All published articles of this journal are available on ScienceDirect.
Multiple Risk Factors Analysis of Post-dural Puncture Headache (PDPH) among Parturient Patients Underwent Caesarean Section at Obstetric Hospitals in Somaliland
Abstract
Background
Regional anesthesia, particularly spinal technique, is administered during obstetric surgery. The patient and the procedure have risk factors that affect the likelihood of post-dural puncture headaches (PDPH). This study aimed to assess multivariate statistical analyses of risk factors that predict PDPH occurrence in patients who underwent Caesarean section in an obstetrics hospital in Somaliland.
Methods
A cross-sectional study was designed and conducted in obstetrics-selected hospitals in Somaliland. Four hundred parturient patients were included. Statistical tests included Chi Squire and risk analysis (Odd & Risk relative ratios) and the Receiver Operating Characteristic (ROC) curve was used to analyze sensitive risk factors to predict PDPH occurrence.
Results
The results revealed that 325 parturient patients (81.25%) developed PDPH while 75 parturient patients (18.75%) didn’t report PDPH; multiple lumbar puncture attempts were significantly associated with an increased risk of PDPH, with a P-value of 0.001 and an odds ratio (OR) of 2.705 (95% CI: 1.588–4.605). The ROC analysis for these attempts showed an area under the curve (AUC) of 62%, indicating that the sensitivity and specificity of lumber puncture attempts (56%, 32%) to predict PDPH. However, other risk factors (Age, PMI, Needle type & size, patient’s position) indicate weak predictive value for PDPH occurrence.
Conclusion
The study concluded that Lumber puncture attempts were a significant risk factor in predicting PDPH compared to other. However, the other risk factors were reported as weak, sensitive and specificity risk factors to predict PDPH occurrence.
1. INTRODUCTION
Cesarean section (CS) under spinal anesthesia has advantages such as allowing the mother to stay conscious throughout the procedure, minimal depression of the fetus, small drug dose, low failure rate, rapid onset, and simplicity of the technique. Therefore, since 2001, performing CS under spinal anesthesia has become a popular and preferred method of general anesthesia [1, 2].
A frequent and uncomfortable complication of spinal anesthesia is post-dural puncture headache (PDPH). It is a throbbing pain on both sides of the head in the front-back area that arises five days after a dural puncture. The pain can get worse with activities that increase pressure in the head, such as sneezing, coughing, pushing, and sudden movements, but resting down can alleviate the pain a bit within 15 minutes [3]. When the needle punctures the dura and causes a hole, cerebrospinal fluid (CSF) can escape rapidly through it, which lowers the pressure inside the skull and leads to post-dural puncture headache (PDPH). Signs of PDPH include feeling dizzy, having a stiff neck, being sensitive to light, seeing double, feeling nauseous, and throwing up [4]. With good rest, fluids, and painkillers, within 48 hours [5], these signs usually diminish in a week. Some factors increase the chance of obstetric patients getting PDPH, such as age, weight, pregnancy, or previous headaches or migraines. The likelihood of PDPH also varies with the needle's type and size, how it is inserted, how many tries it takes, and how much CSF fluid is lost during the procedure [6]. Needles with pencil-point tips (Sprotte or Whitacre) that are 25F to 27F in size produce fewer PDPH than needles with Quincke cutting tips because their tips are blunter and narrower. Thus, the needle size and type are the main determinants of PDPH, and using a smaller needle diameter significantly lowers the PDPH risk [7]. The study aims to determine the sensitivity and specificity of different risk factors for PDPH prediction in obstetric patients with spinal anesthesia. There is not much information on some aspects, such as the number of pregnancies. The incidence and risk factors of PDPH after different neuraxial anesthesia methods are still being researched. Moreover, those studies do not concentrate on specific risk factors' sensitivity, specificity, and risk analysis that can predict the occurrence of PDPH.
Following the administration of regional anesthesia, the patient and the procedure tend to have risk factors that affect the likelihood of post-dural puncture headaches, particularly spinal anesthesia. Factors that affect the risk represent the needle's characteristics and how often the lumbar puncture is attempted, age, BMI, and headache history, including post-dural puncture headache. The goal of the study was to ascertain, which had not been documented in prior studies, the sensitivity-specificity risk factors analysis that can predict the incidence of PDPH. One study found that PDPH can result from different spinal surgeries and neuraxial anesthesia combinations, and some risk factors are known. How often these risk factors affect PDPH after various treatments is not well-studied [8]. Thus, the study identified the main risk factors in multiple analyses to forecast the PDPH incidence that are accurate and precise, using a method based on scientific evidence that could lower PDPH in the future.
