All published articles of this journal are available on ScienceDirect.
Levosimendan Versus Milrinone in the Management of Impaired Left Ventricular Function in Patients Undergoing Coronary Artery Bypass Graft Surgery
Abstract
Background:
Patients undergoing cardiac surgery are at risk of postcardiotomy myocardial dysfunction. This condition causes delayed recovery, organ failure, prolonged intensive care unit and hospital stays, and an increased risk of mortality; these patients often require inotropic agent support. Levosimendan is a calcium sensitizer with a unique mechanism of action, binding to cardiac troponin C and enhancing myofilament responsiveness to calcium, increasing myocardial contraction without increasing myocardial oxygen consumption. Phosphodiesterase III inhibitors such as milrinone provide an alternative means of inotropic support by increasing the concentration of cyclic AMP and intracellular calcium. They also have vasodilatory effects.
Objective:
The aim of this study was the comparison between levosimendan versus milrinone regarding their effects on the hemodynamics, need for additional mechanical (intra aortic balloon pump) or pharmacological support to the heart, weaning from mechanical ventilation and duration of intensive care unit stay for patients after Off-Pump Coronary Artery Bypass Graft (OPCABG) surgery suffering from impaired left ventricular function (preoperative ejection fraction ≤ 40%).
Methods:
60 patients between 40 and 70 years of both sexes with impaired left ventricular function (ejection fraction ≤ 40%), New York Heart Association (NYHA III & IV), undergoing elective Off-Pump Coronary Artery Bypass Graft (OPCABG) surgery were selected for this study. After induction of anesthesia, patients were randomly assigned to one of two equal groups each containing 30 patients:
Group L (Levosimendan group) included patients who received levosimendan 0.1- 0.2 µg/kg/min. Started immediately with the induction of anesthesia.
Group M (Milrinone group) included patients who received milrinone 0.4-0.6 µg/kg/min. Started immediately with the induction of anesthesia.
In both groups, norepinephrine was titrated (8 mg norepinephrine in 50 ml saline) to keep mean arterial pressure MAP ≥ 70 mmHg.
Hemodynamic findings included Preoperative and post ICU discharge ejection fraction, systemic and pulmonary artery pressures, systemic and pulmonary vascular resistance, cardiac output and stroke volume. Also laboratory findings included Serum lactate and Troponin I., in addition, to post operative findings were: Need for intra aortic balloon pump, time of weaning from the ventilator, days of ICU stay and appearance of drug allergy compared in both groups.
Results:
There was a significant increase in the ejection fraction in both groups that was greater in the levosimendan group. The decrease in pulmonary pressure in the levosimendan group was more significant than milrinone group. There was a gradual decrease in pulmonary and systemic vascular resistance in both groups with a more significant decrease in the levosimendan group. There was a gradual increase in cardiac output and stroke volume in both groups that was greater in the levosimendan group. Serum lactate gradually decreased in both groups with an insignificant difference; there was an increase in serum troponin I level in both groups which was more significant in the milrinone group. Weaning from mechanical ventilation and length of ICU stay was shown to be significantly shorter in time in the levosimendan group.
Conclusion:
Both levosimendan and milrinone caused a significant increase in cardiac output, stroke volume and ejection fraction, with a decrease in pulmonary and systemic vascular resistance. These effects improved cardiac performance by decreasing afterload and increasing cardiac inotropism. It was noticed that these effects were more significant with levosimendan than milrinone. Also, there was a decrease in ICU stay, mechanical ventilation timing and hospital stay with levosimendan than milrinone which decreased the costs of treatment for the patients.
1. INTRODUCTION
Patients undergoing cardiac surgery are at risk of postcardiotomy myocardial dysfunction. This condition causes delayed recovery, organ failure, prolonged intensive care unit and hospital stays, and an increased risk of mortality. These patients often require inotropic support, which has been associated with an increased risk of cardiovascular complications [1]. Treatment of myocardial dysfunction includes optimization of myocardial contractility through appropriate fluid and pharmacologic management and mechanical support [2]. Extensive use of inotropes in this situation is needed, but the optimal pharmacologic management of myocardial dysfunction in cardiac surgery is a matter of ongoing debate [3]. The occurrence of myocardial dysfunction after cardiac surgery is a potential indication for the use of levosimendan, a calcium sensitizer with a unique mechanism of action. By binding to cardiac troponin C, it enhances myofilament responsiveness to calcium, thereby increasing myocardial contraction without increasing myocardial oxygen consumption. In addition, levosimendan activates adenosine triphosphate-dependent potassium channels, which are important mediators of ischemic and anesthetic cardioprotection. Levosimendan might thus have a potential benefit for patients with myocardial oxygen imbalance requiring inotropic drug support [4].
