All published articles of this journal are available on ScienceDirect.
Validity of Lung Ultrasound Score and Inferior Vena Cava Diameter Compared to Pulse Pressure Variation Predicting Fluid Responsiveness in Mechanically Ventilated Critically Ill Patients: A Comparative Study
Abstract
Background
The assessment and regulation of intravascular volume provides a significant problem for critically ill cases.
Aim
This study aimed to evaluate the efficacy of IVC and lung ultrasonography compared to pulse pressure differences in expecting fluid responsiveness in cases mechanically ventilated with circulatory failure.
Methods
The research has been performed on 150 cases in the ICU of Fayoum University Hospitals with permission from the local institutional ethical committee and the local institutional review board (D 310).
Results
A statistically significant variance has been observed among fluid responders and fluid non-responders with p-value < 0.05 regarding delta lung B lines, inferior vena diameter during both inspiration and expiration, inferior vena cava distensibility index, and pulse pressure variation, while there was a statistically insignificant variance regarding lung B lines, heart rate, central venous pressure, urine output, serum lactate, and ICU stay with p-value more than 0.05. Additionally, the area under the Receiver-Operating Characteristic (ROC) curve and the p-values for various hemodynamic and ultrasound variables were investigated. Variables with p-values fewer than 0.05 (statistically significant) have been shown their sensitivities (true positive), specificities (true negative), and best cut-off values.
Conclusion
Pulse pressure variation, lung ultrasound, and inferior vena cava distensibility index have a predictive value for fluid responsiveness with high specificity and sensitivity.
Clinical Trial Registration Number
This study is registered on ClinicalTrials.gov (NCT05980494; principal investigator: Mohamed Ahmed Hamed; date of registration: July 31, 2023).
1. INTRODUCTION
The assessment and intravascular volume control provide a significant difficulty for critically ill cases. Hypotensive cases are frequently resuscitated using IV crystalloid fluids as a suggested therapy for various shock conditions [1].
Over the last ten years, there has been an enhancing interest in the use of Lung Ultrasound Scans (LUS) in critical care management due to its simplicity, bedside access, cost-effectiveness, noninvasiveness, and absence of radiation [2].
LUS can identify pleural effusions, pneumothorax, pulmonary edema, and consolidation [3]. Furthermore, it may enhance the clinical management of circulatory failure and shock, with the component of the lung becoming an essential element of the overall case evaluation. Furthermore, it was associated with the severity of Acute Respiratory Distress Syndrome (ARDS) and serves as a predictor of death [4].
Measurements of ultrasound of the inferior vena cava were suggested as a method to assist with management options of fluid. Established associations exist among respiratory cycle-induced variations in the diameter of the inferior vena cava and Central Venous Pressure (CVP) [5].
Pulse Pressure Variation (PPV) quantifies the disparity between the minimum and maximum pressure throughout a respiratory cycle, separated by their means. It is seen as a dynamic parameter resulting from variations in intrathoracic pressure throughout Mechanical Ventilation (MV). Positive pressure can reduce the Right Ventricle (RV) preload and elevate the RV afterload, hence lowering right heart stroke volume throughout inspiration. The preload to the Left Ventricle (LV) is subsequently diminished, resulting in a reduction of left heart stroke volume. Variations in stroke volume in the left-sided are amplified on the steep segment of the Frank-Starling curve, making pulse pressure alteration a potential predictor of volume responsiveness [6].
This investigation aimed to evaluate the inferior vena cava efficacy and lung sonography than PPV in the responsiveness of predicting fluid in MV cases with circulatory failure.
2. METHODS
The research has been performed on 150 cases in the ICU of Fayoum University Hospitals following the agreement of the local institutional ethical committee and the local institutional review board (D 310). The prospective observational investigation enrolled hypotensive cases on mechanical ventilation from August 2022 until June 2024. A thorough, informed consent has been given prior to recruiting. The suggestions of the Consolidated Standards of Reporting Trials (CONSORT) for reporting randomized, controlled clinical studies have been adhered to. This trial is registered on clinicaltrial.gov (NCT05980494).