2. METHOD
2.1. Study Design and Participants
In this cross-sectional study, 400 parturient patients underwent cesarean section and were anesthetized by spinal anesthesia at Hargeisa Group Hospital, Gargaar Multi-specialty, and Kaah Community Hospitals from July 2023 to June 2024. Parturient patients aged between 17 to 45 years were included and were categorized according to the activity of reproduction to group age [(17- 29 years) with a peak of fertility, group (30-35 years) decreased fertility, and group (greater than 35 years) as declined fertility and reproduction] [9, 18]. Maternal patients ASA class I - II were planned for scheduled caesarean sections during the period of study.
2.2. Ethical Considerations
This study was approved by the Department of Planning/Policy and Strategic Information, National Ethical Committee, along with a unit of research development, ministry of Health Development, Republic Somaliland (Project ref: MOHD/DG:2/1246/2023).
2.3. Setting and Study Size
400 Parturient patients underwent cesarean section and were anesthetized by spinal anesthesia at Hargeisa Group Hospital, Gargaar Multi-specialty, and Kaah Community Hospitals, which were conducted from July 2023 to June 2024. Patients admitted to the hospital for spinal anesthesia during the data collection period were included in the study. The sample size was calculated based on the formula for unmatched case-control studies.
Formula for Sample Calculation: N=Z^2Pq/e^2
N = sample size
Z = Number of patients admitted for LSCS under spinal anesthesia Pq = Variance of population
E = Allowable error 5%
N= Maternal patients
2.4. Technique of Spinal Anesthesia
Spinal anesthesia was performed by injecting 12-15 mg of Bupivacaine 0.5% isotonic at L3-L4 according to the weight. The spinal needle size ranging from 25, 26, and 27 G was used during anesthesia and most of the patients were given anesthesia in a sitting position respective to the lateral. Two types of spinal needles were used for the lumber puncture technique, including pencil point and quincke tip and patient vital signs were monitored by standard anesthesia monitors during the intra-operative and postoperative periods.
2.5. Variables, Data Sources/measurement, and Bias
Demographic data and consent regarding parturient patients were collected preoperatively in antenatal wards through parameters of risk factors of post-dural puncture headache (spinal needle type, size, and attempt of lumber puncture intra-operatively) from anesthesia records and anesthesia team and postoperatively after 24 to 3 days by stranded questionnaire from the patients in postnatal wards.
This data was collected by a team of trained anesthesia practitioners in the hospitals included in this study. Data for this research was acquired through a questionnaire and is stored safely in an online database in an Excel spreadsheet available upon request.
Data was collected equally and confidentially from the hospital selected in the study.
2.6. Quantitative Variables
This study included 400 parturient patients who underwent cesarean section under spinal anesthesia and the study reported that 325 (81.25%) patients developed PDPH and 75 (18.75%) patients did not (Fig. 1).
2.7. Statistical Methods
SPSS program version 26.0 was used for statistical analysis. Nominal variables are presented as frequencies and Chi squire tests were used for the comparison of categorical variables between groups. P value ≤ (0.05) was expressed as significance level, and risk analysis of risk factors by Odds ratio & Relative risk ratio with 95% CI was measured and sensitivity and specificity estimated by Receiver Operating Characteristics (ROC) curve analysis cut-off value area under the curve of results parameter. The results were considered positive if there were less or equal cut-offs or negative when there were more cut-off values and results were presented in tables and figures.
3. RESULTS
3.1. Participants
In this study, 400 patients were included who underwent cesarean section under spinal anesthesia. It was found that 325 (81.25%) patients developed PDPH and 75 (18.75%) patients did not (Fig. 1).
3.2. Descriptive Data
The patient risk factors were grouped into two age groups according to fertility: group age 17- 29 years with peak fertility and group age 30- 35 years with decreased and declined fertility. The age group increased the risk of PDPH by 1.377 times, body mass index increased the PDPH (normal and obese) by 1.753 times, needle type by 1.628 times, and needle size (25G or larger) increased the risk of PDPH by 1.409 times. Patient position (sitting vs. lateral) reduced the risk of PDPH by 0.451 times. Additionally, lumbar puncture attempts were associated with a 2.705 times higher risk of PDPH, as shown in Table 1.