Phosphodiesterase III (PDE III) inhibition by agents such as milrinone provides an alternative means of inotropic support by increasing the concentration of cyclic Adenosine Monophosphate (cAMP), and thereby intracellular calcium [5]. Phosphodiesterase (PDE) inhibitors also have vasodilatory effects due to PDE inhibition in vascular smooth muscle cells [6]. Available inotropes including PDE inhibitors may increase myocardial oxygen consumption, heart rate and risk of arrhythmias. An increase in myocardial oxygen consumption by inotropes in a state of inadequate oxygen delivery may further deteriorate underlying heart failure and even lead to increased mortality [7].
The aim of this study was the comparison between levosimendan versus milrinone, regarding their effects on the hemodynamics, need for additional mechanical (intra aortic balloon pump) or pharmacological support to the heart, weaning from mechanical ventilation and the duration of Intensive Care Unit (ICU) stay for patients after Off-Pump Coronary Artery Bypass Graft (OPCABG) surgery who were suffering from impaired left ventricular function (preoperative ejection fraction ≤ 40%).
2. METHODS
The study was approved by the department of anesthesia, faculty of medicine, Ain-Shams University and Ethical and Scientific Committees and informed consent was obtained from the patients. The study was conducted in cardiothoracic surgery operating theater, El-Maadi military hospital.
2.1. Inclusion Criteria
60 patients, between 40 and 70 years of both sexes with impaired left ventricular function (Ejection fraction ≤ 40%), mean pulmonary artery pressure between 25-35 mmHg, New York Heart Association (NYHA III & IV), undergoing elective Off-Pump Coronary Artery Bypass Graft (OPCABG) surgery were selected for this study.
2.2. Exclusion Criteria
Geriatric patients (age over 70 years), patients with end-organ failure (renal, liver), perioperative surgical complications unrelated to the study (accidental surgical trauma to a nearby organ or massive blood loss defined as blood loss exceeding circulating blood volume within a 24-hour period due to surgical insult) and associated mitral valve stenosis or aortic valve stenosis.
2.3. Monitoring
All patients were monitored using:
(1) Five-lead electrocardiogram, pulse oximetry, invasive arterial blood pressure, pulmonary artery catheter to measure the pulmonary artery pressure (systolic, diastolic and mean), pulmonary capillary wedge pressure, cardiac output, pulmonary vascular resistance and systemic vascular resistance.
(2) Nasopharyngeal temperature, urine output, arterial blood gases, end tidal Carbon dioxide (CO2).
2.4. Anesthetic Management
2.4.1. Premedication
All preoperative cardiac medications were continued until the morning of surgery except for Angiotensin Converting Enzyme Inhibitors (ACEI), which were stopped one day before surgery and aspirin stopped four days before surgery. Patients were premedicated with oral diazepam 5 mg the evening before surgery. Upon arrival at the pre-induction room, the patients received supplementary oxygen via nasal prongs, and were monitored with standard American Society of Anesthesio- logists (ASA) monitors. After local infiltration of lidocaine 2%, a peripheral venous cannula (14 or 16 Gauge) and left radial 20 Gauge arterial cannula were inserted.
2.4.2. Induction
Induction of anesthesia was achieved by Intravenous (IV) fentanyl (10 µg/kg), thiopentone (5 mg/kg), and pancuronium (0.1 mg/kg).
After intubation, a triple lumen central venous catheter and a pulmonary artery catheter were inserted via the right internal jugular vein. A temperature probe was inserted in the naso- pharynx.
After induction of anesthesia, patients were randomly assigned to one of two equal groups each containing 30 patients:
Group L (Levosimendan Group) included patients who received levosimendan 0.1 µg/kg/min. started immediately with the induction of anesthesia.
Group M (Milrinone Group) included patients who received milrinone 0.5 µg/kg/min. started immediately with the induction of anesthesia.
