All published articles of this journal are available on ScienceDirect.
Incidence and Associated Factors of Anesthesia-Related Complications in Ophthalmic Surgeries: A 6-Year Retrospective Cohort Study
Abstract
Introduction
The incidence of anesthesia-related complications in ophthalmic surgeries remains inadequately studied, especially in large-scale cohorts. Current research primarily emphasizes particular ophthalmic procedures, resulting in a lack of comprehensive understanding of the incidence and contributing factors of these complications within a varied patient demographic at university-affiliated, tertiary care hospitals.
Methods
This study employed a retrospective cohort design, analyzing electronic medical records from 2017 to 2022 at the Maharaj Nakorn Chiang Mai Hospital, Thailand. The Institutional Review Board approved the study. Data on anesthesia-related complications, including respiratory, cardiovascular, and cerebrovascular incidents, were collected. Statistical analyses evaluated the incidence rates and identified significant risk factors by comparing patients with and without complications.
Results
In a cohort of 3,982 patients, the incidence of complications related to anesthesia was determined to be 16.47%. Key predictors identified were extreme age categories, elevated ASA classifications, multiple attempts at intubation, and anesthetic durations exceeding 90 minutes. The establishment of a Pre-Anesthetic Clinic enhanced patient outcomes through comprehensive preoperative evaluations and risk assessments.
Conclusion
This study underscores the essential requirement for continuous evaluation of anesthesia-associated risks in ophthalmic surgical procedures. Structured preoperative evaluations can improve patient safety and reduce complications. The results indicate the need for modifications to institutional policies aimed at enhancing anesthesia care and facilitating positive postoperative outcomes.
1. INTRODUCTION
Ophthalmic surgery is considered a low-risk procedure because it is associated with minimal blood loss, a restricted surgical field, and limited effects on the circulatory and respiratory systems [1, 2]. Even so, ophthalmic surgery entails specific anesthetic considerations and patient risks, especially given that the patient demographic frequently includes extreme age groups, such as young children and the elderly [3]. The perception of eye surgery as low-risk may lead anesthesiologists to adopt a less cautious approach in patient care, potentially increasing the risk of severe complications. The surgical field imposes constraints on anesthesiologists, preventing them from promptly managing the airway during surgery. Furthermore, there is the challenge of appropriately adjusting anesthetic agents for delicate muscle surgeries that require stability throughout the procedure. Post-surgery, it is essential to facilitate a smooth awakening for the patient, avoiding coughing or vomiting, as these actions may negatively affect the stitches in the intraocular compartment and potentially alter intraocular pressure (IOP).
Despite its clinical significance, the incidence and associated factors of anesthesia-related complications in ophthalmic surgeries remain inadequately studied, particularly in large-scale cohorts. Current research is confined to small, single-center studies and narrowly focused investigations on particular ophthalmic procedures or specific age groups, such as the elderly or pediatric patients, thereby hindering a comprehensive understanding of anesthesia-related risks across diverse patient populations [1-3]. There exists a knowledge gap concerning outcomes in university-affiliated tertiary care hospitals that manage a wider range of complex cases.
This study aims to bridge this gap by analyzing the incidence and factors associated with anesthesia-related complications in ophthalmic surgeries over a six-year period at the university-based, tertiary care Maharaj Nakorn Chiang Mai Hospital, Thailand. By leveraging a retrospective cohort design, we provide a robust assessment of the patterns and predictors of complications in a real-world clinical environment. We aim for the results to contribute to optimizing anesthesia care in ophthalmic surgeries, adjusting institutional policies, guiding preoperative risk assessment, and ultimately improving patient safety. This study aims to report the incidence of anesthesia-related complications, identify the factors associated with these complications, and highlight the importance of the pre-anesthetic clinic (PAC).
2. MATERIALS AND METHODS
2.1. Study Design
This study was a retrospective cohort design, utilizing electronic medical records (EMR) from 2017 to 2022, retrieved from Maharaj Nakorn Chiang Mai Hospital, a university-based tertiary facility located in Northern Thailand. The Institutional Review Board (IRB) at the Faculty of Medicine, Chiang Mai University, granted approval for the study, designated by code number ANE-2566-09502, via an expedited review process. The study was conducted in accordance with the Helsinki Declaration (2013) by deidentifying patients, maintaining data confidentiality, and, due to the retrospective nature of the study, ensuring no harm to the patients.
2.2. Patients
Eligible participants included patients of all ages scheduled for ophthalmic surgeries requiring anesthesia services. Local anesthesia administered by the ophthalmologist was excluded. The keywords utilized in the electronic medical database for information retrieval included 2017–2022, cataract surgery, glaucoma surgery, corneal transplant, keratoplasty, strabismus correction, vitrectomy, intraocular lens aspiration, blepharoplasty, pterygium surgery, dacryocystorhinostomy (DCR), laser photocoagulation or scleral buckling for retinal detachment repair, enucleation or evisceration, and requests for anesthesia services.
