All published articles of this journal are available on ScienceDirect.
Relationship between Temperature and Pain Sensation Following a Peripheral Ulnar Block: An Exploratory Pilot Study
Abstract
Objectives
In recent years, measuring skin temperature has been studied as a potential method for predicting the success of peripheral nerve blocks. However, additional research is needed. This study aimed to explore the temperature course following a peripheral Ulnar Nerve Block (UNB).
Methods
An exploratory observational study was conducted in which an ulnar nerve block at the wrist was performed on healthy volunteers using 1% lidocaine (1 ml). Skin temperature was measured using probes and analyzed in relation to pinprick testing, with detailed temperature profiles depicted as graphs to allow visual analysis of temperature variations. Additionally, temperature at specific time points was analyzed based on changes in pinprick testing and/or temperature.
Results
Ten UNBs were performed on five subjects. The temperature profiles revealed an increase in temperature in all 10 cases, with a median temperature of 34.2°C (range 33.7–34.7) during the plateau phase. A gradual decrease in temperature was observed in nine out of ten UNBs before the return of pain sensation, with a median duration of 20.0 minutes (range 5–43) and a median decrease of 1.1°C (range 0.5–4.1).
Conclusion
The temperature course following a peripheral ulnar nerve block was analyzed in this study. Based on the results, skin temperature is suggested to serve as an indicator of a successful nerve block. Additionally, it is suggested that the temperature decreases prior to the return of pain sensation, which could be used to infer a declining block in clinical practice.
1. INTRODUCTION
Peripheral nerve blocks are commonly used for preoperative and postoperative pain management. The current assessment of a peripheral nerve block mainly relies on subjective narratives of painlessness based on qualitative measurement methods, such as pinprick, cold, heat, touch, etc [1-3]. Pinprick is widely accepted as a standard sensory assessment of local anesthetic effects [2-4], although it does not fully translate to pain perception in clinical settings [2]. An objective method to assess peripheral nerve blocks would be considered beneficial, but no such method has yet been established.
A physiological response is induced by a peripheral nerve block, in which sympathetic fibers are inhibited [5], leading to vasodilation, increased blood flow, and consequently, an increase in tissue and skin temperature. Based on these physiological mechanisms, temperature has been explored as a means of predicting a successful nerve block in the upper extremity [1, 4, 6-9], with a significant temperature increase most pronounced distally [1, 7, 10].
To date, the course of temperature following the administration of a peripheral nerve block has not been thoroughly investigated. It has been hypothesized that following a peripheral ulnar nerve block, a temperature increase would be observed, reaching a temperature plateau as a result of maximum vasodilation. A corres- ponding decrease in temperature would then be expected as the block begins to subside, coinciding with changes in pain sensation.
The relationship between skin temperature and pain sensation following a peripheral ulnar nerve block was aimed to be explored in this study.
2. SUBJECTS AND METHODS
The study was approved by the Regional Committees on Health Research Ethics for Southern Denmark (jf. No. S-20200081-CSF).
Healthy volunteers were recruited via social media posts shared with acquaintances and medical students at the University of Southern Denmark between August and September, 2020. The study was conducted in accordance with the Declaration of Helsinki, and informed written consent was obtained from all participants. No payment was provided, but transportation costs and a meal voucher were reimbursed on the day of the trial.
Inclusion criteria included adults aged 18 years or older and weighing between 50-120 kg. Exclusion criteria included inability to understand and/or speak the Danish language, use of nicotine-containing products, previous surgery on the upper extremities, permanent intake of painkillers, random intake of painkillers on the days of the experiments, medicine with vitamin K antagonist, high dose heparin or fractionated heparin, infection, redness or rash around the injection site, allergy to lidocaine, coagulopathy, diabetes mellitus, peripheral neurological disease, epicondylitis medialis, Raynaud’s disease, or pregnancy.