In both groups, norepinephrine was titrated (8 mg norepinephrine in 50 ml saline) to keep Mean Arterial Pressure (MAP) ≥ 70 mmHg, if hypotension occurred, which might result from the drop of systemic vascular resistance with the induction of anesthesia or with the introduction of milrinone or levosimendan.
2.4.3. Maintenance
All the patients were mechanically ventilated with 80% oxygen/air and respiratory rate and tidal volumes were adjusted to ensure adequate oxygenation (SpO2 ≥ 95%) and CO2 elimination (Et CO2 35-45 mmHg). Anesthesia was maintained with sevoflurane 1 to 2 percent, as well as fentanyl increments of 2-5 µg/kg to achieve an adequate level of anesthesia and hemodynamic stability. Muscle relaxation was maintained by pancuronium infusion (0.02-0.03 mg/kg/hr).
In all patients, the central venous pressure was kept between 6 and 9 cm H2O and pulmonary capillary pressure between 15 and 18 mmHg by the administration of intravenous fluids (colloids and crystalloids). Concentrations of milrinone or levosimendan were kept constant until the patient was transferred to ICU. When all vital signs and hemodynamics were stable, inotropic support was weaned. Hypotension was defined as mean blood pressure ≤ 60 mmHg, and was treated with norepinephrine 0.1-0.3 μg/kg/min. During manipulation of the heart and use of octopus stabilizer, any drop in the blood pressure was treated using increments of titrated norepinephrine to keep Mean Arterial Pressure (MAP) ≥ 70 mmHg. During grafting, the surgeons used coronary shunt to maintain coronary artery flow and Glyceryl Trinitrate (GTN) 1 mg/ml was infused at a rate of 0.5-5 ml/hour to overcome any ischemic changes.
2.5. Weaning from Mechanical Ventilation, Extubation and Duration of ICU Stay
Weaning from mechanical ventilation followed a standard protocol using the following criteria: temperature > 36°C, stable hemodynamics (defined as the ability to increase body oxygen consumption (e.g., spontaneous breathing) without the need for increased inotropic support), chest tube drainage < 100 mL/h and urine output ≥ 0.5 mL/kg/h.
The patient’s trachea was extubated when the following criteria were achieved: adequate response to command, SpO2 ≥ 95% at FiO2 ≤ 0.5, pH ≥ 7.3, PaCO2 ≤ 55 mm Hg, and respiratory rate < 30 breaths per minute (bpm).
Patients were discharged from the Intensive Care Unit (ICU) when the following criteria were met: SpO2 ≥ 92% at FiO2 ≤ 0.5 by facemask, stable hemodynamics, chest tube drainage < 50 mL/h, urine output > 0.5 mL/kg/h, no intravenous inotropic or vasopressor therapy.
2.6. Data Collection
2.6.1. Demographic Data:
- Age, sex, weight, height.
Preoperative and after ICU discharge ejection fraction:
2.6.2. Hemodynamic Parameters:
- Invasive (systolic, diastolic and mean arterial blood pressure)
- Via pulmonary artery catheter we measured:
Pulmonary Artery Pressure (PAP), mean systemic-to-pulmonary artery pressure ratio, Pulmonary Vascular Resistance (PVR), Systemic Vascular Resistance (SVR), cardiac output and stroke volume.
- Heart rate.
Hemodynamic variables were recorded preoperatively, intraoperatively and postoperatively.
2.6.3. Laboratory Measurements:
Laboratory measurements were done preoperatively, intraoperatively and postoperatively including:
Troponin I, serum lactate, hematocrit (Hct) and Arterial Blood Gases (ABG).
2.6.4. Post Operative Findings:
Need for intra aortic balloon pump, time of weaning from the ventilator, days of ICU stay and the appearance of any drug allergy.
3. STATISTICAL ANALYSIS
Statistical analysis was performed using SPSS (Statistical Package for the Social Sciences) version 15, Echosoft Corp., U.S.A. Data were represented as mean ± standard deviation. Independent samples t-test was used to compare variables between the two studied groups. Repeated measures Analysis of Variance (ANOVA) test was used to compare three variables within the same group. Post Hoc test was done to identify the different group if ANOVA test was positive. In all tests, the result was considered statistically significant if the p- value was less than 0.05.
