All published articles of this journal are available on ScienceDirect.
The Feasibility and Applications of Non-invasive Cardiac Monitoring in Obese Patients Undergoing Day-case Surgery: Results of a Prospective Observational Study
Abstract
Aims:
This prospective observational study evaluates the utility of non-invasive cardiac monitoring in obese patients in the day-surgery case, considering factors, such as Body Mass Index (BMI) and anaesthesia technique.
Background:
Obese patients are more likely to be admitted to hospital or to get hospitalized because they are more prone to concomitant diseases and obesity itself is not a contraindication to day surgery. Obese patients are a high-risk patient population that may particularly benefit from monitoring perioperative haemodynamic variations.
Methods:
In this observational study, we compared haemodynamic variations between overweight or obese and normal weight patients undergoing day-case surgery. We adopted NICOM® as a non-invasive cardiac output monitoring.
Objective:
The aim of the current study was to investigate the haemodynamic impact of BMI and anaesthesia technique during day-case surgery procedures. The other goal was to evaluate the feasibility and applications of non-invasive cardiac output monitoring among the obese population in day-surgery.
Results:
74 patients were included in the study. 34 were overweight or obese (weight 84 ± 10 kg, height 160 ± 10 cm, BMI ≈ 30 kg/m2), 40 were normal weight (weight 63 ± 15 kg, height 160 ± 10 cm, BMI ≈ 22 kg/m2). Compared to normal-weight patients, obese patients show an increase in blood pressure with a return to baseline values at the end of surgery (p < 0.05). The Cardiac Output (CO) shows a similar trend, whereas the heart rate is normal. A decrease in the Cardiac Index (CI) during the operation was noticed in both groups, the one in obese patients (p = 0.24) being greater. In the same way, the Stroke Volume Index (SVI) was lower in obese patients during surgery (p < 0.05). In spinal anaesthesia, the Total Peripheral Resistance Index (TPRI) was not statistically different between the groups of study. As for the TPRI in obese patients, we reported values similar to the ones in non-obese patients in spinal anaesthesia. In local anesthesia, TPRI was higher in obese patients than in non-obese.
Conclusion:
Cardiovascular alterations in relation to obesity include an increase in blood pressure, CO and SV. An inadequate monitoring of haemodynamic parameters is a risk factor for perioperative complications. NICOM® provides a continuous, non-invasive haemodynamic measurement.
1. INTRODUCTION
1.1. Rationale
Obesity is a medical problem. Currently, in the United States, the prevalence of obesity is 39.8% and affects about 93.3 million adults [1].
Obese patients are more likely to get to the hospital because they are more prone to concomitant diseases [2]. Obesity itself is not a contraindication to day surgery [3] and obese patients benefit from short-duration anaesthetic techniques and early mobilisation associated with outpatient surgery [2, 4].
Obese patients are a high-risk patient population that may particularly benefit from monitoring perioperative cardiac output due to their increased risk of cardiac and non-cardiac morbidity and mortality in the case of surgery [4].
In the perioperative medicine, haemodynamic management aims to optimize perfusion pressure and oxygen delivery to maintain adequate cellular metabolism [5]. To optimize cardiopulmonary function, haemodynamic management aims at the administration of fluids and vasoactive agents based on the predefined target values of haemodynamic variables. This is the so-called “goal direct therapy”, that has been shown to improve the patient’s outcome [6-10].
Cardiovascular alterations related to obesity include an increase in the total blood volume, Cardiac Output (CO) and Stroke Volume (SV), that grows linearly with body weight [11].
In the past, the measurement of advanced haemodynamic variables required invasive haemodynamic monitoring. Recently, different non-invasive haemodynamic monitoring technologies have been proposed [12]. In general, they permit the estimation of CO and other haemodynamic variables without needing arterial or central venous cannulation. In addition, their use in clinical practice is relatively easy and does not require extensive training. On the other hand, all the available technologies still have technical limitations with regard to their clinical applicability [12].
Among these, Non-Invasive Cardiac Output Monitor (NICOM®, Cheetah Medical Inc., Portland, OR, USA) is a bioreactance-based technology [13, 14]. The bioreactance signal is determined by measuring blood flow-dependent changes in the phase shifts between an oscillating electrical current applied across the thorax and the resulting voltage signal. This signal has been shown to be directly proportional to aortic blood flow [13]. Importantly, this technology is independent of patient physical characteristics. Indeed, body mass does not impact the haemodynamic monitoring systems' results. Although obese patients now make up a significant part of the anaesthesia population, studies on the applicability of this non-invasive cardiac output measurement device in this specific population remain limited.
