilitation/recovery. Pain and complications were the greatest concerns in elective orthopedic procedures and emergent procedures, respectively. In high-burden surgeries, patients were primarily concerned about complications.
Conclusion
Surgery-related concerns were 50% greater than anesthesia-related concerns. The three main concerns in older patients were complications, pain, and rehabilitation/recovery. The top concerns varied among specific surgical types. These findings emphasize the importance of tailoring preoperative counseling to address specific fears of each surgical population.
1. INTRODUCTION
The current population is aging rapidly, with over 25% consisting of older adults [1]. With the projected age increase, the prevalence of older adults undergoing surgery is anticipated to increase. Half of the population over 65 years of age will require surgery at one point in their lives, and 53% of all surgical procedures are being performed on older adults [2].
During the preoperative period, surgical patients often suffer from anxiety and worry [3]. These negative feelings reflect their preoperative concerns, which can vary from surgical and anesthetic complications to financial strain on family members [3]. The health-related concerns in older patients may differ from those of younger age groups. For example, older adults may be more concerned with preserving quality of life rather than the duration of life [4]. If left unaddressed, the concerns of older patients are independent risk factors for postoperative mortality and morbidity [5].
Old age itself is a risk factor for poor surgical outcomes as older adults have a deteriorating physiological reserve in all organ systems. These changes predispose older adults to perioperative adverse events [6]. These worsened outcomes can negatively impact their functional trajectory and ability to engage in their independent activities of daily living during the recovery process [7]. Compared to young adults, their increased susceptibility to adverse surgical outcomes may contribute to their unique preoperative concerns [8].
Patient-centered care involves incorporating the specific healthcare needs of patients and actively involving them in their treatment process [9]. National policies and guidelines have pointed to the necessity of patient participation through shared decision-making processes [10-12]. Despite the aging demographic, the unique health-related priorities of advanced age, and their increased risk of postoperative complications, the preoperative concerns in patients over 50 years old have not been systematically examined. This review aimed to comprehensively summarize the preoperative concerns of older patients undergoing non-cardiac surgeries. Identifying and addressing preoperative concerns can optimize patient-centered care in the older surgical population [13].
2. METHODS
2.1. Study Design and Registration
This systematic review is reported as per the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) reporting guidelines [14]. The protocol of this systematic review is registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42023442055).
2.2. Search Strategy
The search strategy was developed with a medical information specialist (ME). The following databases, all via the Ovid platform, were searched: MEDLINE, MED- LINE ePubs Ahead of Print and In-process, Embase, Cochrane Central Register of Controlled Trials, and the Cochrane Database of Systematic Reviews. Search results were limited to English language and human subjects, and the year range from January 1, 2000 to March 26, 2023. The search strategies included controlled vocabulary and text word terms in the following component blocks: preoperative and elderly, surveys/questionnaires and patient concerns, and qualitative component and surgery component. Results were limited to English language, adults, and conference and/or non-journal materials were removed at source. All searches were conducted on March 26, 2023. Reference lists of included articles were searched to find related articles missed in the systematic search. Full details regarding the search strategy are attached in the appendix of the supplementary material.
2.3. Study Selection
Title and abstract screening of identified articles was carried out independently by two reviewers (MQ, WL) using Covidence [15]. The full-text review was completed independently by two reviewers (MQ, WL), and conflicts were resolved through deliberation with a third (EY). The inclusion criteria were: 1) Patients aged ≥ 50 years; 2) undergoing non-cardiac surgeries; 3) assessment of preoperative concerns conducted prospectively with valid measures; 4) quantitative results were reported; 5) randomized controlled trials (RCTs), prospective cohort studies, and cross-sectional studies; and 6) English language. Exclusion criteria were: 1) ambulatory surgical populations, 2) wait-list populations, 3) studies with quantitative results that could not be compared or ranked, 4) retrospective studies, case reports/series, case-control studies, conference abstracts, and qualitative studies, and 5) studies that provided a singular score that represented broad measures of concern (e.g. surgical fear scores).