2.3. Variables
This study investigates perioperative complications as primary outcomes, focusing on respiratory, cardiovascular, and cerebrovascular issues, as well as postoperative nausea and vomiting (PONV), medication errors, and unplanned admissions to the intensive care unit (ICU) in patients undergoing ophthalmic surgeries. The complications were diagnosed systematically according to established clinical criteria [4-7]. The main focus of this study is the administration of anesthesia throughout the perioperative period, encompassing the preoperative, intraoperative, and postoperative phases of surgery. Perioperative anesthesia-related adverse events refer to any negative outcomes or incidents directly linked to the administration of anesthesia, varying in severity from transient, mild conditions to severe, life-threatening occurrences [8]. Predictor variables include different types of ophthalmic surgeries, surgery duration, operator expertise, staff availability (ophthalmologist and anesthesiologist), and patient-specific factors such as age, comorbidities, pre-existing respiratory or cardiovascular conditions, and obesity, all of which may influence the likelihood and severity of adverse events. The analysis considers specific effect modifiers, including patient subpopulations such as pediatric and elderly patients, individuals with pre-existing respiratory conditions, and obese patients. Respiratory complications, defined as perioperative respiratory adverse events (PRAE), were identified through the occurrence of events including laryngospasm, bronchospasm, hypoxemia, and desaturation [4, 5]. Cardiovascular complications, encompassing outcomes from arrhythmias to cardiac arrest, were identified through standard diagnostic protocols [6]. Major cerebrovascular complications, such as stroke and intraoperative awareness, were incorporated as outcomes, with diagnostic criteria specifically adapted to the perioperative context [7].
2.4. Bias Recognition
To address the biases inherent in a retrospective cohort study, several measures were implemented. Clear inclusion and exclusion criteria were applied during participant selection to minimize selection bias, while the diagnosis of complications was standardized using ICD-10 codes documented in the discharge summaries from electronic medical records (EMR), reducing both information bias and outcome assessment bias. To mitigate confounding bias, potential confounders were identified, stratified accordingly, and multivariate statistical methods were applied for adjustment. The study cohort was clearly defined by specifying a fixed time period ending at the admission date for scheduled ophthalmic surgery, thereby minimizing the effects of temporal ambiguity and survivorship biases. Missing data were acknowledged, and their potential impact on the results was thoroughly analyzed and discussed in the limitations section. Lastly, the risk of reverse causality bias was minimized, as patients were systematically assessed for risk factors prior to surgery through the pre-anesthetic clinic (PAC).
2.5. Sample Size
The total study population was identified as 4,056 patients using keyword inputs within the electronic medical record (EMR) database from 2017 to 2022. Following the exclusion of 74 patients, the final cohort included 3,982 patients. The power of the study was calculated retrospectively based on the original sample size of 4,056 patients. From previous studies [1-3], the expected incidence rate of complications was estimated to be 10%. The null hypothesis assumed a true incidence rate of 10%, with no pre-specified directionality, utilizing a significance level (α = 0.05) and a two-tailed test. With the initial sample size of 4,056 patients, the statistical power of the study was determined to be greater than 90% to detect an incidence rate of 10%. This was achieved with a small standard error due to the large sample size. The margin of error was calculated to be approximately 0.92%, indicating the study's robustness in reliably detecting perioperative complications.
2.6. Statistical Methods
This is an observational study. We employed statistical methods to compare patients who experienced anesthesia-related complications with those who did not. Continuous variables were analyzed using the Student’s t-test for normally distributed data and the Mann-Whitney U test (rank-sum test) for data that did not meet the assumption of normality. Categorical variables were assessed using the Chi-square test or Fisher’s exact test when expected cell counts were less than five, to examine differences between the two groups. To identify significant risk factors associated with anesthesia-related complications, a two-step process was performed. First, univariate analysis was conducted for each variable to preliminarily identify associations. Variables with a p-value <0.20 in the univariate analysis were entered into a multivariable logistic regression model to control for confounding and identify independent predictors of complications. Adjusted odds ratios (aORs) with 95% confidence intervals (CIs) were calculated to quantify the strength of association between risk factors and complications. Statistical significance was set at a p-value <0.05. To investigate subgroup effects and potential interactions, stratified analyses were conducted based on key covariates: age groups and surgical factors. Interaction terms were considered in the regression models to assess whether associations differed across subgroups. Methods were implemented to address missing data. For variables with missing values, multiple imputation techniques were performed to minimize bias. Sensitivity analyses were conducted to evaluate the impact of missing data and confirm the robustness of findings, including a complete-case analysis. Differences between imputed and complete-case results were examined to ensure consistency. As this was a retrospective study, there was no loss to follow-up. However, patients with incomplete records or an inability to meet eligibility criteria were excluded from the analysis, and this was documented in detail. All statistical analyses were performed using SPSS version 26 (IBM Corp., Armonk, NY, USA), guaranteeing a robust evaluation of differences and associated risk factors.