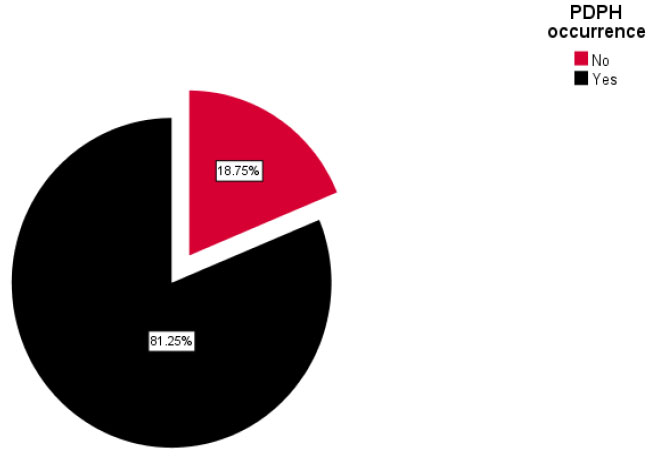
Shows the postdural puncture headache occurrence among parturient patients in obstetric hospitals in somaliland.
| Risk Factors of PDPH | Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|
| Lower | Upper | ||
| Age group (17 - 29 & 30-45 years) | 1.377 | 0.824 | 2.300 |
| Body Mass Index (BMI) (Normal weight / Obese) | 1.753 | 0.334 | 9.216 |
| Spinal Needle type (Quincke tip / Pencil tip) | 1.268 | 0.472 | 3.411 |
| Needle size (25 G / > 25 G) | 1.409 | 0.780 | 2.545 |
| Position (Sitting & Lateral Position) | 0.451 | 0.110 | 1.848 |
| Lumbar Puncture attempt (1st attempt / More attempts) | 2.705 | 1.588 | 4.605 |
| Risk Factors of PDPH (Patient Factors) | PDPH Occurrence | P-value | Relative Risk Ratio | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| No (%) | Yes (%) | Lower | Upper | |||
| Age group (17-29 Yrs) |
46 (20.9) | 174(79.1) | 0.24 | 1.146 | 0.932 | 1.408 |
| Age group (30-35years & >35 years) | 29 (16.1) | 151(83.9) | 0.832 | 0.612 | 1.132 | |
| Body Mass Index (BMI) Normal weight | 2(28.6) | 5(71.4) | 0.50 | 1.733 | 0.343 | 8.763 |
| Body Mass Index (BMI) Obese | 73(18.6) | 320(81.4) | 0.989 | 0.950 | 1.029 | |
| Setting Position | 72 (20.3) | 319 (79.7) | 0.25 | 0.978 | 0.932 | 1.027 |
| Lateral Position | 3 (33.3) | 6 (66.7) | 2.167 | 0.554 | 8.467 | |
| Risk Factors of PDPH (Technique Factors) | PDPH Occurrence | P-value | Relative Risk Ratio | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|
| No (%) | Yes (%) | Lower | Upper | |||
| Spinal needle (Quincke tip) | 70 (19.0) | 298 (81.0) | 0.63 | 1.217 | 0.530 | 2.798 |
| Spinal needle (Pencil tip) | 5(15.6) | 27(84.4) | 0.960 | 0.820 | 1.123 | |
| Spinal Needle Size (25 G) | 58 (77.3) | 230(70.8) | 0.25 | 1.093 | 0.949 | 1.258 |
| Spinal Needle Size (> 25 G) | 17(22.7) | 95(29.2) | 0.775 | 0.494 | 1.217 | |
| Lumbar Puncture (1st attempt) | 51(68.0) | 143(44.0) | 0.001 | 1.545 | 1.268 | 1.884 |
| Lumbar Puncture (Multiple attempts) | 24 (32.0) | 182 (56.0) | 0.571 | 0.405 | 0.806 | |
3.3. Outcome Data, Main Results, and Other Analyses
The results of the current study revealed that there were no significant changes (P value 0.24) of PDPH occurrence between age groups; however, the age group 17-29 years reported a greater risk ratio of PDPH (1.146) compared to age group 30-45 year, which reported 0.832, BMI also reported no significant changes of PDPH for normal and obese patients (P value 0.50, RR 1.733 & 0.989) and both setting and lateral positions were detected to have no significant changes (P vale 0.25) and slightly increased of relative risk ratio in lateral position 2.167 respective to other position have shown in Table 2A.
The results of the current study revealed that there were no significant changes (P value 0.63) in PDPH occurrence related to needle types; however, quincke tip spinal needle statistically reported slight increases in the PDPH occurrence and risk ratio (1.217) compared to pencil tip (0.960). Spinal needle size 25G reported slight statistical increases in the PDPH occurrence and risk ratio (81% RR ratio 1.217) compared to other spinal needle sizes but there was a significant association. However, lumber puncture attempts reported a significant elevation of PDPH occurrence with multiple attempts compared to the first attempt have shown in Table 2B.
