All published articles of this journal are available on ScienceDirect.
Preemptive Alveolar Recruitment Maneuver Followed by PEEP in Obese Patients Undergoing Laparoscopic Gastric Banding. Does it make a Difference? A Randomized Controlled Clinical Study
Abstract
Background:
Impaired respiratory functions during general anesthesia are commonly caused by lung atelectasis more in morbidly obese patients. This occurs more frequently with laparoscopic surgery due to trendelenburg position and pneumoperitoneum. Preemptive recruitment maneuver + PEEP results in the prevention of these changes.
Aim:
To quantitate the effects of RM and PEEP on intraoperative hypoxemia and respiratory mechanics during laparoscopic gastric banding in obese patients.
Study Design:
A randomized, double-blinded, controlled study.
Method and Materials:
Fifty adults ASA I-II, BMI (40-50 kg/m2) for elective laparoscopic gastric banding were randomized into, groups C, and RM, 25 patients each. Group C patients received standard ventilation, VT 6 ml/kg, I: E ratio 1: 2 PEEP 5 cm H2O, and respiratory rate 10-12 breaths/ min. RM patients received standard ventilation with one alveolar recruitment maneuver after mechanical ventilation with PEEP of 15 cm H2O till the end of the surgery. Heart rate, mean blood pressure, respiratory mechanical parameters: peak airway pressure, plateau pressure and end-expiratory lung volume, PaO2, PaO2/FiO2 and (SpO2) were assessed.
Results:
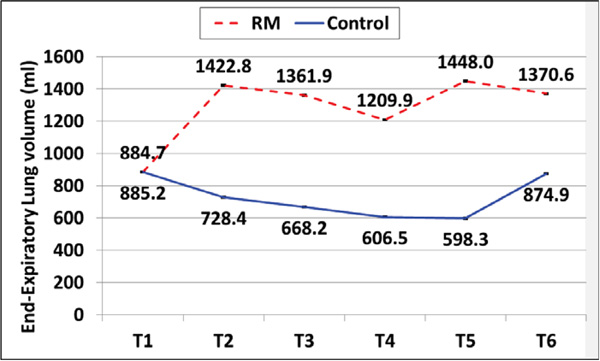
PaO2 and PaO2/FiO2 ratio increased significantly in the RM group after RM from T2 (before pneumoperitoneum) to T6 (end of surgery) compared with group C (P < 0.001). Peak and plateau airway pressures increased significantly in group C from T2 till T5 (60 min after pneumoperitoneum) compared with the RM group (P < 0.001). End-expiratory lung volume increased significantly in the RM group after RM compared with group C (P<0.001).
Conclusion:
Preemptive RM with PEEP of 15 cm H2O was effective in preventing pneumoperitoneum-induced intraoperative hypoxemia and respiratory mechanics changes.
1. INTRODUCTION
World Health Organization defined obesity as a Body Mass Index (BMI) above 30 kg/m2. The characteristic physiological changes induced by obesity such as decreased Functional Residual Capacity (FRC), increased demand for oxygen, decreased lung compliance, and altered ventilation-perfusion ratio make these patients prone to perioperative complications like atelectasis, hypoxia and hypercapnia [1].
Several clinical trials have tested different intra-operative ventilation strategies in these patients to re-inflate the collapsed lungs and optimize the oxygenation. These strategies include the application of Positive End Expiratory Pressure (PEEP) or Recruitment Maneuvers (RM) in the form of application of positive airway pressure to re-inflate the collapsed lung tissue [2].
End Expiratory Lung Volume (EELV) which is the functional residual capacity during mechanical ventilation has been found to be a sensitive indicator than oxygenation for PEEP- induced alveolar recruitment [3]. No well-known effective ventilation protocol has been established for obese patients undergoing the laparoscopic procedure with general anesthesia. This ventilation strategy would be expected to optimize respiratory mechanics, gas exchange, and minimize the risk of postoperative respiratory complications.