3. RESULTS
Between 2017 and 2022, a total of 4,056 patients were scheduled to receive anesthesia services for ophthalmic surgeries. Seventy-four patients were excluded because of incomplete data. The remaining 3,982 patients were analyzed. Figure. (1) demonstrates the Consolidated Standards of Reporting Trials (CONSORT) diagram.
The surgeries included phacoemulsification, lens aspiration, 23-gauge pars plana vitrectomy, intraocular muscle correction, and glaucoma drainage implant (GDI). The demographics and baseline characteristics are presented in Table 1. A total of 3,982 patients underwent ophthalmic surgeries, of whom 57.9% were male and 42.1% female. The majority of patients (70.6%) were aged between 5 and 65 years, with 22.4% aged above 65 years. Most patients (71.5%) had no history of prior ocular surgeries. The sample included 91.7% of surgeries lasting more than one hour, and endotracheal intubation was the predominant airway management technique utilized (87.5%), while the remainder used laryngeal masks. Complications occurred at least once in 594 events involving 656 out of 3,982 patients. Among 56 patient events, two complications were noted; three complications arose in five patient events, and one patient experienced four complications. The incidence rate of anesthesia-related complications was 16.47%. The events can be classified as follows: cardiovascular events (6.28%), respiratory events (5.5%), cerebrovascular events (0%), postoperative nausea and vomiting (PONV) (2.29%), unplanned ICU admissions (0.36%), and shivering (0.35%). As shown in Fig. (2), the most prevalent anesthesia-related complications were difficult intubation (25%), arrhythmias (19%), hypertension (17%), nausea/vomiting (16%), sore throat (12%), hypotension (9%), and shivering (2%). The percentages represent the distribution of these complications among the total number of patients with complications. Rare complications such as desaturation and myocardial infarction were observed in very few cases and, for clarity, are not presented in the figure.
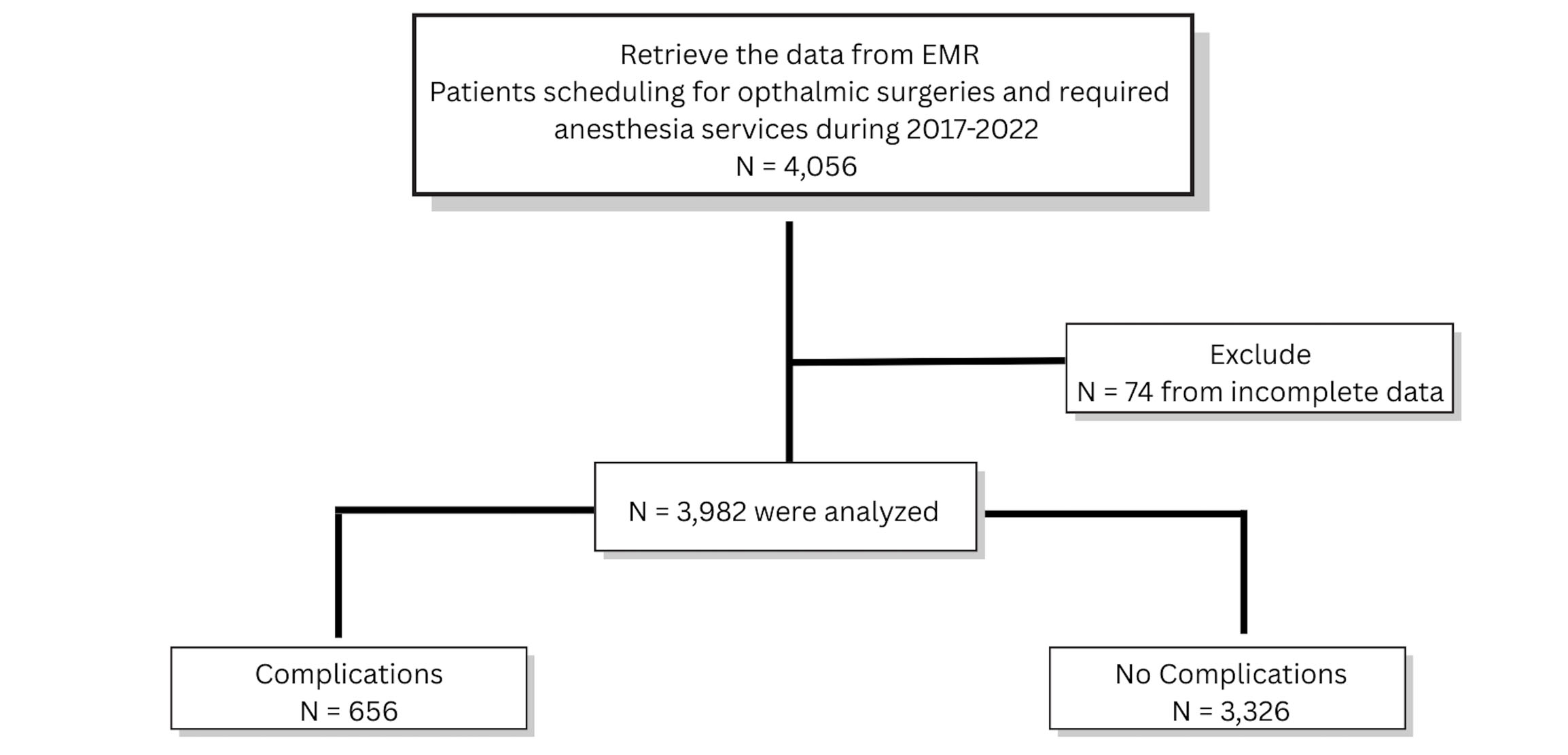
Consolidated Standards of Reporting Trials (CONSORT) diagram. EMR: electronic medical record.
| Variables | n (%) | |
|---|---|---|
| Gender M/F | 2,307 (57.9%)/1,675 (42.1%) | |
| Age group | - | |
| • < 5 yr. | 278 (7.0%) | |