2.1. Procedure
The trial was conducted at the recovery unit, where the subjects were continuously monitored using a standard ECG, a pulse oximeter, and a blood pressure cuff, along with visual observation for potential adverse side effects. An anaphylaxis kit was prepared in case of adverse reactions, such as convulsions or cardiovascular depression. Possible cardiovascular side effects, including hypertension, hypotension, tachycardia, bradycardia, or, in severe cases, arrhythmias or cardiac arrest, were considered. Similarly, symptoms affecting the central nervous system, such as sensory disturbances, blurred vision, tremors, fainting, etc., were monitored. Appro- priate medication would be administered according to the facility’s local guidelines. The subject was seated in an armchair with the hands positioned supinated on the armrests. Direct sunlight was avoided, and all clothes were removed from the hands and forearms. The subject was adapted to room temperature for a minimum of 10 minutes before the UNB was performed. The room temperature was maintained at a constant 22°C. Philip’s skin surface temperature probes (Netherlands) were placed on the 5th outer phalanx on the palmar side of both hands [10]. The sensors were connected to a Phillips IntelliVue X2 monitor device (Netherlands), and conti- nuous measurements were ensured, with the subject's opposite finger acting as its own control. The temperature equipment was concealed from the subject, and a thin opaque blanket was placed over the forearm to blind the subject during pinprick testing. Pinprick testing was conducted using a 25G Uniplex Nanoline needle (GM Medical, Denmark) by a single operator to standardize the procedure. Measuring points for pinprick testing were marked with a pen on the 2nd and 5th proximal phalanx on the palmar side to standardize the tests. The 2nd phalanx was used as a control due to its pure sensory median innervation [11].
2.2. Blocks
The blocks were administered by a chief physician in anesthesiology with experience in over 15,000 ultrasound-guided peripheral nerve blocks. The ulnar nerve block was guided by ultrasound and performed using 1 ml of a 1% lidocaine solution. An out-of-plane technique was employed within the neurovascular sheath where the ulnar nerve runs to execute the nerve block at wrist level, using a G27 needle (Braun, Germany). Following a one-hour intermission after the termination of the first experiment to ensure the cessation of the analgesic effect and the validity of the new measurements, the experiment was conducted on the opposite hand of the subjects. The duration of the UNBs was anticipated to be one to two hours [12].
2.3. Pinprick Tests and Temperature Measurements
Pinprick tests were performed every minute from the onset of the nerve block. When full impact, defined as loss of pain sensation, was demonstrated by the pinprick test, the block was included in the data collection. If loss of pain sensation was not achieved within 45 minutes, the block was considered incomplete and excluded. Following the indication of pain sensation loss by the subject, pinprick testing was performed, and temperature measurements were read every five minutes. When a change in pinprick testing, such as reported pain sensation, occurred, or a drop in skin temperature > 0.5°C between two consecutive measurements was detected, the measurement frequency was increased to every two minutes. The predefined temperature cut-off value of 0.5°C was set to prevent a true temperature decrease from being overlooked while taking into account that minor temperature fluctuations could be due to measure- ment uncertainties. A maximum allowable error of the temperature probe of less than 0.005%/°C was reported by the manufacturer. When no sensorial change between the 2nd and 5th phalanx was indicated by the subject based on pinprick testing, pinprick testing was stopped. Tempe- rature measurements were continuously recorded every two minutes for a period of 16 minutes, after which the experiment was terminated. The 16-minute limit was selected based on experiences from a prior, unpublished study conducted by one of the authors. The final dataset was constituted by the lowest skin temperature recorded. During this period, it was anti- cipated that the block would subside to such an extent that any subsequent increase in temperature could be attributed to external influences and further measure- ments were deemed redundant for the experiment. Fixed points, T0–T5, were selected based on changes in pinprick testing and/or temperature measurements. T0–T5 were defined as: T0 - “Application of UNB”, T1 - “Onset of UNB” (loss of pain sensation), T2 - “Average temperature plateau”, T3 - “Reduced pain sensation”, T4 - “Full regain of pain sensation” and T5 - “Ended test”, and were graphically delineated with time points individually adjusted to count from the time of UNB administration. Additionally, an X, indicating the last temperature plateau measurement, was portrayed. The temperature plateau was assessed clinically when repeated measurements were found to be stable. A time window from X–T3, that is, from the last temperature plateau measurement to reported reduced pain sensation, is illustrated by a shaded area under the graph.