Therefore, the rational stands behind this study were to quantitate the effects of preemptive alveolar recruitment maneuver followed by PEEP on intraoperative gas exchange, respiratory mechanics and hemodynamics for laparoscopic gastric banding in obese patients under general anesthesia. We hypothesized that RM followed immediately with PEEP could attenuate the intra-operative pneumoperitoneum-induced detrimental effects on gas exchange and respiratory mechanics.
2. PATIENTS AND METHODS
2.1. Study Groups
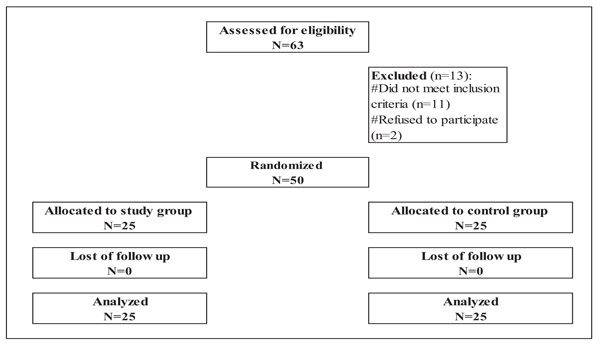
After obtaining the approval of our institutional ethics and research committee (FMASU R64/2018), written informed consent was taken from all patients. Fifty American Society of Anesthesiologist (ASA) physical status II-III patients scheduled for elective gastric banding were prospectively included in the current study, patients were enrolled into one of two randomized, double-blind, controlled study groups using a randomization schedule generated by computer and sealed opaque envelopes.
Patients were eligible for inclusion if they were; 20-50 years of age and had Body Mass Index (BMI) between 40 and 50 kg/m2. They were excluded if they had one of the following: previous lung surgery, chronic obstructive pulmonary disease, restrictive lung disease, bronchial asthma, home oxygen therapy, lung bullae, uncompensated cardiac disease (NYHA class III or IV), hemodynamic instability and increased intracranial pressure. In addition, any patient who developed hemodynamic instability (mean blood pressure < 60 mmHg) or desaturation (SpO2 < 90%) during the recruitment procedure was excluded from the study.
Patients were randomly divided into two groups, control group (group C, n = 25) and study RM group (group RM, n = 25) (Fig. 1). All patients were fasted at least 8 hrs before induction of anesthesia and were premeditated with granisetron 1 mg IV, ranitidine 50 mg IV and midazolam 2 mg IV before shifting to the operating theatre. Group C patients received the standard ventilation protocol immediately after intubation as the following; Volume Controlled Ventilation mode (VCV), with VT 6 ml/kg of Ideal Body Weight (IBW), inspiratory: Expiratory ratio 1: 2, Positive End Expiratory Pressure (PEEP) of 5 cm H2O, and respiratory rate 10-12 breaths/ min that was adjusted to keep End-Tidal Carbon Dioxide tension (ETCO2) between 35-45 mmHg. Patients in group RM received the standard ventilation protocol immediately after intubation with one alveolar recruitment maneuver, followed by PEEP of 15 cm H2O done as soon as the patient connected to mechanical ventilation till end of surgery and extubation. The recruitment was performed as soon as the patient was connected to mechanical ventilation and before positioning and initiation of pneumoperitoneum by application of continuous positive airway pressure 40 cm H2O for 45 seconds. This recruitment maneuver was followed immediately by PEEP of 15 cm H2O in the study group (group RM) that was kept constant throughout till the end of surgery and deflation of pneumoperitoneum. For safety, the peak inspiratory pressure of the ventilator was limited to 45 cm H2O. Engström Carestation ventilator (General electric, Helsinki, Finland) was used in this study. Many studies have been done to evaluate the accuracy, precision and reproducibility of measurements of EELV done by this ventilator [4-6].