| • 5-65 yr. | 2,810 (70.6%) | |
| • > 65 yr. | 894 (22.4%) | |
| Previous ocular surgery | - | |
| • No | 2,848 (71.5%) | |
| • Yes | 1,134 (28.5%) | |
| • Retain intra-ocular gas | 43 (3.8%) | |
| • Not retain intra-ocular gas | 1,091 (96.2%) | |
| Systemic co-morbidities | - | |
| • No | 2,919 (73.3%) | |
| • Yes | 1,063 (26.7%) | |
| Types of ophthalmic surgery | - | |
| • Phacoemulsification | 1,875 (47%) | |
| • Lens aspiration | 134 (3.4%) | |
| • 23 Gauge pars plana vitrectomy | 1,548 (38.9%) | |
| • Intraocular muscle correction | 173 (3.4%) | |
| • Glaucoma drainage implant | 252 (6.3%) | |
| Duration of surgery | - | |
| • < 30 minutes | 54 (1.36%) | |
| • 30 minutes – 1 hour | 278 (7.0%) | |
| • > 1 hour | 3,650 (91.7%) | |
| Technique of airway management | - | |
| • Laryngeal mask airway | 497 (12.5%) | |
| • Endotracheal intubation | 3,485 (87.5%) | |

Distribution of the most common anesthetic-related complications observed in ophthalmic surgeries. Percentages indicate the proportion of each complication among the total cases with common complications. Less frequent complications (such as desaturation and myocardial infarction) are not depicted in this figure.
Table 2 demonstrates the incidence of anesthesia-related complications, management, and prognosis. Respiratory complications occurred in 219 cases (5.5%). The most common respiratory issue was difficult intubation (137 cases). Less common complications included sore throat (66 cases). Severe complications, such as pulmonary aspiration (1 case) or re-intubation (2 cases), were infrequent. Regarding prognosis, most patients showed improvement. Difficult intubation was successfully managed in 135 cases, indicating that intubation was achieved on the second or third attempts by anesthesiology staff utilizing additional airway equipment. Successful intubation using a video laryngoscope was achieved in 78% of cases. The remaining patients were successfully intubated by anesthesiology staff utilizing a conventional laryngoscope blade and repositioning to enhance the laryngeal view. However, 2 patients required consultation with more than one anesthesiology staff member, and 1 patient required re-intubation and subsequent ICU admission. Other mild complications, such as sore throat and desaturation, resolved without extensive management.