2.1. Inclusion Criteria
Cases over eighteen years of age on mechanical ventilation with circulatory failure, characterized by a Mean Arterial Pressure (MAP) below sixty-five millimeters of mercury or a systolic arterial pressure below ninety millimeters of mercury and exhibiting signs of hypoperfusion (such as skin mottling and serum lactate levels of two millimoles per liter or higher). [7].
2.2. Exclusion criteria
Intracardiac shunt, previously recognized severe valvular illness or cardiac arrhythmias. Chest drains, elevating intraabdominal pressure, peripheral vascular disorders, and ARDS cases result from reduced tidal volume. Interstitial lung illness is characterized by B-lines, which result from the thickened interlobular septa associated with fibrosis and remain unaffected by hydration status or fluid intake. Contraindications for the administration of fluid include acute pulmonary edema, left ventricular cardiogenic shock, ejection fraction below fifty percent, volume overload, and renal cases with oliguria, involving those cases that had an acute anuric renal failure or hemodialysis. Cases with thrombosis of arteries of the lower extremity or veins, significant arterial plaque in the lower extremities, blockage of lower extremity arteries, implantation of inferior vena cava restrictions, and lower extremity varicosities were also excluded.
All patients fulfilling the criteria were monitored by six leads. Electrocardiogram, measurement of blood pressure, lung ultrasound, pulse oximetry, inferior vena cava ultrasound, urinary catheter for urine output, and plethysmographic variability were performed on each subject in this investigation. The suggestions of the Consolidated Standards of Reporting Trials (CONSORT) have been adhered to. Lung ultrasound and IVC measurements have been conducted with a convex ultrasound probe (Philips Clear Vue 350, Philips Healthcare, Andover MAO1810, United States of America, Machine ID: 1385). The procedure has been conducted by an experienced radiologist in accordance with established guidelines. Each hemithorax will be divided into three primary regions (lateral, anterior, and posterior), delineated by the anterior axillary, posterior axillary lines, and para-sternal, resulting in a total of twenty-eight sectors. Each section will be partitioned into lower and upper halves, resulting in a total of six distinct quadrants for all sides: anterior inferior, anterior superior, lateral inferior, lateral superior, posterior inferior, and posterior superior [8, 9]. All quadrants received a score depending on B lines, defined as echogenic artifacts that have a small origin at the pleural line, continuing to the screen inferior edge, and being timed with movements of respiratory, revealing subpleural interstitial edema in the following manner: (0) Normal aeration is considered by the presence of A-lines with lung sliding or less than 2 isolated B lines. (1) Moderate loss of lung aeration is characterized by well-defined, multiple B lines. (2) Severe loss of lung aeration is characterized by several coalescent B lines. (3) Complete loss of lung aeration or lung consolidation is indicated by the absence of every single B line. This was utilized to compute the total lung ultrasound score (derived from the summation of all quadrant scores) and the scores for locations (anterior, lateral, and posterior) [10].
2.3. PPV
Cases were temporarily sedated, paralyzed, and placed on totally regulated MV. Ventilation modes were chosen based on either volume or pressure control, as determined by the primary physicians' decision. The tidal volume was no fewer than eight milliliters per kilogram of estimated body weight. The designated respiration rate was fourteen breaths per minute. The Positive End-Expiratory Pressure (PEEP) ranged from eight to ten cmH2O. The plateau pressure was maintained below thirty cmH2O. Radial artery cannulation has been performed in all cases for invasive blood pressure follow-up by a twenty-gauge cannula, and pulse pressure variation was directly measured on Nihon Kohden monitors at baseline. Then, patients underwent a Passive Leg Raising Test (PLRT) to evaluate the responsiveness of fluid. Independent of central venous pressure, a noninvasive ΔPLRSAP more than seventeen percent was shown to consistently identify fluid responders throughout “blind PLR.” In the context of “CVP-guided PLR,” a significant alteration in central venous pressure (minimum of two millimeters of mercury) indicates that noninvasive ΔPLRSAP is more effective, with a cutoff value equal to nine percent. The results observed in sedated cases who previously received volume expansion and/or catecholamines must be validated throughout the initial period of circulatory failure (prior to placement of arterial line) [11].