2.2. Anesthetic Technique
On arrival of the patient to the operating theatre and before induction of anesthesia, all standard monitors were applied including Heart Rate (HR), Electrocardiogram (ECG), oxygen saturation (SpO2), end-tidal CO2, arterial blood pressure (systolic (SBP), diastolic (DBP) & mean (MAP)) and temperature. Additionally, monitoring of neuromuscular blockade by Train of Four (TOF) and BIS electrodes (BIS QUATRO-BX13366, Aspect Medical Systems, Inc. Chicago, USA) were connected to the patient.For continuous blood pressure monitoring and frequent blood gas analysis, a radial artery catheter was inserted after induction of anesthesia. Preoxygenation with 100% oxygen face mask for 5 min was done for all patients and anesthetic management was standardized for all patients as follows.
Anesthesia was induced by intravenous remifentanil (1µg /kg) over 30-60 seconds, followed by propofol 2 mg/kg. Intubation was facilitated with succinylcholine (1 mg/kg) and cuffed 7-7.5 mm endotracheal tube (Portex, Inc., London, England) was inserted. Maintenance of anesthesia was carried out by continuous infusion of remifentanil (0.25µg/kg/min), propofol infusion (3-5 mg/kg/h) and inspired oxygen fraction of 0.5 mixed with air. Anesthesia was titrated to keep the 'BIS' value within the range 40-50. Muscle relaxation was monitored by 'TOF' every ten minutes, rocuronium infusion from 0.2-0.6 mg/kg/hr was given and adjusted to maintain 1-2 twitches on the 'TOF' stimulation. Lungs were mechanically ventilated to maintain normocapnia (EtCO2 35-45 mmHg). All surgical procedures were done by the same surgeon who was blind about the study.
All vital signs were continuously monitored and recorded regularly throughout the procedure till the end of the surgery and extubation. Anesthesia was given to all patients by a single anesthetist who was not involved in the study and requested to follow the study design. Ringer acetate solution was set at a rate of 10 ml/kg/hr as a baseline infusion in all groups to assure optimization of intravascular volume and hemodynamic stability. Additional solutions were infused if required.
Pneumoperitoneum was generated by insufflating carbon dioxide into the abdomen with intra-abdominal pressure maintained at 12 cm H2O during the procedure. A bolus of normal saline 0.9% 250 ml and/or incremental doses of vasopressor drugs (ephedrine 5 mg or phenylephrine 50µg) was used for intraoperative hypotension (reduction in mean arterial blood pressure (MAP) > 25%). Discontinuation of all anesthetic agents and 100% oxygen ventilation were done at the end of surgical procedure. The residual effect of rocuronium was reversed with neostigmine in a dose of 40 µg/kg and atropine sulfate 20 µg/kg. Then after regaining patients’ spontaneous breathing, they were extubated and transferred to the Post Anesthesia Care Unit (PACU) for routine follow up. Postoperative analgesia was started with pethidine 50 mg IM every 8 hours paracetamol infusion 1 gm every 6 hours to keep Visual Analogue Scale (VAS) ≤ 4 . After fulfilling the recovery discharge criteria, patients were transferred to the ward. Chest X-ray was performed 2 hours postoperatively and 24 hours later to exclude any adverse effects of the recruitment maneuver.
2.3. Data for Assessment
- Hemodynamic Parameters: Heart Rate (HR), Mean Blood Pressure (MAP).
- Respiratory Mechanical Parameters: Peak Airway Pressure (Paw-peak), Plateau Pressure (Paw-plat) and End Expiratory Lung Volume (EELV).
- Oxygenation Parameters: Partial Arterial Oxygen tension (PaO2), Partial pressure of arterial oxygen/ fraction of inspired oxygen ratio (mmHg) and Oxygen saturation (SaO2).