| Complications | Number (%) | Location | Prognosis | ||||
|---|---|---|---|---|---|---|---|
| Intraoperative | Recovery room | Within 24 h after surgery | Improve | Consultation | ICU admission | ||
| Respiratory (total number, %) (219, 5.5%) | |||||||
| Difficult intubation | 137 | 137 | 0 | 0 | 135 | 2 | 1* |
| Pulmonary aspiration | 1 | 1 | 0 | 0 | 0 | 1 | 0 |
| Esophageal intubation | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Re-intubation | 2 | 0 | 2 | 0 | 1 | 0 | 1* |
| Desaturation | 5 | 5 | 0 | 0 | 5 | 0 | 0 |
| Bronchospasm | 3 | 3 | 0 | 0 | 3 | 0 | 0 |
| Sore throat | 66 | 0 | 60 | 6 | 66 | 0 | 0 |
| Dental injury | 5 | 5 | 0 | 0 | 5 | 0 | 0 |
| Cardiovascular system (total number, %) (250, 6.28%) | |||||||
| Arrhythmias | 107 | 107 | 0 | 0 | 105 | 2 | 0 |
| Hypotension | 50 | 50 | 0 | 0 | 50 | 0 | 0 |
| Hypertension | 92 | 90 | 2 | 0 | 92 | 0 | 0 |
| Myocardial infarction | 1 | 0 | 1 | 0 | 0 | 1 | 1 |
| Cardiac arrest | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cerebrovascular system (total n) 0 | |||||||
| Stroke | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Nerve injury | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Awareness | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Others (total number, %) (105, 2.6%) | |||||||
| Nausea/ vomiting | 91 | 0 | 80 | 11 | 91 | 0 | 0 |
| Hypoglycemia | 1 | 1 | 0 | 0 | 1 | 0 | 0 |
| Hyperglycemia | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Shivering | 14 | 0 | 14 | 0 | 14 | 0 | 0 |
| Anaphylaxis | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Drug errors | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Cardiovascular complications were more frequent, with 250 cases (6.28%). Arrhythmias were the most common cardiovascular issue (107 cases). All arrhythmias observed were bradycardia occurring during the early phase of ophthalmic surgery. Forty percent required intravenous atropine, while the remainder resolved spontaneously and/or after notifying the surgeons. Hypotension (50 cases) and hypertension (92 cases) were significant but managed mainly during surgery. There was 1 case of myocardial infarction in the recovery room, and no cardiac arrests were reported. Regarding prognosis, most cardiovascular complications resolved with intraoperative management, except for the myocardial infarction case, which required cardiologist consultation and admission to the cardiac ICU.
Digestive system complications, primarily nausea/vomiting (91 cases), were common, occurring mostly in the recovery room (80 cases) or within the first 24 hours postoperatively (11 cases). Regarding metabolic issues, there was 1 case of hypoglycemia occurring intraoperatively, which resolved postoperatively. Thermoregulatory issues, specifically shivering (14 cases), were noted exclusively postoperatively in the recovery room.
Multiple risk factors were significantly linked to heightened postoperative complications, including age group, smoking, hypertension, dyslipidemia, renal impairment, prior cerebrovascular disease, and the frequency of intubation attempts (p < 0.05), as demonstrated in Table 3. Increased surgical duration in minutes correlated with a rise in complications. The odds ratio suggests that for every additional hour, complications increase by a factor of 1.53. Multivariate analysis indicated that patients in extreme age groups, with high ASA classifications, multiple intubation attempts, and anesthetic durations exceeding 90 minutes, are significant predictors of postoperative complications in elective ophthalmic surgery (Table 4).
| Variables | Complications n (%) |
No complications n (%) |
p-value | |
|---|---|---|---|---|
| Gender M/F | 324 (14)/ 158 (9.4) | 1,983 (86)/ 1,517 (90.6) | 0.56 | |
| Age group | - | - | - | |
| • < 5 yr. | 19 (6.83) | 259 (93.17) | 0.00* | |
| • 5-65 yr. | 425 (15.12) | 2,385 (84.88) | ||
| • > 65 yr. | 212 (23.71) | 682 (76.29) | ||
| Previous ocular surgery | - | - | - | |
| • No | 93 (3.26) | 2,391 (96.74) | 0.20 | |
| • Yes | 76 (6.7) | 1,058 (93.3) | ||
| • Retain intra-ocular gas | 6 (13.9) | 37 (86.1) | 0.57 | |
| • Not retain intra-ocular gas | 82 (7.5) | 1,009 (92.5) | ||
| Systemic co-morbidities | - | - | - | |
| • No | 253 (8.6) | 2,666 (91.4) | 0.03* | |
| • Yes | 756 (71.1) | 307 (28.9) | ||
| Duration of surgery | - | - | - | |
| • < 30 minutes | 8 (14.8) | 46 (85.1) | 0.02* | |
| • 30 minutes – 1 hour | 93 (33.4) | 185 (66.5) | ||
| • > 1 hour | 555 (15.2) | 3,101 (84.7) | ||
| Technique of airway management | - | - | - | |
| • Laryngeal mask airway | 43 (8.65) | 454 (91.35) | 0.34 | |
| • Endotracheal intubation | 386 (11) | 3,099 (89) | ||
| ASA physical status ≥ 3 | 106 | 3,326 | 0.00* | |
| Intubation attempt > 1 | 7 | 378 | 0.02* | |
| Poor control of hypertension | 238 | 815 | 0.00* | |
| Diabetes with insulin infusion | 118 | 399 | 0.00* | |