This review defined preoperative concerns as negative thoughts and emotions directly related to upcoming surgery and/or its outcomes. Synonymous terms used throughout scales included “fears,” “cause of anxiety,” and “worries.”
2.4. Data Extraction
Data extraction was performed by two independent reviewers (MQ, WL) using a standardized Excel file. Data on study characteristics (e.g., author, publication year, sample size), participant characteristics (e.g., surgery, demographics), and questionnaires (e.g., survey format, item generation, and setting of survey administration) were extracted from all included studies. Finally, concern items and relative rankings reported by studies were extracted and classified under seven pre-established concern domains. All conflicts were resolved by a third reviewer (EY).
2.5. Data Analysis
This review employed both qualitative and quantitative analysis. Characteristics of the studies, patient popu- lations, and scales were summarized descriptively in tables. The surgical procedures were classified as either non-cardiac mixed, orthopedic, or high-burden (vascular, oncological, and abdominal). Mixed surgery was defined as including various surgical specialties in a single study (i.e., ophthalmology, gynecological, neurosurgery, oral, plastic, urological, otolaryngology, general, etc.). Orthopedic surgeries were further divided into elective and emergent procedures. High-burden surgeries included vascular, oncological, and abdominal procedures [16]. The composite of non-cardiac mixed, orthopedic, and high-burden surgeries was termed “all surgeries” in this review.
The identified concerns within the included studies were thematically classified into the following seven concern domains: 1) anesthesia-related, 2) surgery-related, 3) pain-related, 4) complications, 5) medical experience, 6) recovery and rehabilitation, and 7) the impact on daily life. The process of categorization was based on an extensive review of relevant literature [17-28]. Further subdomains generated through an inductive thematic analysis were used to harmonize heterogeneous data, allowing for detailed analysis.
Following data extraction, the pertinent concerns of each study were identified following the methodologies of previously published articles [29, 30]. Items ranking in the top 25% of importance were selected for each survey. For instance, the top two concerns were chosen if eight concerns were studied. For studies with over 40 items, only the top 10 were considered to limit their overall impact on rankings. The top quartile items were assigned points based on relative rankings (e.g., Rank 1, given ten points; Rank 10, given one point). The total sum of points allocated to each domain and subdomain is presented as a percentage of the total available points from the sample.
To address methodological heterogeneity of included studies, separate analyses were conducted for scales that assessed less than three concerns. These included the Amsterdam Preoperative Anxiety and Information Scale (APAIS), Visual Analogue Scale (VAS), Fear of Surgery, and Fear of Anesthesia scales.
2.5.1. Measures of Preoperative Concerns
The APAIS is a well-validated, self-employed tool consisting of six questions rated on a 5-point Likert scale (1: not at all, 5: extremely) [31]. The relevant subscale scores were: 1) anesthesia-related anxiety (APAIS-AA) and 2) surgery-related anxiety (APAIS-SA) [32].
The VAS-Fear of surgery and anesthesia scales are two single-item measures that evaluate the fear of surgery and anesthesia, respectively [33]. Meta-analysis was per- formed using Cochrane Review Manager version 5.4 when two or more studies adopted the same scale [34]. Surgery vs anesthesia-related anxiety was analyzed as a continuous outcome using Mean Difference (MD). The outcome was presented as a forest plot. The continuous event was combined using the Inverse Variance (IV) method with a 95% confidence interval (CI). A random effect model was used, and a P-value of 0.05 or less was considered significant.