2.4. Statistical Analyses
No formal sample size estimation was made, as this was a pilot preliminary study and was not designed to hold power for detailed statistical comparison. The number of subjects was set at five, with a total of 10 UNBs included, to observe the relationship of the temperature course following a peripheral ulnar nerve block. It is suggested that conclusions be validated through further studies. If a subject was excluded from the study, a new subject was invited to participate in order to obtain a full dataset of five subjects.
The relationship between temperature and nerve block duration is graphically presented. Due to the limited number of participants, the time of UNB and temperature were described with median, range, and confidence intervals (CI). The 95% CI was estimated using the binomial method. Statistical analyses were conducted using STATA17 (StataCorp LCC, Texas, USA).
3. RESULTS
A full set of data was obtained, including 10 successful UNBs, involving four men and one woman aged 22 to 38. Pain sensation persisting beyond 45 minutes was reported by a sixth subject, leading to their exclusion from the analyses. The unsuccessful nerve block was attributed to a failed administration of anesthesia. No significant adverse events were reported following the application of the UNBs, and full sensibility was subsequently regained by all the subjects.
The 10 UNBs are individually shown in Fig. (1), with each block illustrated separately for the right and left hand of each subject and depicted graphically alongside the associated control measurements.
Values related to Fig. (1) are mentioned in Table 1.
The effective duration of the ulnar nerve blocks, from the onset to reported reduced pain sensation (T1–T3), was 89.5 minutes (Table 1). A notably different sensation was reported by subject D throughout the block of the left hand, which was characterized by a loss of pain sensation (T1) prior to a detectable temperature increase and a deviating short temperature plateau phase, as shown in Fig. (1). From the application of UNB (T0) to the onset (T1), an increase in temperature was observed in nine out of ten UNBs. A maximum temperature increase was attained in the successive minutes following onset (T1) as the temperature reached the plateau phase (Fig. 1). All 10 UNBs reached a temperature plateau phase following onset within a median time duration of 20 minutes (range 5–25) and with a median temperature increase of 3.0°C (range 0.3–10.4).
| - | A - Right | A - Left | B -Right | B - Left | C - Right | C - Left | D - Right | D - Left | E - Right | E - Left | Median | Range |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tp (C), T0 | 32.2 | 29.1 | 24.4 | 27.6 | 30.4 | 27.4 | 28.1 | 24.3 | 29.4 | 28.1 | 28.1 | [24.3-32.2] |
| Tp (C), T1 | 34.3 | 32.9 | 31.2 | 32.8 | 32.6 | 28.3 | 30.5 | 23.6 | 30.1 | 31.2 | 31.2 | [23.6-34.3] |
| Tp (C), T2 | 34.7 | 34.2 | 34.7 | 34.6 | 34.2 | 33.9 | 33.7 | 34.0 | 34.0 | 34.2 | 34.2 | [33.7-34.7] |
| Tp (C), T3 | 33.4 | 34.1 | 33.3 | 33.4 | 33.6 | 32.8 | 29.6 | 33.4 | 32.3 | 33.6 | 33.4 | [29.6-34.1] |
| Tp (C), T4 | 33.6 | 31.8 | 32.2 | 32.2 | 34.0 | 29.0 | 25.3 | 32.3 | 28.9 | 27.2 | 32.0 | [25.3-34.0] |
| Tp (C), T5 | 32.6 | 30.8 | 26.9 | 30.2 | 30.4 | 27.7 | 23.7 | 31.3 | 28.9 | 25.7 | 29.6 | [23.7-32.6] |
| T1 – T3 (min) |
105 | 103 | 143 | 85 | 60 | 43 | 63 | 35 | 107 | 94 | 89.5 | [35-143] |
| X-Tp (C), (X- T3) |
0.5 | * | 1.4 | 1.2 | 0.6 | 1.1 | 4.1 | 0.6 | 1.7 | 0.6 | 1.1 | [0.5-4.1] |
| X -T3 (min) | 25 | * | 43 | 20 | 30 | 13 | 18 | 5 | 20 | 19 | 20.0 | [5-43] |
A median temperature of 34.2°C was observed during the temperature plateau phase (T2) (Table 1). A narrow range of only 1.0°C was noted within the plateau phase, with minimal temperature fluctuations observed compared to the control hand’s measurements. Where a temperature decrease was detected within the plateau phase, a corresponding fluctuation was typically observed in the control hand.