2.4. Primary Outcome
The specificity and sensitivity of each parameter in predicting the responsiveness of fluid.
Measured parameters and secondary outcomes: LUS B lines score, dIVC index, baseline characteristics involving patient age, weight, body mass index, PPV, CVP, HR, serum lactate, and UOP, and length of stay in the ICU.
Sample size: The sample size has been estimated utilizing MedCalc Statistical Software version twenty (MedCalc Software, Ostend, Belgium). The minimal sample number of cases was 118, with fifty-nine non-responsive cases and fifty-nine responsive cases. Estimation is guided by the area under the curve of 0.915 derived from research [12]. Compared with a null value of 0.8, with an alpha of 0.05 and a power of ninety percent, the sample size has been raised to 150 cases to improve precision and ensure that at least fifty-nine responding and fifty-nine non-responsive cases are involved.
2.5. Statistical Analysis
Data was gathered and encoded with Microsoft Excel, while analysis was conducted with IBM SPSS version twenty-eight for Windows. Descriptive statistics were exhibited as percentages and numbers for categorical information, while means with medians or SD with interquartile ranges have been utilized for numerical data variables. The receiver-operating characteristic curve has been utilized to determine the optimal cutoff point for the inferior vena cava distensibility index and the lung ultrasonography score. The AUC has been documented and utilized to evaluate the diagnostic efficacy of various tests. Specificity, sensitivity, negative predictive value, and positive predictive value were shown with the ninety-five percent confidence intervals. A P-value less than 0.05 has been deemed statistically significant.
3. RESULTS
Mean height, age, body mass index, and weight were 163.2 cm, 40.5 years, 30.5 kg/m2, and 80.7 kg, respectively (Table 1).
| Item | Mean | SD |
|---|---|---|
| Age (years) | 40.5 | 13.5 |
| Height (centimeter) | 163.2 | 8.6 |
| Weight (kilogram) | 80.7 | 18.4 |
| BMI (kilogram /meter square) | 30.5 | 7.4 |
The ultrasound score was zero in 67% (100 cases), one in 16% (24 cases), 2 in 10% (15 patients), and 3 in 7% (11 cases) (Table 2).
| Item | Number | Percentage |
|---|---|---|
| Passive leg-raising test Positive (Fluid responsiveness) Negative (Fluid non-responsiveness) |
82 68 |
55% 45% |
| Lung ultrasound score 0 1 2 3 |
\ \ 100 24 15 11 |
67% 16% 10% 7% |
There was a statistically significant variance among fluid non-responders and fluid responders with p-value < 0.05 regarding delta lung B lines, inferior vena diameter during both inspiration and expiration, pulse pressure, and inferior vena cava distensibility index variation, while there was a statistically insignificant variance regarding lung B lines, central venous pressure, heart rate, urine output, serum lactate, and ICU stay with p-values more than 0.05 (Table 3).
There was statistically insignificant variation regarding lung ultrasound scores among fluid responders and non-responders with p-values greater than 0.05 (Table 4).
The area under the Receiver-Operating Characteristic (ROC) curve and p-values of various hemodynamic and ultrasound variables were analyzed among patients. Variables with p-values lower than 0.05 (statistically significant) were evaluated to determine their sensitivities (true positive rates), specificities (true negative rates), and optimal cutoff values (Table 5).