2.6. Quality Assessment
Study quality was evaluated by two independent reviewers (WL, EY) using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Randomized Controlled Trials (RCTs), cross-sectional studies, and cohort studies [35, 36]. Disagreements between the two independent reviewers were resolved through discussion and consensus or by another reviewer (FC). For RCTs, bias was assessed through seven questions across three domains: (1) administration of intervention/exposure; (2) assessment, detection, and measurement of outcome; and (3) statistical conclusion validity. The remaining questions evaluating bias related to selection and allocation and participant retention were not applicable to this study as the primary outcome of this review was preoperative concerns in all patients. Therefore, these questions were excluded from the quality assessment. The tool consisted of seven questions for cross-sectional studies and four for cohort studies, following the removal of questions deemed not applicable to this study. All question items were evaluated with “yes” (the study fulfilled the domain criteria), “no” (the study did not fulfill the domain criteria), or “unclear” (the study’s adherence to the domain criteria could not be conclusively proven). Studies with a “yes” score on more than 70% of the questions were considered high-quality, those with a score between 50-70% were considered medium quality, and those with a score less than 50% were considered low-quality [37, 38].
3. RESULTS
3.1. Study Selection
The results of the search strategy are summarized in Fig. (1). A total of 17,714 studies were identified. After the removal of duplicate studies, title, and abstract screening, 193 full-text studies were assessed for eligibility. An additional 176 studies were excluded due to failure to meet the inclusion criteria. A total of 17 studies fulfilled the selection criteria and were included for qualitative synthesis [39-55], and two studies were included for quantitative analysis [45, 53].
3.2. Study Characteristics
The characteristics of the included articles are summarized in the supplementary material (Table S1). In total, 1,777 patients were included in 17 studies (mean age: 68.3 ± 9.9 years, 51.4% female). Twelve studies were cross-sectional [40-42, 44, 46-51, 53, 54], three were prospective cohorts [43, 45, 52], and two were RCTs [39, 55].