| Dyslipidemia | 92 | 321 | 0.00* | |
| Anemia | 56 | 226 | 0.11 | |
| Smoking | 57 | 230 | 0.02* | |
| Chronic kidney disease stage ≥ 3 | 58 | 164 | 0.00* | |
| Previous ischemic stroke | 16 | 46 | 0.05* | |
| Clinical risk factors | OR (95% CI) | p-value |
|---|---|---|
| Male | 1.05 (0.80-1.39) | 0.513 |
| ASA physical status ≥ 3 | 1.26 (1.05-1.50) | 0.010* |
| Age < 5 yr. | 1.96 (1.20-3.18) | 0.007* |
| Age > 65 yr. | 2.78 (1.67-4.63) | 0.000* |
| Operation time ≥ 2 hours | 1.53 (1.37-1.70) | 0.000* |
| Smoking | 1.31 (0.95-1.81) | 0.089 |
| Intubation attempt > 1 | 3.56 (1.23-10.26) | 0.019* |
| Poor control of hypertension | 1.16 (0.92-1.46) | 0.198 |
| Diabetes with insulin infusion | 1.05 (0.8-1.37) | 0.724 |
| Chronic kidney disease stage ≥ 3 | 1.17 (0.82-1.65) | 0.373 |
| Previous ischemic stroke | 1.18 (0.65-2.14) | 0.582 |
Analysis of Missing Data and Sensitivity: Multiple imputation techniques were employed to address missing data in the variables, thereby minimizing potential bias in the analysis. Sensitivity analyses, encompassing a complete-case analysis, were performed to evaluate the robustness of the findings. The sensitivity analyses revealed no significant differences between the analyses of imputed data and complete-case analyses, thereby confirming the consistency of the outcomes.
Patients Excluded: Seventy-four patients with incomplete data regarding perioperative complications were excluded from the primary analysis. An analysis of the discharge summaries indicated that all excluded patients were discharged to their homes, on average, 4 ± 2 days post-surgery. No mortalities were recorded among these patients. The findings indicate that the excluded patients exhibited postoperative outcomes similar to those of the overall study population.
4. DISCUSSION
The search for “anesthetic complications in ophthalmic surgery” revealed findings focused on ocular complications associated with perioperative anesthesia. However, anesthetic complications occurring in perioperative ophthalmic surgery are rarely documented in the literature. The under-researched and underreported nature of the topic arises from various factors discussed in the introduction, including the perception of minimal surgical risk. The research indicated that among 3,982 patients scheduled for ophthalmic surgery under anesthesia, the incidence rate of complications was 16.47%. This figure does not align with the perceived minimal surgical risk associated with ophthalmic procedures. This study aims to investigate the underlying causes of the unexpectedly high incidence of anesthesia-related complications in ophthalmic surgery.
Comparative analysis of our study results with prior research indicates that the incidence of complications during eye surgery ranges from less than 1% to 21%, influenced by factors such as the type of surgery and the duration of patient follow-up [1-3]. Prior research has identified complications associated with specific categories of eye surgeries, including cataract surgery, vitreoretinal surgery, ocular oncologic surgery, and primary rhegmatogenous retinal detachment, among others [1-3, 9]. Conversely, our study includes all categories of eye surgeries necessitating general anesthesia. This aspect is regarded as a strength of the study, as it offers a comprehensive overview of ophthalmic surgery. Despite being classified as a low-risk procedure, it is essential to prioritize patient safety and consider potential anesthesia-related complications. The study results indicated that severe complications, including myocardial infarction and unplanned ICU admission, were observed in elderly and neonatal patients, whereas all cases of bronchospasm (3 cases) were noted in patients under 5 years of age.
Cardiovascular events were the most frequently observed complication, reported in 6.28% of cases in this study, consistent with findings reported by Cheng et al. [1]. The most prevalent cardiovascular event observed was arrhythmias, specifically bradycardia. All instances of bradycardia in our study occurred during ophthalmic surgery, specifically in the early anesthetic maintenance period. The activation of the oculo-cardiac reflex (OCR) is presumed to be the cause [10]. The sensory nerves of the eye were activated, likely due to traction on the extraocular muscles, pressure on the globe, or manipulation of the orbital structures, transmitting the input through the afferent limb of the ophthalmic division of the trigeminal nerve (cranial nerve V). The efferent limb, involving the vagus nerve (cranial nerve X), is activated, resulting in a decrease in heart rate [10]. All bradycardia events were fully resolved either by notifying the surgeon to cease stimulation, administering atropine, or a combination of both, without any severe consequences.