1.2. Objectives
The aim of the current study was to investigate the haemodynamic impact of Body Mass Index (BMI) and anesthesia technique during day-case surgery procedures. The other endpoint was to evaluate the feasibility and applications of non-invasive cardiac output monitoring among obese population in day-surgery.
2. METHODS AND MATERIALS
The current study was approved by the local Institutional Review Board and it was in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients before inclusion in this study.
We identified patients who underwent day-case surgery over the period from September 1th, 2018 to August 31th, 2019 in the “Day Surgery Unit” of our hospital (University of Campania “Luigi Vanvitelli” – Naples, Italy).
No prior sample size calculation was performed; however, all eligible patients were considered.
The inclusion criteria were as follows:
1. Day-case surgery procedures.
2. American Society of Anaesthesiology (ASA) ≤ 3.
3. 20 ≤ BMI ≤ 35.
4. Age of patient ≥ 18 years.
The exclusion criteria were as follows:
1. Severe cardiovascular diseases, including aortic insufficiency and thoracic aortic aneurysm.
2. External pacemakers.
3. Severe respiratory diseases.
4. Pregnancy.
5. Mental disability or other psychiatric disorder.
6. Incapacity to provide written informed consent.
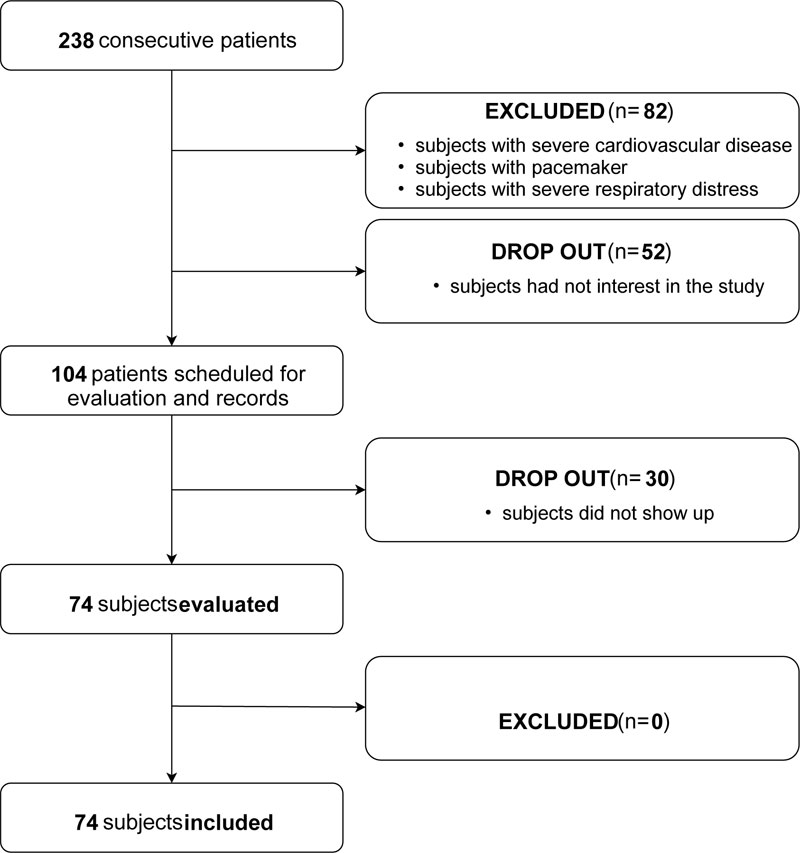
The flow chart (Fig. 1) shows in detail the procedure of patient selection. 238 patients were consecutively evaluated during the preoperative examination. In our practice, it is performed about 7 days before surgery. Eighty-two patients did not meet the required inclusion criteria. From the remaining 156 patients, 104 patients agreed to participate but thirty of them did not come to the scheduled appointment. Seventy-four patients were evaluated, and all of them were finally included in the present study.
According to the obesity criteria issued by a panel of experts from the World Health Organization, patients with a BMI < 25.0 kg/m2 were assigned to the non-obese group (NO group), and those with a BMI ≥ 25.0 kg/m2 were assigned to the obese group (O group).
We obtained demographic (age, sex, race) and clinical (height, weight, BMI, BSA) data. The BMI was calculated as weight in kilograms divided by the square of height in meters. The Body Surface Area (BSA) was calculated using DuBois and DuBois formula based on height and weight [15, 16].
All patients underwent standard blood exams including Arterial-Blood Gas (ABG) test, Chest X-ray (CXR), electrocardiogram (ECG) and spirometry.