Concerns were evaluated across various surgical populations, which were classified into mixed [39-42], emergent orthopedic [43, 44], elective orthopedic [45-49], and high-burden surgeries [50-55]. Two articles reporting on the same data set were included because they presented the results of different measures of concern (APAIS and self-generated scale) [50, 51].
The quality assessment of the included studies is detailed in the supplementary material (Tables S2-4). All studies, including cross-sectional, cohort, and RCTs, were given a score higher than 70%, suggesting high quality. Of the 11 cross-sectional studies, seven did not fully describe the study settings in detail [40-42, 46-49], and four did not adjust for confounding variables [44, 50, 51, 53]. Adjustment of confounding variables was also not performed in two of the four cohort studies [43, 45]. Lastly, blinding by outcome assessors was deemed unclear in both RCTs [39, 55]. All studies fulfilled the remaining domain criteria of the assessment tools.
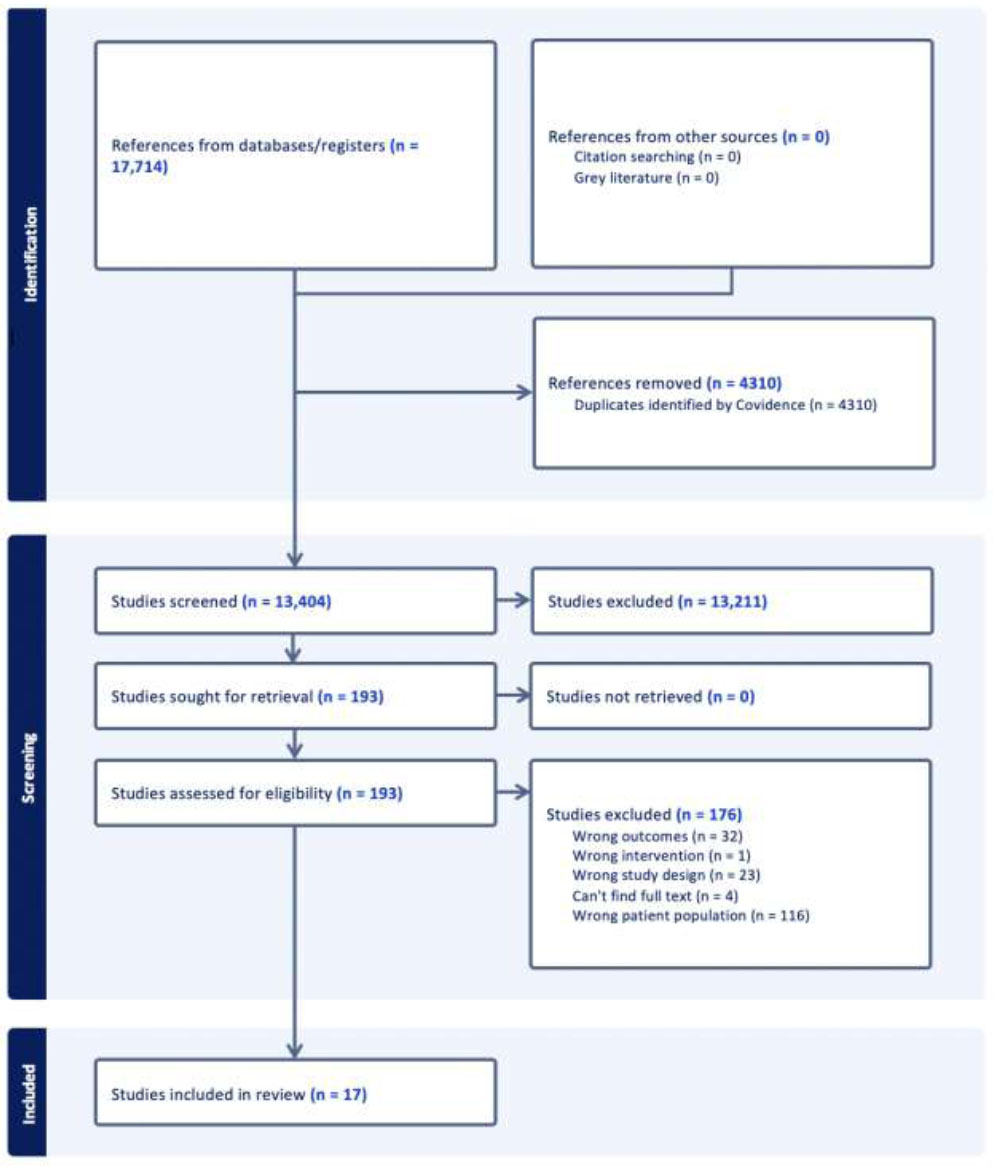
PRISMA flowchart.
3.3. Identification of Assessment Measures
Substantial heterogeneity was observed in the assessment measures used across studies. Scales varied in item number (range: 5-65) and the types of concerns. Studies reporting on three or more concerns used study-specific surveys generated ad-hoc to assess preoperative concerns [40, 41, 43-50, 54, 55]. The characteristics of these questionnaires are summarized in Table S5. All studies reported qualitative strategies such as literature review, patient interviews, expert panels, and pilot studies to inform item generation and ensure the inclusion of relevant concerns (Table S5). Seven studies employed measures assessing less than three concerns [39, 40, 42, 45, 51-53]. These were the APAIS (n=6) and the VAS fear of surgery and anesthesia scales (n=1).
3.4. Classification of Domains and Subdomains
In total, 316 individual concern items were extracted and categorized into seven domains (Table 1). The concern domain ‘Impact on daily life’ consisted of the most items (n=68, 21.5%) (Table S6). The number of concern domains assessed by each study ranged from 2-7 (mean: 4.5). ‘Surgery’ and ‘Anesthesia’ were the most widely assessed domains across all included studies, each appearing in 82% of studies (n=14) (Table S7). After thematic analysis, concerns were further classified into 26 subdomains (Table 1). Risks associated with anesthesia were most assessed subdomains (n=14, 82.3%) followed by postoperative pain (n=10 studies, 58.8%).