4. RESULTS
4.1. Demographic Data
The demographic data for the study groups are shown in Table 1.
4.2. Preoperative and Post ICU Discharge Ejection Fraction
Ejection fraction as measured by echocardiography at the time of ICU discharge compared to ejection fraction measured preoperatively.
Comparing group L and group M, there was a significant increase in ejection fraction in both groups, with a more significant increase in L group (Table 2).
4.3. Systemic Systolic, Diastolic and Mean Arterial Blood Pressures
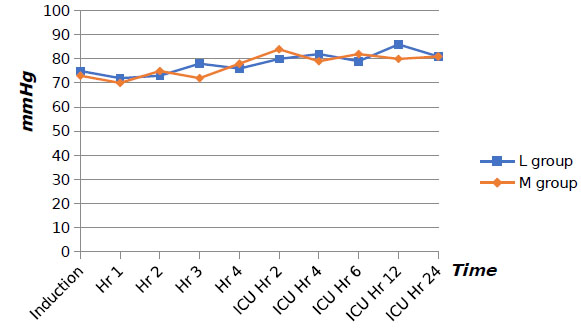
Comparing group L and group M, there were no significant changes in systolic, diastolic and mean Arterial Blood Pressures (ABP) (Fig. 1) respectively in both groups from time of induction of anesthesia, during surgery and for the first 24 hours in the ICU.
4.4. Pulmonary Systolic, Diastolic and Mean Arterial Blood Pressure
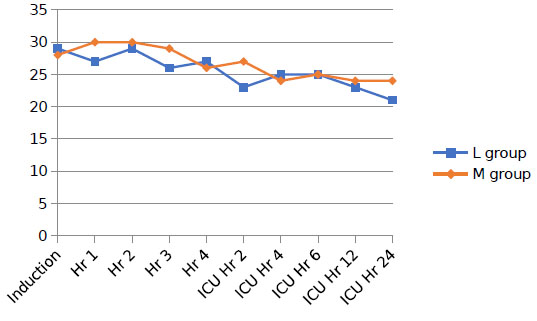
Comparing group L and group M, there was a gradual decrease in systolic, diastolic and mean Pulmonary Arterial Pressure (PAP) (Fig. 2) respectively in either groups from the time of induction of anesthesia, during surgery and for the first 24 hours in the ICU, with significantly more decrease in group L.
| Demographic Data | Group L | Group M |
|---|---|---|
| Number of cases | 30 | 30 |
| Sex(Male/Female) | 22/8 | 18/12 |
| Age (Years) | 56.7 ± 11.4 | 54.4 ± 14.6 |
| Weight (Kg) | 84 ± 13 | 83.6 ± 11.6 |
| Height (Cm) | 171.3 ± 15.4 | 168.7 ± 13.7 |
| - | Group L | Group M |
|---|---|---|
| Preoperative ejection fraction | 31.7 ± 7.4 | 33.26 ± 6.2 |
| Ejection fraction after ICU discharge | 49.23 ± 4.77*‡ | 42.9 ± 5.1* |
4.5. Mean Systemic to Pulmonary Pressure Ratio
Comparing group L and group M, there was a gradual increase in mean systemic to pulmonary artery pressure ratio in both groups from the time of induction of anesthesia, during surgery and for the first 24 hours in the ICU, with significantly more increase in group L.
4.6. Pulmonary Vascular Resistance
Comparing group L and group M, there was a gradual decrease in pulmonary vascular resistance in both groups from the time of induction of anesthesia, during surgery and for the first 24 hours in the ICU, with significantly more decrease in group L, and slight increase in PVR in group M after stoppage of the infusion of both drugs.
4.7. Systemic Vascular Resistance
Comparing group L and group M, there was a gradual decrease in systemic vascular resistance in both groups from the time of induction of anesthesia, during surgery and for the first 24 hours in the ICU, with significant continuing decrease in SVR in group L after stopping the infusion of both drugs.