The primary respiratory complication observed in our study was difficult intubation. Multivariate analysis indicated that multiple intubation attempts significantly predicted postoperative complications in elective ophthalmic surgery. This issue is categorized as high frequency, yet it is manageable and preventable. This finding highlights the importance of comprehensive preoperative assessment and suggests the need for strategic planning in situations involving challenging airways. The availability and responsiveness of anesthesiology staff to intervene when residents are unable to successfully intubate is crucial [11-15].
Our findings underscore several factors influencing anesthesia-related complications, as follows.
Demographic Categories: The study found that extreme age groups, specifically pediatric and elderly patients, correlate with increased complication rates. This indicates that these populations may necessitate more thorough preoperative assessments and customized anesthesia management [2, 3, 16]. Our findings align with prior studies indicating that extreme age groups, particularly pediatric and elderly patients, are at increased risk for adverse outcomes [3].
Elevated American Society of Anesthesiologists (ASA) classifications signify an increased risk of complications. Patients with substantial comorbidities exhibit a higher likelihood of adverse outcomes, highlighting the necessity for comprehensive risk assessments.
The study identified that multiple intubation attempts were a significant predictor of complications. This underscores the necessity of preparing for difficult airways and ensuring the availability of skilled personnel to promptly manage these scenarios.
Extended surgical durations, especially those surpassing 90 minutes, were associated with higher rates of complications. This indicates that prolonged surgeries necessitate vigilant monitoring and potentially more rigorous anesthetic management [4].
The establishment of a Pre-Anesthetic Clinic improved patient outcomes through comprehensive preoperative assessments. This underscores the importance of systematic assessments and the identification of anticipated difficult airway cases to mitigate the risks associated with anesthesia.
Patient-specific factors, including co-morbidities such as hypertension and diabetes, contribute to an increased likelihood of complications, underscoring the necessity of considering individual health profiles in anesthesia planning [16].
The factors collectively highlight the complexity of anesthesia management in ophthalmic surgeries and underscore the need for ongoing evaluation and optimization of anesthesia practices to improve patient safety and outcomes.
However, these results may differ from those of Alboim et al. [9], who reported that outpatient preoperative evaluations did not significantly reduce adverse events in cataract surgery candidates. Similarly, a Cochrane review concluded that routine preoperative medical testing for cataract surgery does not improve procedure safety [11, 12]. Despite these contrasts, the PAC at our institution functions as a dedicated consultation center for patients with complex or controversial conditions, aiming to provide tailored assessments for better surgical outcomes.
Minor complications that directly impact recovery quality following ophthalmic surgery under general anesthesia include nausea, vomiting, and shivering. This study identified a significant incidence of postoperative nausea and vomiting (PONV), with 91 cases reported, despite minimal use of nitrous oxide and limited administration of systemic opioids [13]. We hypothesized that the etiology of PONV may originate from OCR [10, 14]. Another explanation for PONV involves changes in intraocular pressure (IOP) that synergize with residual anesthetic agents [14, 15]. A forced-air warming device was regularly employed during surgical procedures and continued in use within the post-anesthetic care unit (PACU) for specific cases of shivering.
The study indicates that complications arising during anesthesia for eye surgery correlate with extended surgery durations. An in-depth analysis indicated that extended surgery durations are attributable to our institution's status as a medical school with residency training programs. Ophthalmology residents initially perform surgeries rather than staff, resulting in prolonged surgery durations. This influences the anesthesiologist's decision-making concerning the adjustment of anesthesia and muscle relaxants, as well as the duration of the surgery. In certain instances, staff ophthalmologists must be summoned due to the inability of resident ophthalmologists to successfully perform the surgery. This study's findings offer empirical evidence emphasizing the necessity of consulting staff ophthalmologists to minimize surgery times, thereby reducing complications, and highlight the critical role of communication within the team.
This study presents significant limitations that require acknowledgment. The reliability of a retrospective analysis is contingent upon the completeness and accuracy of electronic medical records (EMR). Despite efforts to reduce bias in information and outcome assessment, the risk of incomplete records remains. Seventy-four patients were excluded because of incomplete data, which may introduce selection bias. An analysis of the excluded patients revealed that their postoperative outcomes were similar to those of the included population, thus minimizing the overall effect of this exclusion. The statistical power of the study exceeds 90%; however, the retrospective design limits the ability to establish causality between risk factors and complications. Furthermore, while multiple imputation techniques were employed to address missing data, residual biases may continue to influence the results. The research focused solely on patients undergoing specific ophthalmic surgeries; therefore, the results may not be applicable to other surgical fields or patient populations.