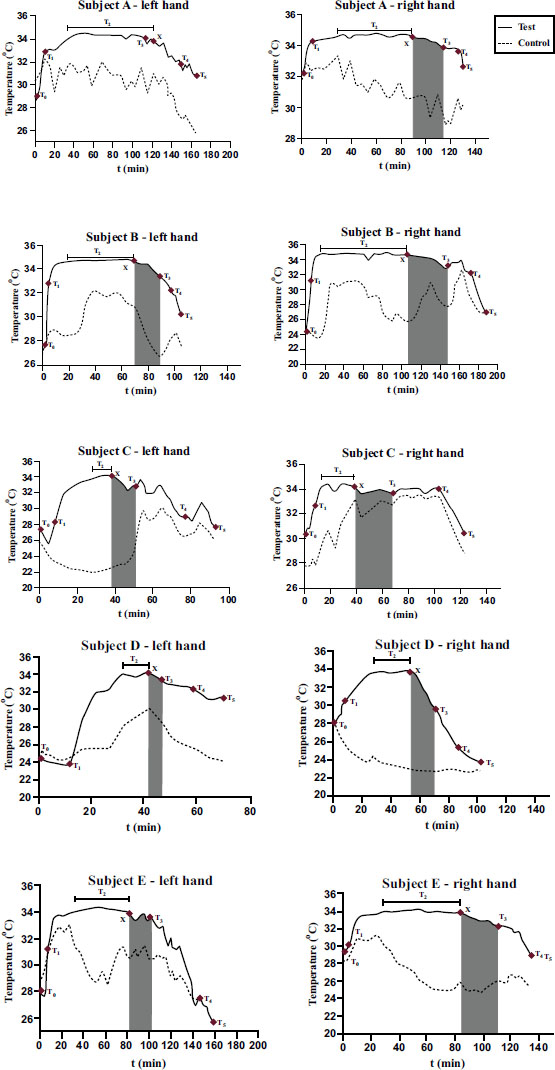
Individual temperature profiles for each subject are divided into the right and left hand with associated fixed points (T0-T5), adjusted to count from the ulnar nerve block (UNB) administration. The tested hand is marked with a full line, while the control hand is marked with a dotted line. A marked area under the graph indicates a time window from the last temperature plateau measurement to the reported reduced pain sensation (X-T3). Pain sensation prior to the last temperature plateau measurement was indicated by subject A’s left hand, and therefore, no area under the graph was marked. T0 represents the application of UNB; T1 represents the onset of UNB; T2 represents the average temperature plateau; T3 represents reduced pain sensation; T4 represents full regain of pain sensation; T5 represents the ended test; and X represents the last temperature plateau measurement.
In two out of ten UNBs, a temperature decrease of 0.8°C was observed during the plateau phase in subject B’s right hand, which was matched by an equivalent decrease of 0.8°C in the control hand. Similarly, in subject C’s right hand, a decrease of 0.6°C was observed, along with a corresponding decrease of 0.8°C in the control hand. However, in the remaining eight UNBs, temperature fluctuation in the plateau phase never exceeded 0.5°C between any two contiguous measurements.
By the final temperature measurement of the temperature plateau phase (X), a steady temperature decrease was observed prior to the reported reduced pain sensation in nine out of ten UNBs, with the exception of subject A’s left hand, where pain sensation was indicated prior to a temperature decrease. For subject D’s right hand, a notably larger temperature decrease of 4.1°C was observed. A median temperature decrease of 1.1°C from X–T3, the last temperature plateau measurement prior to reduced pain sensation, was observed in nine out of ten UNBs, with a median time duration of 20.0 minutes (Table 1). The median temperature with confidence intervals for the five timepoints (right and left hands combined) is presented in Table 2.