The result variable(s): Age, Body Mass Index (BMI), and position have shown area under the curve. Age group 53% (weak), sensitivity 45%, specificity 38%, ROC curve cut off for the BMI is 52% (weak), the result area under a curve of Position 0.48 (48%) (weak) as shown in Fig. (2).
3.4. Study Design and Participants
Regarding the ROC curve, the cut-off value of LP attempts (AUC, the area under the curve is 62%) sensitivity of 56% and specificity of 32%. LP attempts result is considered positive if it is less or equal cut-off or negative when there are more cut-off values. The ROC curve cut-off value area under the curve of needle type and needle size is 50% and 53% (Weak). The results of needle type and size are considered positive if it is less or equals the cut-off or negative when there are more cut-off values shown in Fig. (3).
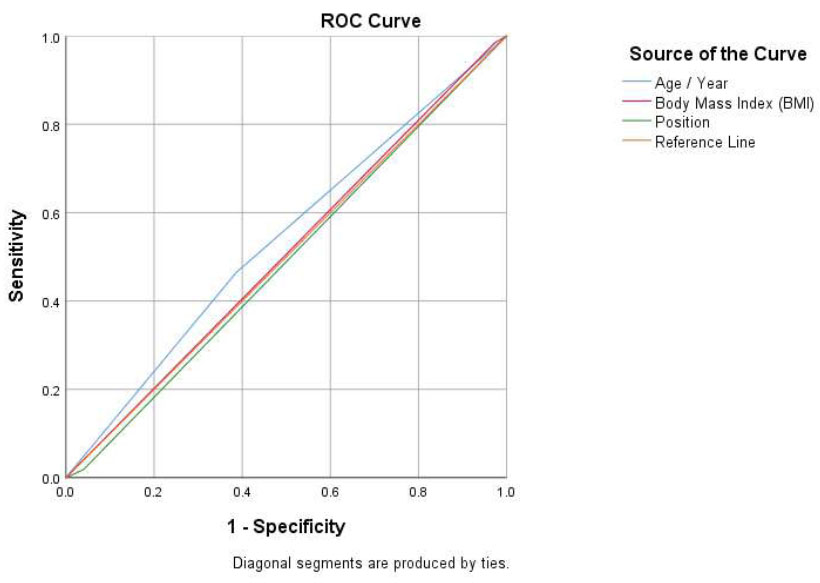
Receiver operating characteristics (ROC) of the age, body mass index (BMI), and position of parturient patients.
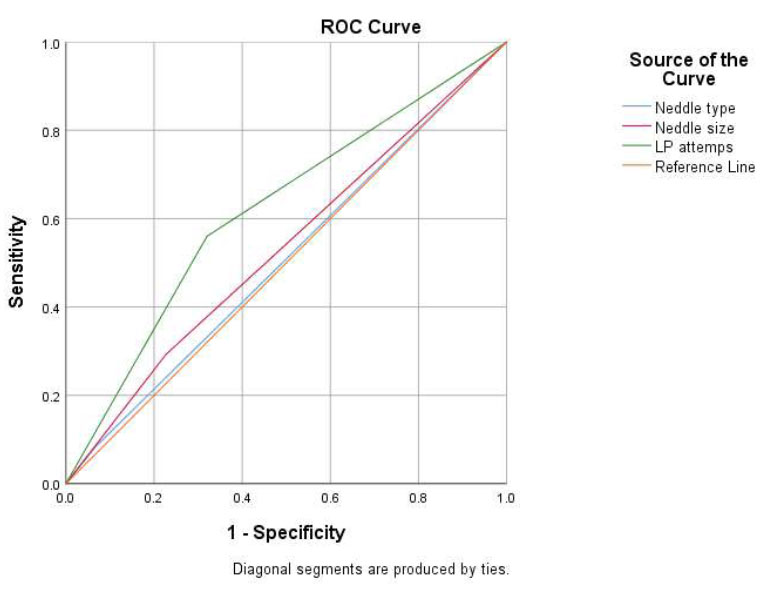
Receiver operating characteristics (ROC) of the needle type, needle size, and lumber puncture attempts of parturient patients.
4. DISCUSSION
PDPH is a common complication of neuraxial anesthesia that develops primarily after puncturing the dura mater, causing a CSF leakage, which results in intracranial hypotension [10]. Multiple reports of research documented the risk factors that influence PDPH occurrence, including patient’s risk factors (age, BMI, ASA classification, gestational age, urgency of surgery, previous PDPH, parity, and gravidity) [11] and technique’s risk factors (needle type, needle gauge, number of attempts, and direction of bevel) [12].