This study's findings are mainly relevant to patients undergoing ophthalmic surgeries during the specified period at the data collection institution, potentially limiting generalizability. The study's large sample size of 3,982 patients enhances the reliability of the findings; however, the context of implementation, including the practices and demographics of a single institution, should be considered when generalizing results to wider populations. Variations in anesthetic practices, patient demographics, and healthcare systems across regions may significantly impact outcomes and the applicability of these findings. Future studies in varied settings are needed to validate the results and improve the generalizability of findings across diverse populations and surgical contexts.
4.1. New Knowledge of the Study
This study identifies predictors of anesthesia-related complications in ophthalmic surgeries, advancing knowledge in anesthesiology. Key findings are summarized as follows:
Effects of Repeated Intubation Attempts: Our research indicates that an increased number of intubation attempts significantly predicts anesthesia-related complications. This finding highlights the necessity of effective airway management strategies and training for anesthesiology personnel, as intubation challenges can elevate surgical risks. Comprehending this relationship can inform clinical practices to reduce complications linked to difficult airways.
The study indicates that surgical durations over 90 minutes are associated with increased complication rates. This finding suggests that extended surgeries require enhanced monitoring and potentially stricter anesthetic management to ensure patient safety. Understanding the influence of surgical duration on outcomes can improve surgical scheduling and resource allocation in clinical environments.
The Pre-Anesthetic Clinic is essential for enhancing patient outcomes. The establishment and use of PACs enable thorough preoperative assessments, improving risk stratification and personalized anesthesia management. This approach can significantly reduce complications, especially in high-risk groups.
4.2. Clinical Implications
The findings of this study can be implemented in clinical practice through the following recommendations:
1. Improve training protocols for airway management. Given that multiple intubation attempts are a significant predictor of complications, it is essential for training programs to emphasize advanced airway management techniques.
2. Enhance surgical scheduling through the assessment and adjustment of practices to minimize the duration of ophthalmic procedures. Engage experienced personnel earlier in the process to support residents, potentially decreasing total surgery duration and related risks.
3. Improve Pre-Anesthetic Clinics (PAC). Develop the PAC model to ensure thorough evaluations for patients with complex medical histories. Facilitating healthcare providers to improve patient safety and outcomes in ophthalmic surgeries, thus reducing anesthesia-related complications.
CONCLUSION
This study offers important insights into the incidence and predictors of anesthesia-related complications during ophthalmic surgeries in a university-based, tertiary care hospital. The analysis reveals an incidence rate of 16.47%, suggesting that the perceived risk of anesthesia in these procedures is frequently underestimated. Identified key predictors include extreme age groups, elevated ASA classifications, multiple intubation attempts, and extended anesthetic durations, highlighting the necessity for comprehensive preoperative evaluations. The establishment of a Pre-Anesthetic Clinic (PAC) has been crucial in enhancing patient safety through the meticulous screening of surgical candidates. Our findings emphasize the importance of acknowledging the complexities of perioperative anesthesia and improving communication among residents and staff ophthalmologists, advocating for a structured approach to reduce surgical delays and associated complications. This study underscores the necessity for ongoing research into anesthesia-related risks and advocates for the adoption of specific policies aimed at improving patient outcomes and safety in ophthalmic surgery.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: P.P. (Corresponding author) contributed to conceptualization, proposal development, ethical board acquisition, data analysis, manuscript writing of the original draft, and gave final approval of the version to be published. W.K. was responsible for the ethics submission process, data acquisition, data curation, data analysis, and also provided final approval of the version to be published. A.S. contributed to conceptualization, methodology, statistical review, manuscript validation, and gave final approval of the version to be published. All three authors agreed to take responsibility for all aspects of this research manuscript regarding its accuracy and integrity.
LIST OF ABBREVIATIONS
| ASA | = American Society of Anesthesiology |
| PAC | = Pre-Anesthetic Clinic |
| IOP | = IntraOcular Pressure |
| EMR | = Electronic Medical Record |
| OCR | = Oculo-Cardiac Reflex |
| PACU | = Post-Anesthetic Care Unit |
| PONV | = Postoperative Nausea and Vomiting |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The institutional review board of Maharaj Nakorn Chiang Mai Hospital, Faculty of Medicine, Chiang Mai University, Thailand approved the study (code ane-2566-09502).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available along with the article as (Excel file). This is a partial dataset, anonymized to the patient identification.
ACKNOWLEDGEMENTS
Declared none.