All these measurements were performed at the following time intervals; T1 (baseline) preoperatively, T2 before induction of pneumoperitoneum, T3 immediately after induction of pneumoperitoneum, T4 30 minutes after pneumoperitoneum, and T5 60 minutes after pneumoperitoneum & T6 following pneumoperitoneum deflation and at the end of surgery. EELV was measured by nitrogen (wash-out/ wash-in) using an automated module available on the ventilator.
The primary outcome for the current study was to evaluate the efficacy of preemptive alveolar recruitment maneuver on pneumoperitoneum induced intraoperative hypoxemia (PaO2) while the secondary outcome was to assure pulmonary and extra-pulmonary safety of this maneuver. The pulmonary safety was assessed by monitoring of intraoperative changes in respiratory mechanics, arterial blood gases and chest X-ray in the recovery room to detect hypoxia or pneumothorax if present while the extra-pulmonary safety was assessed by monitoring the vital signs for the presence of hypotension or any arrhythmia.
2.4. Statistical Analysis and Sample Size
The collected data were coded, tabulated, and statistically analyzed using IBM SPSS statistics (Statistical Package for Social Sciences) software version 18.0, IBM Corp., Chicago, USA, 2009.
Descriptive statistics was done for quantitative data as mean ± SD (standard deviation) for quantitative normally distributed data while it was done for qualitative data as number and percentage.
For quantitative variables inferential analyses were done using the Shapiro-Wilk test for normality testing, and for the independent groups, an independent t-test was used. Mean ± SD and the 95% Confidence Interval (CI) were calculated for the differences between groups. Chi-square test was used for inferential analyses of independent variables in terms of qualitative data with the difference between proportions. The level of significance taken at p-value < 0.050 was significant, otherwise it was considered non-significant. The p-value is a statistical measure for the probability that the results observed in a study could have occurred by chance.
3. RESULTS
Regarding patients' characteristics and operative data (Table 1) there was no significant difference between both groups in this study.
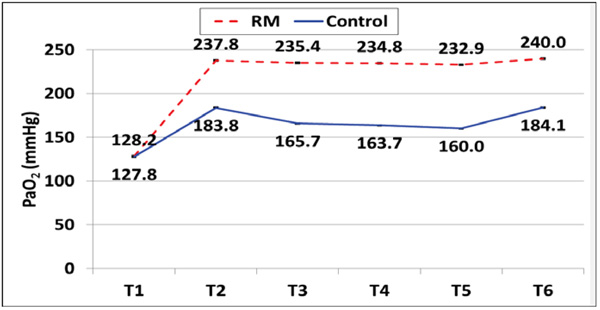
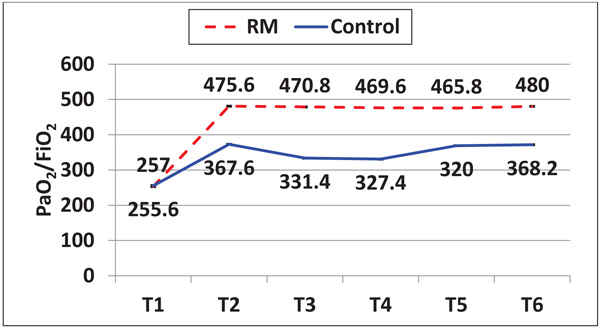
3.1. Arterial Oxygenation
This study documented that there was a significant reduction in PaO2 and PaO2/FiO2 ratio among patients in the control group (group C) throughout the procedure till the end of surgery and after deflation of pneumoperitoneum where they start to increase to reach baseline values. In contrast, both PaO2 and PaO2/FiO2 were significantly increased till the end of surgery and deflation of pneumoperitoneum (T6). These results demonstrated a significant difference between both groups regarding PaO2 and PaO2/FiO2 from T2 till the end of surgery and deflation of pneumoperitoneum (P < 0.05) (Figs. 2 and 3).