4.1. Key Results
The purpose of this study, which involved 400 parturient patients who underwent caesarean sections, was to assess the multivariate statistical risk analysis to predict highly sensitive and specific risk factors in developing post-dural puncture headache (PDPH) following spinal anesthesia. Ljubisavljevic et al., and Al-Hashel et al., reported that younger patients had a higher chance of developing PDPH compared to older patients; the possible cause could be related to less CSF production and elastic dura matter [13, 14] and these findings agree with our results which reported that patients between 17-29 years have higher PDPH occurrence when compared with other age groups.
The current results did not detect a significant association between BMI and PDPH occurrence in parturient patients. However, many studies reported that a BMI greater than 30 kg/m2 had a significant association with the incidence of PDPH [11, 13, 15].
This study reported that there was no significant association between patient positions during lumber puncture, needle types and size relevant to PDPH occurrence; however, the relative risk factors statistically were detected between lateral and setting position and different needle sizes to increase risk of PDPH occurrence. The decrease of spinal size to less than 27G for cesarean section reduced PDPH incidence [16]. Moreover, the previous randomized trial reported the incidence of PDPH with needle-type Quincke was 22.43% [17].
The current study detected that spinal needle size 25G reported slight statistical increases in the PDPH occurrence and risk ratio (RR: 1.093; 95% CI =0.949-1.258) compared to other sizes. A smaller needle size reduces the risk of CSF leakage and PDPH when piercing the dura mater [19, 20]. A 27G is better than 25G, as two studies showed less PDPH with 27G (p<0.05) [21, 22]. A similar study also showed that PDPH was more common with 20G and 22G needles than with 24G and 25G (AOR = 4.206; 95% CI = 1.247–14.187; p = 0.021), which matches our findings [23].
The findings of this study confirm that the technique-related risk factors, lumber puncture attempts reported significant increases in PDPH occurrence with both first and multiple attempts and (sensitivity 56% specificity 32% and significant P value 0.001, OR 2.705 95% IC 1.588-4.605) increased incidence and risk of PDPH occurrence. However, higher incidence reported during multiple attempts in the current results. Every time the dura matter is penetrated, there is more CSF loss and a greater risk of CSF hypotension and PDPH [24]. This is consistent with multiple studies that associate the frequency of dura matter punctures with the occurrence of PDPH, such as Wegi Girma et al., who report that PDPH occurrence increases 1.5 times with multiple attempts (P= 0.001) [11]. Another statement from Demilew BC et al. is that the chance of PDPH increases 4.7 times with repeated punctures of the dura matter (P = 0.05).
CONCLUSION
This study concluded that multiple analyses reflected that Lumber puncture attempts, particularly multiple attempts, were significant potential risk factors that can predict post-dural puncture headache. However, other factors detected weak sensitivity and specificity.
LIMITATIONS
The study's limitations are that awareness of preoperative consent is not applicable in most hospitals in Somaliland as a mandatory protocol in theater. The limited appropriate quality of technique.
WHAT IS ALREADY KNOWN ABOUT THIS TOPIC
PDPH is a frequent and uncomfortable complication of spinal anesthesia, characterized by throbbing pain on both sides of the head.
Risk Factors: Factors such as age, gender, weight, pregnancy, previous headaches, needle type and size, insertion technique, and number of lumbar puncture attempts influence the likelihood of PDPH.
WHAT THIS STUDY ADDS
High Incidence of PDPH: 81.25% of the participants developed post-dural puncture headache (PDPH) after undergoing a Caesarean section with spinal anesthesia.
Significant Risk Factor: Multiple lumbar punctures attempt significantly increased the likelihood of PDPH occurrence.
Needle Characteristics: The type and size of the needle used in spinal anesthesia play a crucial role in the risk of developing PDPH.
Predictive Analysis: The study used statistical methods like Chi-square, odds ratios, and ROC curves to analyze and predict PDPH risk factors.
AUTHOR’S CONTRIBUTION
H. S., M. A., M. S. B., M. F., P. K. K. and G. M.: Wrote the paper; K. A. and O. S.: Data analysis or interpretation were contributed; E. S. H. G.: Collected the data; S. M. A. E.: Provided the study concept and design.
LIST OF ABBREVIATIONS
| PDPH | Post-dural Puncture Headache |
| ROC | Receiver Operating Characteristics |
| BMI | Body Mass Index |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Department of Planning/Policy and Strategic Information, National Ethical Committee, along with a unit of research development, ministry of Health Development, Republic Somaliland (Project ref: MOHD/DG:2/1246/2023).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Demographic data and consent regarding parturient patients were collected preoperatively in antenatal wards.