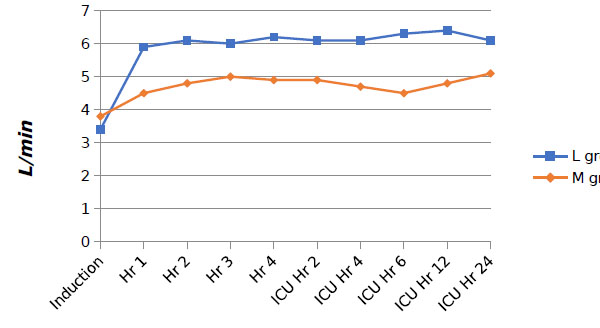
4.8. Cardiac Output
Comparing group L and group M, there was a gradual increase in cardiac output in both groups from time of induction of anesthesia, during surgery and for the first 24 hours in the ICU, with significantly more increase in group L (Fig. 3).
4.9. Stroke Volume
Comparing group L and group M, there was a gradual increase in stroke volume in both groups from the time of induction of anesthesia, during surgery and for the first 24 hours in the ICU, with significantly more increase in group L.
4.10. Heart Rate
Comparing group L and group M, there was no significant difference in heart rate in both groups.
4.11. Serum Lactate
Comparing group L and group M, there was a gradual decrease in serum lactate in both groups from baseline, during surgery and for the first 48 hours in the ICU, with an insignificant difference in both groups which indicates adequate tissue perfusion in both groups.
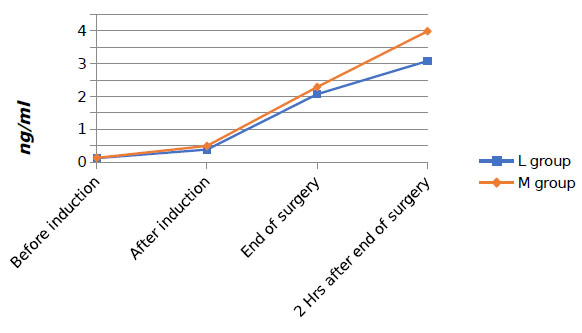
4.12. Troponin I
Comparing group L and group M, there was an increase in serum troponin I in both groups but the increase of serum troponin I in group M was more statistically significant that indicates less myocardial tissue injury in group L (Fig. 4).
Postoperatively, the need for Intra Aortic Balloon Pump (IABP), weaning from mechanical ventilation and the days spent in ICU are shown in Table 3.
5. DISCUSSION
For many years, post-ischemic dysfunction was treated with catecholamines, despite the fact that these drugs impair the calcium balance of the cardiomyocytes. Catecholamines have a desired positive inotropic effect but it also induces several undesired effects such as arrhythmias, cell death, systolic and diastolic dysfunction as well as impairing the relationship between cardiac function and oxygen consumption [8]. This study was designed to compare the effects of levosimendan versus milrinone in the management of impaired left ventricular function in patients undergoing coronary artery bypass graft surgery. In our study, comparing the ejection fraction preoperatively and after the patient discharge from the ICU in both groups, there was a significant increase in ejection fraction in both groups with a more statistically significant increase in group L; this may be due to the dual effect of levosimendan as noted above, in addition to the prolonged effect of its active metabolite. Our results were similar to those seen by many previous studies such as the study performed by Righetti and colleagues. They compared levosimendan versus dobutamine in Takotsubo cardiomyopathy. The patients were divided randomly into two groups: levosimendan (six patients) treated with levosimendan and standard treatment, and the control group (six patients) with dobutamine and standard treatment. Left ventricular systolic function was evaluated with serial Trans-Esophageal Echocardiograms (TEE). A TEE was done at baseline and then after 12 and 24 hours of treatment. In the levosimendan group, the ejection fraction at entrance was 25 ± 6%, after 12 hours 36 ± 10%, and 47 ± 5% after 24 hours. In the control group, the ejection fraction at entrance was 24 ± 7%, after 12 hours 28 ± 6% and after 24 hours 33 ± 4% [9].