No overlaps of CIs were found between the test and control hands in T2 and T3 (combined left and right hands) (Table 2).
| Left and Right Hands Combined | Median | Range | 95% - CI |
|---|---|---|---|
| T0 – (test) T0 – (control) |
28.1 28.1 |
24.3 – 32.2 24.1 – 31.4 |
25.4 – 30.1 25.2 – 29.8 |
| T1 – (test) T1 – (control) |
31.2 28.2 |
23.6 – 34.3 23.3 – 32.5 |
28.9 – 32.9 25.4 – 30.1 |
| T2 – (test) T2 – (control) |
34.2 29.5 |
33.7 – 34.8 22.0 – 31.6 |
33.9 – 34.8 24.3 – 31.5 |
| T3 – (test) T3 – (control) |
33.4 28.2 |
29.6 – 34.1 22.8 – 32.7 |
32.5 – 33.8 25.7 – 30.2 |
| T4 – (test) T4 – (control) |
32.0 27.1 |
25.3 – 34.0 22.8 – 33.4 |
27.8 – 32.2 25.5 – 30.1 |
| T5 – (test) T5 – (control) |
29.6 25.9 |
23.7 – 32.6 22.8 – 30.2 |
26.1 – 31.1 24.5 – 28.4 |
4. DISCUSSION
In this exploratory observational study on healthy volunteers, the temperature profile following a peripheral ulnar nerve block was examined. An initial increase in temperature was observed, followed by a plateau phase during which the elevated temperature indicated that a successful nerve block had been achieved. This plateau phase was succeeded by a steady decrease in temperature before the reported return of pain sensation in nine out of ten UNBs. This is suggested as indicating a time window during which temperature may serve as an indicator of declining nerve block efficacy in clinical practice.
Temperature changes following a peripheral nerve block of the upper extremity have been examined in a limited number of studies. Skin temperature following an infraclavicular plexus block was evaluated in previous studies by Minville et al. [8] and Asghar et al. [1] A stat- istically significant temperature increase was found prior to the sensory block, with a temperature increase > 1°C being identified as a reliable early indicator of a successful nerve block. In another study [9], skin temperature following an interscalene brachial plexus block was evaluated, where statistically significant temperature increases were found with the median, ulnar, and radial nerves. However, it was found that only 9% of the temperature increases occurred before sensory loss, suggesting that skin temperature may have limited clinical value as an indicator of a successful nerve block. In the present study, a temperature increase was achieved by all 10 UNBs, with an average plateau phase (T2) and no confidence interval (CI) overlap between intervention and control measurement, indicating that a successful nerve block was attained. Overlapping CIs between intervention and control temperature measurements were found from the onset of sensory loss (T1), suggesting that temperature may not be superior to pinprick testing for indicating a successful ulnar nerve block during early onset.
In another study conducted by Lange et al. [7], skin temperature was investigated following the specific blocking of the median and ulnar nerves of the upper extremity, and a statistically significant temperature increase was found. A mean maximum temperature increase of approximately 5°C was observed following the blocking of the peripheral ulnar nerve, with a mean duration of 22 minutes recorded. The results were found to align with those of the present study, where a temperature plateau was reached by all 10 UNBs, with a median maximum temperature increase of 3.0°C and a median duration of 20 minutes. These findings indicated a maximal vasodilation following a sufficient block.
A review by Hermanns et al. [10] reported a temperature decrease following nerve block adminis- tration before a substantial increase occurred. This phenomenon was observed in half of the blocks in this study and was particularly noticeable in subject D’s left hand (Fig. 1). It may be attributed to an initial increase in sympathetic activity, though this remains uncertain.
To our knowledge, no previous studies have examined the further course of temperature following peripheral nerve blocks in detail. In the present study, a temperature plateau phase was observed in all 10 UNBs, with a median temperature of 34.2°C and a narrow range, suggesting a physiological plateau with limited variation across individuals. During the plateau phase, the temperature was only slightly affected, and significant fluctuations in two contiguous temperature measurements were most likely indicative of a declining block.