Regarding oxygen saturation, the results demonstrated that there were no significant differences between both study groups at all-time intervals (P> 0.05) (Fig. 4).
| Variables |
RM (N = 25) |
Control (N = 25) |
P | |
|---|---|---|---|---|
| Age (years) | 41.9 ± 3.7 | 40.4 ± 4.6 | ^ 0.202 | |
| Gender | Male | 8 (32.0%) | 9 (36.0%) | # 0.765 |
| Female | 17 (68.0%) | 16 (64.0%) | ||
| BMI (kg/m2) | 44.4 ± 2.5 | 44.5 ± 2.7 | ^ 0.889 | |
|
ASA (n, %) |
II | 15 (60.0%) | 16 (64.0%) | # 0.556 |
| III | 10 (40.0%) | 9 (36.0%) | ||
| Hemoglobin (gm/dl) | 13.0 ± 1.2 | 13.4 ± 1.0 | ^ 0.155 | |
| Surgery duration (minutes) | 90.0 ± 8.9 | 90.8 ± 9.7 | ^ 0.763 | |
| Anesthesia duration (minutes) | 101.0 ± 9.3 | 101.8 ± 10.1 | ^ 0.794 | |
3.2. Respiratory Mechanical Parameters
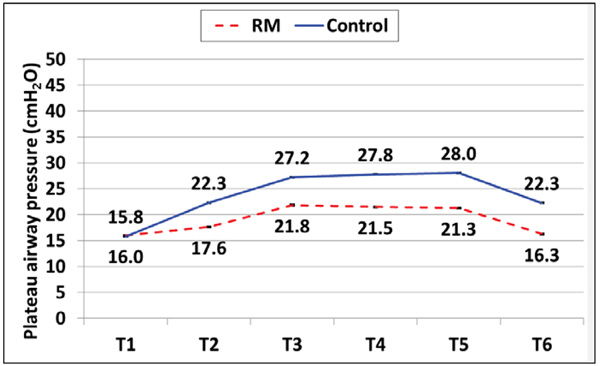
Peak and plateau airway pressures were increased significantly in the group C after initiation of pneumoperitoneum at T3 and stayed high throughout the procedure till surgery end and deflation of pneumoperitoneum (T6) where both parameters declined to lower values. Meanwhile, there was a slight non-significant increase in both parameters among the patients in the RM group throughout the procedure that decreased to readings near the baseline values by the end of surgery and deflation of pneumoperitoneum. Peak and plateau airway pressures showed a significant difference between both groups starting from T2 throughout the procedure till surgery end and deflation of pneumoperitoneum T6 (P < 0.05) (Figs. 5 and 6).


Regarding the End Expiratory Lung Volume (EELV), this study documented a dramatic decrease in EELV among the patients in the control group starting from T2 and continued low during the procedure till T5 then started to increase following pneumoperitoneum deflation at T6. On the other hand, patients in the RM group showed a significant increase in EELV after application of RM and PEEP then continued high till T4 after that declined but still higher than the baseline values at T5 and finally, increased again significantly after pneumoperitoneum deflation at T6. There was a statistically significant difference between both study groups regarding EELV (P < 0.05) (Fig. 7).
4. DISCUSSION
Data from our study demonstrated that Recruitment Maneuver (RM) application followed immediately with 15 cm H2O Positive End Expiratory Pressure (PEEP) before initiation of pneumoperitoneum in patients undergoing laparoscopic gastric banding was effective in improvement of intraoperative oxygenation and prevention of hypoxemia. Moreover, there were great improvements in respiratory mechanics without any harmful effects on patients’ hemodynamic parameters.
4.1. Oxygenation and Gas Exchange
This study documented that there was a marked increase in both PaO2 and PaO2/FiO2 among the patients in RM group with a significant difference when compared with patients in the control group (P < 0.05). This increase started after application of RM and before pneumoperitoneum initiation and continued high throughout the procedure.