| Post Operative Findings | Group L | Group M |
|---|---|---|
| Need for IABP | 0/30 | 3/30 |
| Weaning from ventilator (hours) | 12.26±6.2‡ | 18.76±9.8 |
| ICU stay (Days) | 3.35±1.26‡ | 4.25±1.75 |
| Appearance of drug allergy | -Ve | -Ve |
Results of the current study showed that there were no significant changes in the systemic systolic, diastolic and mean ABP and the heart rate, from the time of induction of anesthesia, during surgery and for the first 24 hours in the ICU in both groups as a result of adherence to the protocol for maintaining these variables within specified range. This was achieved by using norepinephrine infusion to maintain the mean MAP ≥ 70 mmHg, also, adequate analgesia with fentanyl to eliminate stress and pain factors on heart rate and blood pressure. Yet, we noticed a slight gradual increase in mean arterial blood pressure in both groups due to the positive inotropic effect of levosimendan and milrinone and their positive effect on the cardiac output. Our results are similar to those of Al-Shwaf and colleagues comparing the effects of levosimendan versus milrinone in patients with type II diabetic patients with low ejection fraction undergoing elective coronary artery graft surgery, where there was stability in systemic arterial blood pressures and also heart rate due to adequate analgesia with sufentanil infusion (0.5 µg/kg/hr) and sevoflurane for anesthesia, in addition to norepinephrine infusion to maintain the mean MAP ≥ 70 mmHg [2].
In another study performed by Julián Álvarez and colleagues, on the hemodynamic effects of levosimendan compared with dobutamine in patients with low cardiac output after cardiac surgery, the result of measuring MABP showed initial reduction and instability which disagreed with the present study. This was because in this study, they administered levosimendan as loading dose of 12 μg/kg over 15-20 min, followed by infusion of 0.2 μg/kg/min for 24 h. while in the current study, we did not give a loading dose which may be more effective in maintaining the arterial blood pressure stable [10]. There was a gradual decrease in pulmonary systolic, diastolic and mean ABP in both groups from the time of induction of anesthesia, during surgery and for the first 24 hours in the ICU, this was due to the direct effect of levosimendan and milrinone on decreasing the pulmonary vascular resistance, and their inotropic effect on left ventricle that helps in decreasing pulmonary congestion. The decrease in pulmonary pressure in group L was more significant in comparison to group M which means that levosimendan is more effective in reducing pulmonary artery pressure. These results agreed with the study performed by De Hert and colleagues on the effects of levosimendan in cardiac surgery patients with poor left ventricular function in comparison with milrinone. In this study, thirty patients with a preoperative ejection fraction ≤ 30% scheduled for elective cardiac surgery with cardiopulmonary bypass were randomized to two groups: milrinone group (0.5 μg/kg/min) and levosimendan group (0.1 μg/kg/min), started immediately after the release of the aortic cross-clamp. The treatment was masked to the observers. All the patients received dobutamine (5 μg/kg/min). There was a gradual reduction in Mean Pulmonary Artery Pressure (MPAP) in levosimendan and milrinone groups from baseline and for the first 24 hours in the ICU [5].
A gradual increase in cardiac output and stroke volume in both groups from time of induction of anesthesia, during surgery and for the first 24 hours in the ICU, with a significantly more increase in group L. Phosphodiesterase III inhibitors such as milrinone enhanced myocardial contractility by increasing the concentration of cyclic AMP, and thereby intracellular calcium. This action resulted in an increase in myocardial oxygen consumption. In contrast, levosimendan improved myocardial contractility primarily by enhancing myocardial contractile protein sensitivity to calcium without increasing its intracellular concentration. This action does not result in an increase in myocardial oxygen consumption. Levosimendan may, therefore, have a more advantageous profile than phosphodiesterase III inhibitors, especially in patients with a compromised myocardial oxygen balance [11].
Serum lactate level is an indication for the adequacy of tissue perfusion which reflects the efficacy of heart performance. It was noticed that serum lactate gradually decreases in both groups indicating effective results of both drugs on cardiac output and tissue perfusion.
Serum troponin I is an indicator of myocardial tissue injury. There was an increase in serum Troponin I level in both groups due to several effects including surgical manipulations and chemical injury of the drugs used. The increase of troponin I in group M was more obvious, which might be due to the cardioprotective effect of levosimendan because of its facilitation of adenosine triphosphate dependent potassium channel opening. This protection might also be a consequence of the favorable effect of this drug on the myocardial oxygen supply-demand balance. These result coincides with a study done by Tritapepe and colleagues which detected the preconditioning effects of levosimendan in coronary artery bypass grafting [12].