Following the temperature plateau phase, a median temperature decrease of 1.1°C with a median time duration of 20.0 minutes was observed in nine out of ten UNBs, suggesting that temperature may serve as an objective method to deduce a declining block in clinical practice.
At T3, no overlap of CI was found between the test and control hands, indicating an influence on temperature caused by the local anesthetics. However, as the anesthetic effect diminished and pain sensation was detected via pinprick testing, larger temperature fluc- tuations were observed in both the control and test hands, likely due to the cessation of sympathetic nerve blockade. As a result, skin temperature measurements may lose clinical relevance once pain sensation returns. A possible limitation of the study is the relatively short acclimatization period of 10 minutes, which may have contributed to the observed differences in baseline temperature values between the right and left hands. Despite this, the overall temperature course of the control hands is believed to provide insight into general temperature fluctuations over time, and its impact on the results is considered limited.
The strengths of this study are demonstrated through the consistent use of pinprick testing by the same operator, the multiple measurements taken, and the selection of an appropriate temperature gauge. Skin surface temperature probes were utilized, which are widely available in hospital wards, easy to use, and interpretable by various healthcare professionals.
A key limitation of the study is the relatively small sample size. This was considered acceptable as the study design was exploratory and hypothesis-generating rather than comparative. Another limitation is the calculated average temperature plateau phase, with measurements being based on a subjective clinical assessment of when a plateau was, rather than on pre-set cut-off values. However, since no established reference is known to exist, an assessment is deemed necessary to estimate a true value for the plateau. The pinprick testing also presented a limitation. As the block began to subside, it became evident that differentiating between pain and touch sensations was difficult for all subjects. Subject A experienced particular difficulty, reporting a pain sensation in the blocked left hand before a temperature decrease was detected. In subsequent pinprick tests, both pain and no pain sensations were reported.
Overall, a pain sensation was indicated before the temperature decrease in only one out of ten UNBs. In future studies, it would be desirable for the relationship between temperature and pain sensation to be tested in postoperative patients, thereby eliminating the uncertainty of the pinprick testing. A possible limitation relates to the execution of the experiments on non-fasting subjects, as feeding may influence microcirculation and, thus, temperature measurements. However, this choice was intentionally made to reflect a postoperative temperature course in patients undergoing minor operations with local anesthesia, as well as those needing postoperative blocks, who are typically non-fasting. The choice of the applied local analgesic may also be considered a limitation. Lidocaine is commonly used in minor surgeries, whereas long-acting local anesthetics, such as bupivacaine and ropivacaine, are more frequently used in peripheral nerve blocks [13]. However, because their physicochemical properties are similar [13, 14], a comparable physiological response was expected and therefore considered transferable.
CONCLUSION
In this study, temperature was increased, and a plateau phase was reached, which might be related to a successful nerve block. A clinically significant time window in which temperature was decreased after the plateau phase, prior to the return of pain sensation, was observed. It is suggested that temperature could be used to deduce a declining nerve block, which might be considered valuable in clinical practice if similar findings are applied to postoperative patients. In such cases, it would be possible for pain medication to be administered or a new block to be applied to address issues such as rebound pain. However, further studies are needed to confirm the tendencies indicated by this study.
AUTHORS’ CONTRIBUTION
A. D. B.: Took part in writing the manuscript; K. L. V.: Carried out data analysis or interpretation; M. A. S.: Collected the data; C. G.: Contributed to the concept or design of the study; H. I. J.: Provided guidance.
LIST OF ABBREVIATIONS
| CI | = Confidence Intervals |
| UNB | = Ulnar Nerve Block |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Regional Committees on Health Research Ethics for Southern Denmark, Denmark (jf. No. S-20200081-CSF).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [A.B] upon reasonable request.
FUNDING
This study was funded by the Department of Anesthesiology and Intensive Care, Vejle Hospital, Vejle, Denmark.
ACKNOWLEDGEMENTS
The authors would like to thank the volunteers who participated in this study, as well as to the staff at the recovery unit. They would also like to thank Chief Physician, Lisbet Tokkesdal Jensen, for providing the opportunity to conduct this study at the Department of Anesthesiology and Intensive Care, Vejle Hospital.