| Fluid Responder Group (number =82) | Fluid Non-Responder Group (Number =68) | p-value‡ | |||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Lung B lines | 0.7 | 0.8 | 1.1 | 1.5 | 0.081 |
| Delta lung B lines | 1.8 | 1.5 | 0 | 0 | < 0.001 |
| IVC insp D (mm) | 1.6 | 0.1 | 1.5 | 0.2 | 0.004 |
| IVC exp D (mm) | 1.3 | 0.1 | 1.4 | 0.2 | 0.009 |
| Distensibility index IVC (%) | 20.9 | 3.7 | 8.9 | 5.7 | < 0.001 |
| Pulse pressure variation (%) | 16.7 | 3.1 | 11.5 | 2.5 | < 0.001 |
| Central venous pressure (mmH20) | 4.7 | 2.1 | 4.8 | 1.9 | 0.765 |
| Heart rate (beat/minute) | 85 | 17 | 87 | 16 | 0.412 |
| Urine output (ml/h) | 76.8 | 14.7 | 75.3 | 16.1 | 0.551 |
| Serum lactate (mmol/L) | 4.7 | 1.8 | 4.4 | 1.4 | 0.287 |
| ICU stay (days) | 20.4 | 22 | 23.6 | 24.4 | 0.395 |
| Fluid Responder Group (n=82) | Fluid Non-responder Group (n=68) | p-value# | |||
|---|---|---|---|---|---|
| Number | Percentage | Number | Percentage | ||
|
Lung ultrasound score
0 1 2 3 |
54
10 11 7 |
66%
12% 13.5% 8.5% |
46
14 4 4 |
67.5%
20.5% 6% 6% |
0.249 |
| Item | Cut-off | Sensitivity | Specificity | AUC | P-value |
|---|---|---|---|---|---|
| Lung B lines | - | - | - | 0.452 | 0.316 |
| Delta lung B lines | > 0 | 77% | 100% | 0.884 | <0.001 |
| IVC insp D (mm) | > 1.63 | 72% | 63% | 0.651 | 0.001 |
| IVC exp D (mm) | - | - | - | 0.427 | 0.124 |
| Distensibility index IVC (%) | > 18.5 | 90% | 96% | 0.944 | <0.001 |
| Pulse pressure variation (%) | > 13 | 94% | 93% | 0.907 | <0.001 |
| Central venous pressure (mmH20) | - | - | - | 0.476 | 0.632 |
| Heart rate (beat/minute) | - | - | - | 0.458 | 0.381 |
| Urine output (ml/h) | - | - | - | 0.516 | 0.737 |
| Serum lactate (mmol/L) | - | - | - | 0.524 | 0.612 |
| ICU stay (days) | - | - | - | 0.456 | 0.351 |
The reference (diagonal straight) (the 45° degree) line signifies no predictive ability with an Area Under the Curve (AUC) of 0.5, and the closer the curve of the variable is to the upper left corner of the diagram (the y-axis) (above the reference line), the better the predictive ability of the model, whereas receiver operating characteristic curves in the other area with the bottom right corner (below the reference line) indicate poor performance levels. This graph shows that the inferior vena cava inspiratory diameter is away from the reference line and closer to the upper left corner of the diagram (the y-axis), which demonstrates a good predictive ability (Fig. 1).
4. DISCUSSION
Our study demonstrated that there was no statistically significant difference between the two groups in terms of patient characteristics.
A similar study was conducted in 2015 on obese patients for fluid responsiveness on 63 patients with a mean age (42) y and BMI mean (36.1) [13]. Another study was conducted to assess variation of stroke volume as an indicator of responsiveness of fluid and reported that the mean age was (39±11) and BMI was (60±2).
A Mayr et al. study reported that lung ultrasound was performed in 50 critically ill patients on 28 B-line sectors with a mean (17) B line, while our study reported that the B-line mean number was 0.7 in fluid responders and 1.1 in non-responders with insignificant distinction among the 2 groups [14].
Moreover, in our study we measured pulse pressure variation between the responders and non-responders with 16.7 and 11.5, respectively, with a statistically significant variation among the 2 groups.
More studies were performed to assess pulse pressure variation and fluid responsiveness. PPV was 13.6 in fluid responders and 5.3 in fluid non-responders in the study by De Backer et al. [15], but in the study by Kramer et al., the PPV was 16.3 ±4.0 in responders and 7.1±2.7 in non-responders [16].