All procedures were classified according to the type of anesthesia (spinal vs. locoregional anaesthesia). Patients were premedicated with intravenous 50 mg ranitidine and 2 mg midazolam. Subarachnoid block was obtained with the patient in the sitting position using a 25 G pencil point spinal needle at the L2–3 vertebral inter space. After aspirating cerebrospinal fluid, patients received 8 mg hyperbaric 0.5% bupivacaine. Local anaesthesia was performed injecting lidocaine and ropivacaine mixture into the surgical area intradermally and/or subcutaneously. Spinal anesthesia was administered by the resident doctor; in case of failure, the procedure was normally repeated by the attending doctor. Local anesthesia was generally administered by the surgeon.
NICOM® device was installed as soon as the patient arrived in the operating room, at the same time when the conventional vital sign monitoring equipment was applied. Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), mean arterial pressure (MAP) and heart rate (HR) were monitored using Draeger® Infinity Delta monitor. Cardiac Output (CO), Cardiac Index (CI), Stroke Volume Index (SVI) and Total Peripheral Resistance Index (TPRI) were monitored using NICOM®. Four non-invasive sensor pads were applied to the thorax as per device instructions-for-use and, after calibration, all haemodynamic data were recorded and analysed offline.
Data were continuously recorded during the perioperative period. For our analysis, we collected data: 1) before surgical treatment (T0); 2) after skin incision (T1); 3) 10 minutes after the beginning of surgery (T2); 4) after the end of surgery (T3).
2.1. Statistical Analyses
Patients are classified into six categories of BMI according to the National Institutes of Health guidelines: below normal (18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), obese class 1 (30–34.9 kg/m2), obese class 2 (35–39.9 kg/m2), and obese class 3 (≥ 40 kg/m2) [16]. In our study, patients were considered as non-obese with a BMI < 25 kg/m2; the remaining were considered overweight/obese with a BMI ≥ 25 kg/m2.
Data analyses were conducted using Statistical Analysis Software (SAS) and a standard computer program (Excel, 2016). Results were reported as mean ± Standard Deviation (SD). Statistical analyses were performed using Student t-test and repeated measures ANOVA. The level of statistical significance was p < 0.05.
This observational study is in accordance with the STROBE statement [17].
3. RESULTS
Seventy-four patients were included in the study. 34 were overweight or obese (weight 84 ± 10 kg, height 160 ± 10 cm, BMI ≈ 30 kg/m2), 40 were normal weight (weight 63 ± 15 kg, height 160 ± 10 cm, BMI ≈ 22 kg/m2). The age of the patients was 52.75 ± 10 years in the NO group, and 55.76 ± 10 years in the O group. The patients’ clinical and demographics characteristics are presented in Table 1. There were no significant demographic differences between the groups, except for weight, BSA and BMI. The distribution of patients based on BMI is shown in Fig. (2).
The surgical procedures performed in day surgery were: skin lesion removal (13.5%), breast-conserving surgery (lumpectomy) (15%), varicocelectomy (13.5%), phimosis surgical treatment (circumcision) (11%), trans urethral removal of bladder tumour (TURBT) (12%), carpal tunnel surgery (12%), inguinal hernia surgery (9.5%), and lipofilling in breast cancer patients (13.5%). All these procedures were performed in locoregional (76%) or spinal anaesthesia (24%). Table 2 shows the patients’ distribution in the various interventions and the types of anesthesia used.
| Surgical Procedures |
Size (n) |
Sex (M/F) |
Age (years) |
Weight (kg) |
Height (cm) |
BSA (m2) |
BMI (kg/m2) |
|---|---|---|---|---|---|---|---|
| NO Group | 40 | 12/28 | 52.75 | 62.75 | 164.8 | 1.69 | 22.84 |
| O Group | 34 | 24/10 | 55.76 | 84.05 | 165.5 | 2.06 | 30.5 |
| – | p = 0.8 | p = 0.69 | p < 0.05 | p = 0.91 | p < 0.05 | p < 0.05 |

| NO Group | O Group | Total | |
|---|---|---|---|
| Skin lesion removal | 6 (0) | 4 (0) | 10 (0) |
| Lumpectomy | 8 (0) | 3 (0) | 11(0) |
| Lipofilling | 6 (0) | 4 (0) | 10 (0) |
| Varicocelectomy | 4 (2) | 6 (4) | 10 (6) |
| Circumcision | 3 (0) | 5 (0) | 8 (0) |
| TURBT | 6 (4) | 3 (3) | 9 (7) |
| Carpal tunnel | 4 (0) | 5 (0) | 9 (0) |
| Inguinal hernia | 3 (2) | 4 (3) | 7 (5) |
| Total | 40 (8) | 34 (10) | 74 (18) |
In the control group, eight procedures (20%) were performed under spinal anaesthesia; in the obese group spinal anaesthesia was performed ten times (29.5%). Other procedures were carried out under locoregional anaesthesia. General anesthesia was not administered, being normally not provided at our institution in day-case surgery. No failure was reported in the administration of the anesthesia techniques; in the cases in which spinal anesthesia was used, five procedures (1 in the control group and 4 in the obese group) were performed on the second attempt by the attending doctor.