In the present study, comparing the two groups, three patients in group M required IABP as a mechanical support to keep Mean Arterial Blood Pressure (MABP) above 70 mmHg because of failure of milrinone with norepinephrine as inotrope and vasopressor respectively alone in these three cases to keep MABP ≥ 70 mmHg, so IABP was used to increase the diastolic pressure and support the coronary perfusion. While in group L, there was no need for any mechanical support. It was not a significant result because many causes may lead to this result such as the blood loss, preoperative ejection fraction of the cases and surgical manipulations. This is consistent with results from previous studies that found lower incidence of IABP use with levosimendan than with milrinone as the study done by De Hert and colleagues where four patients in group L and group M had an IABP inserted preoperatively. The duration of mechanical inotropic support was shorter in group L, (171 ± 55 hours in group M versus 41 ± 22 hours in group L) [5].
Weaning from mechanical ventilation and length of ICU stay were associated with significantly shorter time in group L. The results of the current study showed superiority of levosimendan over milrinone in reducing the time of mechanical ventilation and duration of ICU stay. These results go with many previous studies; the study done by Al-Shwaf and colleagues compared the effects of levosimendan versus milrinone in type II diabetic patients with low ejection fraction undergoing elective coronary artery graft surgery. Mechanical ventilation time was 1.4 ± 1.3 days in group L versus 2.7 ± 2.75 days in group M, duration of ICU stay was 7.7 ± 10.5 days in group L versus 13 ± 33 days in group M [2].
Our conclusion was also homogenous with the conclusion of a systematic review and meta-analysis by Wang W and colleagues evaluating the efficacy and safety of prophylactic use of levosimendan in CABG surgery. They found that levosimendan was a well-tolerated, effective inotropic agent in patients undergoing CABG, which was associated with a significantly reduced mortality rate and postoperative atrial fibrillation especially when administrated preoperatively, with a bolus and during on-pump CABG [13].
Limitations of this study which may have contributed to discrepancies between its results and the results of similar studies include surgical related factors as surgeon skill and experience and preoperative laboratory data of the patient as hemoglobin and hematocrit levels.
CONCLUSION
In conclusion, both levosimendan and milrinone cause a significant increase in cardiac output, stroke volume and ejection fraction, with a decrease in pulmonary and systemic vascular resistance. These effects improve cardiac performance by decreasing afterload and increasing cardiac inotropism. It was noticed that these effects were more significant with levosimendan than milrinone; this may be due to the unique characteristics of levosimendan mechanism of action mentioned before over other inotropes including phospho- diesterase III inhibitors (milrinone), which gives superiority for the use of levosimendan in ventricular dysfunction. Also, the decrease in ICU stay, mechanical ventilation timing and hospital stay with levosimendan than milrinone decreased the costs of treatment over the patients.
It is evident that hospital days are the main cost driver in Heart Failure (HF) after coronary artery bypass graft surgery; any treatment that reduces heart failure hospitalizations is more likely to be cost-effective compared with other accepted health interventions. In all related studies which compare the use of levosimendan versus other inotropes, Levosimendan has the priority due to shorter ICU and hospital stay time; which adds as a cost benefit to the use of levosimendan [14].
LIST OF ABBREVIATIONS
| HF | = Heart Failure |
| LV | = Left Ventricular |
| CABG | = Coronary Artery Bypass Graft |
| MAP | = Mean Arterial Pressure |
| OPCABG | = Off-Pump Coronary Artery Bypass Graft |
| NYHA | = New York Heart Association |
| cAMP | = cyclic Adenosine Monophosphate |
| PDE | = Phosphodiesterase |
| ICU | = Intensive Care Unit |
| CO2 | = Carbon dioxide |
| ACEI | = Angiotensin Converting Enzyme Inhibitors |
| ASA | = American Society of Anesthesiologists |
| IV | = Intravenous |
| GTN | = Glyceryl Trinitrate |
| PAP | = Pulmonary Artery Pressure |
| PVR | = Pulmonary Vascular Resistance |
| SVR | = Systemic Vascular Resistance |
| SPSS | = Statistical Package for the Social Sciences |
| ANOVA | = Analysis of Variance |
| ABP | = Arterial Blood Pressures |
| IABP | = Intra Aortic Balloon Pump |
| TEE | = Trans-Esophageal Echocardiograms |
| MPAP | = Mean Pulmonary Artery Pressure |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the ethical and scientific committees of the Department of Anesthesia, Faculty of Medicine, Ain-Shams University.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from the patients.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