3.5. Comparative Analysis of APAIS and VAS-fear Scales; Anesthesia and Surgery-related Anxiety
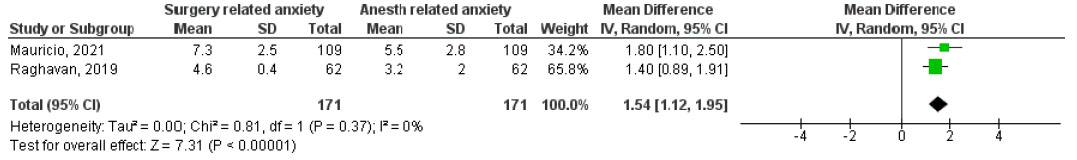
Seven studies employed scales that assessed less than three concerns. Of these, six used the APAIS [39, 40, 42, 45, 51, 53], while the remaining study used the VAS Fear of Surgery and Fear of Anesthesia scales [52]. In all seven studies, surgery-related concerns scored higher than anesthesia-related concerns, indicating greater concerns for surgery than anesthesia (Table 2). A meta-analysis was performed on two studies that both used the APAIS tool: one orthopedic and one mixed surgery [45, 53]. The other studies were not included in the meta-analysis due to heterogeneity in reported outcomes. Across these studies, patients reported a greater degree of anxiety relating to surgery than anesthesia. The pooled mean difference between surgery-related anxiety and anesthesia-related anxiety was 1.54 (95% CI 1.12-1.95, I2=0%, P<0.00001) (Fig. 2).
| Concern Domain | Concern Subdomain | Definitions and Included Variables |
|---|---|---|
| Anesthesia | Associated risks | Death, not waking up after, strokes, heart attacks, nerve damage, other |
| Awareness | Waking up intraoperatively, hearing operation noises | |
| Postop side-effects | Nausea and vomiting, memory loss, headache, drowsiness | |
| Surgery | Operation fear | Surgery itself, death |
| Outcome | Surgery failure, need for reoperation | |
| Pain | Intraop pain | Pain during surgery, needles and injections |
| Postop pain | Pain after surgery, discharge, during rehabilitation, chronic pain | |
|
Complications (Cx) |
General Cx fear | General fear of Cx |
| Cardiovascular | Formation of blood clot, transfusion | |
| Infections | Postop infections, risk with AIDS/hepatitis | |
| Nerve damage | Paralysis, nerve injuries | |
| Re-injury risk | Re-fracture/dislocations of new joints, falling | |
| Medical error | Operation on wrong leg, wrong material used | |
| Medical Experience | Fear of the unknown | Not knowing procedure type, anesthesia type, potential malignancy, Dx |
| Distrust in physician competence | Concerns about anesthesiologist and surgeon proficiency, medical error | |
| Hospital environment | Operating room quality, sanitation, food quality | |
| Financial implications | Hospitalization expenses, ability to pay medical bills, financial burden on family | |
| Communication with HCWs | Nursing care, questions not answered, attitude of medical staff | |
| Rehabilitation and Recovery | Recovery delay | Long/short hospital stays, length of recovery, delayed recovery |
| Postop rehab | Postop physical therapy: quality and availability | |
| Functional recovery/mobility | Ability to kneel, squat, sit cross-legged, lift heavy objects | |
| Impact on Daily Life | Long-term disability | Ability to walk, stiffness, use of equipment aids |
| Return to daily activity | Caring for children, return to work, recreational activity, sexual activity, changes to sleeping habits, lifelong medications | |
| Self-care | Physical dependence, ability to drive car, ride bike, dress or bathe oneself | |
| Psychosocial concerns | Depression, treatment/judgement from others, burden to others, embarrassment due to surgery, scars | |
| Economic | More expenses than expected, ability to pay, family payment burden |
| Study | Surgery | Sample Size | Questionnaire | Rangea | Rank | Concern Domain | Outcome % or Mean ± SD |