Regarding hemodynamics, there was a statistically insignificant distinction among the 2 groups for central venous pressure, heart rate, urine output, and serum lactate with a p-value > 0.05.
In contrast to our investigation, significant elevations have been observed in mean central venous pressure (9.9 ± 4.5 to 11.1 ± 4.8 millimeters mercury, P less than .0001) after fluid boluses. Nevertheless, there were insignificant variations in UOP, and there were clinically minor variations in heart rate and mean arterial pressure that align with our findings [17].
Our outcomes proved that there was insignificant variance in the length of stay in ICU among responders and non-responders. This contrasts with a meta-analysis published in 2017, which indicated that dynamic evaluation of fluid responsiveness had been related to a decreased period of the intensive care unit length of stay (weighted mean distinction, -1.16 days [ninety-five percent confidence interval, -1.97 to -0.36]; I2 = 74%; n = 394, six trials) [18].
Our study aligns with these findings, demonstrating a delta B-line sensitivity of 77% and specificity of 100%. Moretti et al. [19] reported that a dIVC value greater than 16% offered the optimal balance of test characteristics, with a sensitivity of 70.59% and a specificity of 100%. In comparison, our study identified a dIVC cutoff value of greater than 18.5, which achieved a sensitivity of 90% and a specificity of 96%.
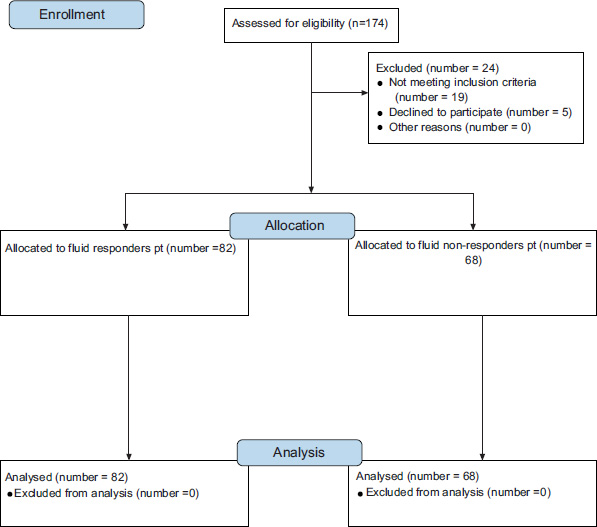
CONSORT flow diagram.
The optimal cut-off for positive predictive value determined by ROC curve analysis was 11.8 percent, with sensitivity at sixty percent, specificity at seventy-four percent, positive predictive value at seventy-four percent, and negative predictive value at sixty-one percent in the investigation by Yang et al. [20]. Conversely, the investigation by Kramer et al. [16] identified the ideal positive predictive value threshold for differentiating responders from non-responders as 11. A positive predictive value of > 11% forecasted an elevation in CO with 100% sensitivity and 93% specificity.
In our investigation, the optimal cutoff value for PPV was more than thirteen, demonstrating a sensitivity of ninety-four percent and a specificity of ninety-three percent for fluid responsiveness.
5. LIMITATIONS OF THE CURRENT STUDY
We did not measure the cardiac output, which is the best method to differentiate between fluid responders from non-responders. The length of stay in ICU could be affected by other associated pathologies. PPV was used in patients during mechanical ventilation who presented with no cardiac arrhythmia and no right ventricular failure. Therefore, the well-known limitations of PPV have not been challenged. We did not adjust volume expansion to patients’ weight or body surface area to be in line with methods of previously published studies.
CONCLUSION
Pulse pressure variation, lung ultrasound, and inferior vena cava distensibility index possess prognostic value for fluid response, demonstrating good specificity and sensitivity.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| ROC | = Receiver-Operating Characteristic |
| LUS | = Lung Ultrasound Scans |
| MAP | = Mean Arterial Pressure |
| AUC | = Area Under the Curve |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Fayoum University Hospitals, Egypt with permission from the local institutional ethical committee and the local institutional review board (D310).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
Declared None.