Our results were in agreement with the results of other multiple randomized control studies that assessed the effects of using alveolar recruitment maneuver together with PEEP on intraoperative oxygenation, respiratory mechanics and postoperative complications. Regardless of the method used for the application of RM, positive results were achieved across these studies in terms of respiratory mechanics and oxygenation [7-11].
In contrast to our study, some other studies proved that application of PEEP alone was not effective in improving intraoperative oxygenation during laparoscopic abdominal surgeries [12, 13]. Both groups showed no significant difference regarding peripheral oxygen saturation (P > 0.05) and this can be explained by the plateau of oxyhemoglobin dissociation curve near 100% saturation.
4.2. Respiratory Mechanics
Present study results showed an abrupt increase in both peak and plateau airway pressures among the patients in the control group with a significant difference when compared with patients in the RM group (P < 0.05). This elevation in both pressures started after positioning and before induction of pneumoperitoneum then, continued throughout the procedure till end of surgery and deflation of pneumoperitoneum. This can be explained by the application of PEEP after RM was successful in counterbalance the pneumoperitoneum-induced cranial shift of the diaphragm giving more space for lung expansion.
Our results were consistent with the results of the study done by Cinnella, et al. [11] who studied the effects of Recruitment Maneuver (RM) and Positive End Expiratory Pressure (PEEP) on respiratory mechanics and transpulmonary pressure during laparoscopic surgery and documented that RM together with PEEP was able to reduce the pneumoperitoneum induced changes in respiratory mechanics.
Also, our results were supported by another study done by Futier E, et al. [13] who concluded that application of 10 cmH2O PEEP combined with RM was successful in counteracting the detrimental effects of pneumoperitoneum in both healthy weight and obese patients undergoing laparoscopy.
In terms of End Expiratory Lung Volume (EELV), the present study demonstrated a dramatic increase in EELV among patients in RM group with a significant difference when compared with the control group patients (P < 0.05). This increase started before induction of pneumoperitoneum then, continued high till 30 minutes after that, there was a slight decrease that improved dramatically at the end of surgery and deflation of pneumoperitoneum.
Our results were consistent with those of Futier E, et al. [13], who found that application of RM and PEEP of 10 cm H2O was associated with a greater increase in EELV compared with PEEP alone in both healthy weight and obese patients undergoing laparoscopy.
Moreover, Maisch S, et al. [14], reported that RM followed by high PEEP levels was necessary to increase EELV during laparoscopy.
4.3. Safety of the Recruitment Maneuver
The results of the current study showed no significant changes between both groups regarding Mean Arterial Blood Pressure (MAP) and Heart Rate (HR) (P > 0.05). This can be explained by optimization of intravascular volume load for our patients by crystalloid infusion. Our results were in agreement with those of Bohm, et al. [15], who confirmed the hemodynamic safety of RM and application of PEEP in intravascular volume loaded patients.
In contrast, one study documented a significantly higher dose of vasopressor used for patients in the recruitment maneuver group compared with the control group [6].
There was no incidence of hypoxia, infection or pneumothorax in both study groups. Our results were in agreement with the results of other many studies that documented the safety of RM and PEEP and they didn’t report any case of barotrauma [7-9].
CONCLUSION
Preemptive application of recruitment maneuver CPAP 40 cm H2O for 45 seconds followed immediately with PEEP of 15 cm H2O was safe and effective in improving the intraoperative oxygenation and preventing the pneumoperitoneum-induced detrimental respiratory mechanics effects in obese patients undergoing laparoscopic gastric banding.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE HUMAN RIGHTS
All clinical investigations were carried out after obtaining the approval of our institutional ethics and research committee (FMASU R64/2018).
HUMAN AND ANIMAL RIGHTS
No animals were used in the study. All humans research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2008 (http://www.wma. net/en/20activities/10ethics/10helsinki/).
CONSENT FOR PUBLICATION
Written informed consent was taken from all patients who participated.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