|---|---|---|---|---|---|---|---|
| Mauricio 2021 [53] | Mixedb | 109 | Portuguese APAIS-SA | 2-10 | 1 | Surgery | 7.3 ± 2.5 |
| - | - | Portuguese APAIS-AA | - | 2 | Anesthesia | 5.5 ± 2.8 | |
| Maurice-Szamburski 2013 [42] | Mixed | 78 | French APAIS-SA | 2-10 | 1 | Surgery | 3.8 ±2.3 |
| - | - | French APAIS-AA | - | 2 | Anesthesia | 3.5 ±1.8 | |
| Karakoyun 2021c [39] |
Mixed | 46 | Turkish APAIS-SA | 3-15 | 1 | Surgery | 11.2 |
| - | - | Turkish APAIS-AA | - | 2 | Anesthesia | 8.5 | |
| Lim 2020 [40] |
Mixed | 140 | Korean APAIS-SA | 3-15 | 1 | Surgery | 9.5 ± 3.9 |
| - | - | Korean APAIS-AA | - | 2 | Anesthesia | 9.1 ± 4.0 | |
| Raghavan 2019 [45] |
Orthopedic | 62 | English APAIS-SA | 2-10 | 1 | Surgery | 4.6 ± 0.4 |
| - | - | English APAIS-AA | - | 2 | Anesthesia | 3.2 ± 2.0 | |
| Jovanovic 2021c [51] |
Vascular | 385 | Serbian APAIS-SA | 3-15 | 1 | Surgery | 43.40%d |
| - | - | Serbian APAIS-SA | - | 2 | Anesthesia | 31.20%e | |
| Buehrer 2015 [52] |
Vascular | 59 | VAS Fear of Surgery | 1-10 | 1 | Surgery | 2.7 ± 3.9 |
| - | - | VAS Fear of Anesthesia | - | 2 | Anesthesia | 1.3 ± 2.7 |
APAIS-SA: Amsterdam Preoperative Anxiety Information Scale – Surgery-related anxiety subscale.
VAS: Visual Analogue Scale.
aDue to differences in factor analysis between scales of differing analysis, ranges of subscales measuring anesthesia-related and surgery-related anxiety differed depending on the inclusion of Items 3 (anesthesia) and 6 (surgery).
bMixed surgeries: Surgeries includes abdominal, breast, cardiac, colorectal, general, gynecologic, neurosurgery or neurosurgery spine surgery, ophthalmologic, oral, orthopedic, otolaryngology, plastic, urologic, and vascular surgeries).
No report on standard deviations for mean scores.
dCut-off value for incidence >8.
3.6. Identification of Top Concerns
Twelve studies were included in the analysis of top concerns [40, 41, 43-50, 54, 55] (Table S5). Fig. (3) compares the distribution of all concern domains ranking in the top quartile in all surgeries (mixed, orthopedic, and high-burden surgeries), orthopedic surgeries only, and high-burden surgeries only. Table 3 displays the top three domains of concern in each surgical discipline.
3.6.1. Top Concerns across all Study Populations
Among the 56 items ranked within the top quartiles of all the included studies, the concern domains of ‘complications,’ ‘pain’, and ‘rehabilitation/recovery’ were the top three in all surgeries (Table 3). In the ‘complications’ domain, the main subdomain concerns were regarding a ‘general fear of complications’ and ‘nerve damage.’ In the ‘pain’ domain, the main subdomain concerns were regarding ‘intraoperative pain’ and ‘postoperative pain.’ Lastly, in the ‘rehab/recovery’ domain, the main subdomain concern was regarding ‘functional recovery.’ For elective orthopedic patients (n = 5 studies, 418 patients), ‘pain’ was ranked as their greatest concern (Table 3). The subdomains of ‘intraoperative pain’ and ‘postoperative pain’ were the most contributory within this domain. For emergent orthopedic patients (n = 2 studies, 227 patients), ‘complications’ were ranked as their greatest concern (Table 3). The subdomain of ‘reinjury risk’ was the most contributory within this domain. For high-burden surgeries (n=3 studies, 501 patients), ‘complications’ were ranked as their greatest concern (Table 3). The subdomain of ‘general fear of complications’ was the most contributory within this domain.
4. DISCUSSION
This systematic review and meta-analysis assessed the preoperative concerns of older patients undergoing non-cardiac surgery [39-55]. Concerns regarding surgery are fifty percent higher than anesthesia concerns. Concerns were distributed across seven overarching domains: anesthesia, surgery, pain, complications, medical expe- rience, rehabilitation/recovery, and impact on daily life. Across all studies on the different types of surgeries, complications, pain, and rehabilitation/recovery were the dominant concerns. Specific concerns varied among different types of surgeries. For elective orthopedic surgeries, pain was a significant concern, followed by nerve damage and paralysis. Patients undergoing emergent orthopedic surgeries did not rank pain as highly, focusing instead on complications and functional recovery. In high-burden surgeries, including vascular, cancer, and abdominal surgery, patients emphasized concerns about postoperative complications, fear of unknown/surgery, and the medical experience.
| - | - | - | Orthopedic Surgeries | |
|---|---|---|---|---|
| - | All Surgeriesa (n = 12) [40, 41, 43-50, 54, 55] | High burden Surgeriesb (n = 3) [50, 54, 55] | Electivec (n = 5) [45-49] | Emergentd (n = 2) [43, 44] |
| Rank | Domain | Domain | Domain | Domain |
| 1 | Complications | Complications | Pain | Complications |
| 2 | Pain | Med Experience | Complications | Rehab/Recovery |
| 3 | Rehab/Recovery | Pain, Surgerye | Rehab/Recovery | Surgery |
a. Includes abdominal, cancer surgeries, mixed surgeries, total ankle arthroplasties, total hip arthroplasties, total knee arthroplasties and spinal surgeries.
b. Includes abdominal, cancer and vascular surgeries.
c. Includes total ankle arthroplasties, total knee arthroplasties, spinal surgeries.
d. Includes total hip arthroplasties.
e. Pain and surgery received the same proportional weight and are thus both presented.
Surgery and anesthesia were the domains of concern that were most widely assessed. The APAIS, VAS Fear of surgery, and VAS Fear of anesthesia are specific scales that assess these concerns. Surgery-related concerns consistently scored higher than anesthesia-related concerns, being fifty percent greater in the meta-analysis. The rationale may be multifactorial. Factors such as the extensiveness of surgery, the prognosis of their diagnoses, such as cancer, and the unknown experience all contribute to surgery-related concerns [3]. Additionally, the lack of effective communication from surgical providers about the operation itself can worsen surgery-related anxieties [56]. Patients had indicated that their anxiety would be lessened if the surgical procedure was explained to them more clearly. Taken together, elements of the surgery and the lack of clear communication surrounding the procedure preoperatively can contribute to greater surgery-related concerns in comparison to anesthesia.
In patients undergoing elective orthopedic operations, the fear of pain, either intraoperatively or postoperatively, was pronounced. This is understandable, as joint replacements are particularly painful procedures [57]. Numerous perioperative strategies exist to minimize pain, including the use of regional anesthesia, multimodal analgesia, and neuropathic pain modulators [57]. Better communication and education about the perioperative management of pain from the health care professional is needed. Interestingly, a study in China showed differing concern priorities in orthopedic patients, with distrust in physicians as a top concern, while pain was a smaller concern [46]. This suggests that cultural and geographic factors may influence preoperative concerns.
Nerve injury/paralysis was another major concern among orthopedic patients, which may be due to surgery itself or anxiety related to regional anesthesia, such as epidural/spinal anesthesia or regional blocks. Nerve injury in older patients can increase their risk of falls, due to factors associated with aging [58]. Additionally, the heightened concern about nerve injury and paralysis in this patient population can be viewed through a psychosocial lens. These injuries severely impede their ability to return to work, socialize, and maintain independence and autonomy [59]. To allay these concerns, both surgeons and anesthesiologists need to offer detailed education and reassurance to older patients regarding the surgical procedures, risk of complications, and nerve injury/paralysis relating to the surgery or regional anesthesia [3].
In emergent orthopedic surgeries, the risk of reinjury was the top concern. Postoperative fear of falling has been found to be common in hip fracture patients, with the fear persisting up to one year post-injury [60-62]. This highlights the importance of early identification of concerns, education, and intervention to allay anxiety [63]. These patients also had prominent concerns regarding their functional recovery. Functional recovery is particularly important in older patients as it allows them to engage in their activities of daily living (ADLs) and instrumental activities of daily living (IADLs), both important in the preservation of their quality of life.
The high-burden surgical populations, including vascular, cancer, and abdominal surgeries, reported medical experience with fear of the unknown as a prominent concern. This is defined as an individual’s propensity to experience fear caused by the perceived absence of information at the point of processing [64]. Patients undergoing high-risk surgeries are often aware that their procedures carry a higher risk of complications, longer recovery times, and uncertain outcomes [55]. Thus, this concern may manifest from the fear of adverse outcomes and their implications on health, quality of life, and life expectancy.
Lastly, it is important to recognize older adults are not a homogenous group. They can be further stratified into young-old, old, and oldest-old [65]. As such, there may be variability in concerns depending on the specific age range (i.e., 50-year-old vs. 80-year-old). In fact, as patients reach their last decade of life (i.e., oldest old), their primary preoperative concerns are more likely related to functional or health state (e.g., walking independently), symptom control (e.g., pain), and survival/death (e.g., living long enough to attend a milestone such as a family member’s wedding) [66]. This nuance is critical to appreciate. Despite there being a supposed “cut-off” for older adults, there still exists variability in concerns among older age ranges that should be clinically appreciated when seeing patients in the preoperative setting.
5. IMPLICATIONS
The findings of this review underscore the necessity for healthcare providers to address patients' concerns about pain proactively and to employ comprehensive pain management protocols that can alleviate anxiety and improve patient outcomes. For elective orthopedic surgeries, management of pain needs to be a critical aspect of preoperative education and postoperative care planning. For high-burden surgeries, the distinct pattern of concerns, including a fear of the unknown, indicates a need for clear communication and psychological support. These insights can inform targeted interventions to improve patient education, perioperative care, and support mechanisms tailored to the specific needs of different patient groups, as well as to enhance patient outcomes and satisfaction.
6. LIMITATIONS
This review has several limitations. First, there was a significant degree of heterogeneity in the numbers, types, and methodology of concerns across studies. Domains and subdomains that were assessed more frequently may have been over-represented, leading to study bias. Identification of the most important concerns was assessed as a relative ranking and thus depended on which concern items were studied.
CONCLUSION
Surgery-related concerns were greater than anesthesia-related concerns. Among all types of surgeries, the three main concerns were complications, pain, and rehabilitation/recovery. In elective orthopedic patients, the number one concern was pain, followed by nerve injury/ paralysis, whereas postoperative complication is the top concern in both emergency orthopedic and high-burden surgery. It is integral that healthcare providers deliver clear communication and education to allay these preoperative concerns among older patients.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
AVAIALABILITY OF DATA AND MATERIAL
All the data and supportive information are provided within the article.
FUNDING
This work is partially supported by the Ontario Ministry of Health Innovation Fund, the University Health Network Foundation, and the ResMed Foundation.
CONFLICT OF INTEREST
Frances Chung is the Editorial Advisory Board member of the journal The open Anesthesia Journal.
ACKNOWLEDGMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.
Supplementary material, along with the published article, is available on the publisher’s website.