NICOM® electrodes were placed on the intended anatomic location in every case. In three cases, we observed displacement of the electrodes due to sweat, chest hair, or manipulation of the electrodes by a patient. In addition, a temporary signal loss occurred for unknown reasons in a case. Except for these incidents, the device recorded all parameters continuously.
We recorded a variation in SBP, DBP, MAP and CO during surgery in the obese group (p < 0.05). This data returned to baseline at the end of surgery.
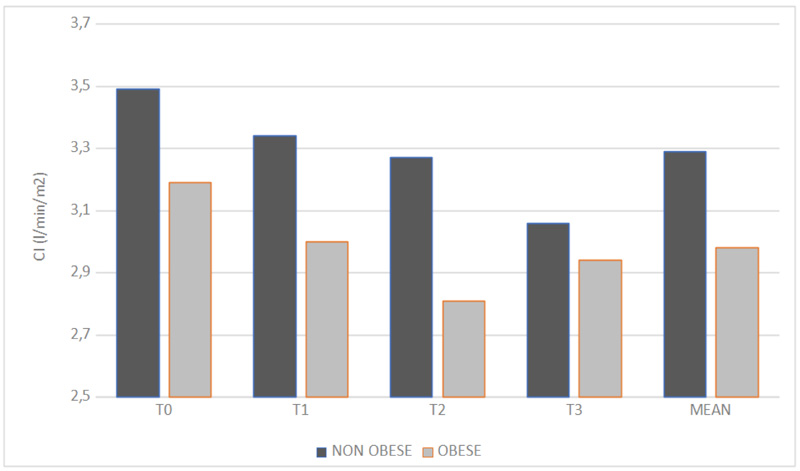
The CI measured by NICOM® in the NO group was 3.49 ± 0.81 l/min at T0, 3.34 ± 0.72 l/min at T1, 3.27 ± 0.77 l/min at T2, 3.06 ± 0.76 l/min at T4. In the O group was 3.19 ± 0.47 l/min at T0, 3.00 ± 0.84 l/min at T1, 2.81 ± 1.13 l/min at T2, 2.94 ± 0.82 l/min at T3. Data analysis shows a statistically significant change (p = 0.047) in CI over time during the operation (Fig. 3), (p < 0.05). This variation is greater in the O group than in the NO one, although this difference is not statistically significant (p = 0.24).
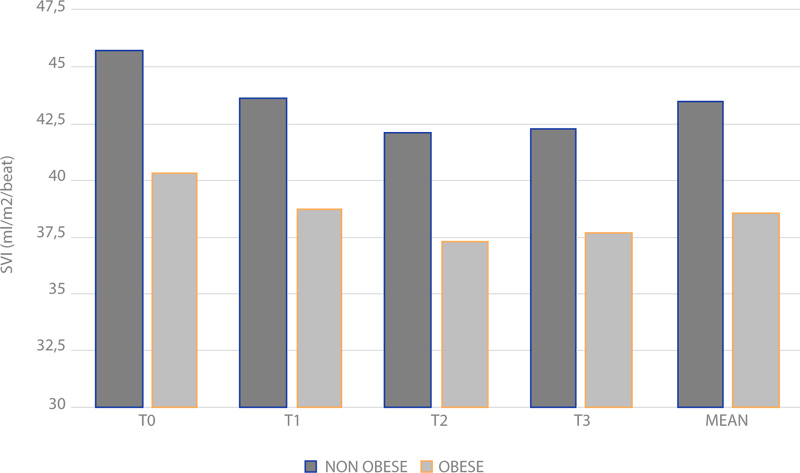
In the same way, the difference in the cumulative averages of SVI was 0.048 (Fig. 4), (p < 0.05). The SVI measured by NICOM® in normal weight group was 45.7 ± 9.8 ml/m2/beat at T0, 43.6 ± 11.8 ml/m2/beat at T1, 42.1 ± 9.6 ml/m2/beat at T2, 42.3 ± 12.1 ml/m2/beat at T3. In the obese group it was 40.3 ± 4.5 ml/m2/beat at T0, 38.8 ± 8.7 ml/m2/beat at T1, 37.4 ± 11.7 ml/m2/beat at T2, 37.7 ± 12.1 ml/m2/beat at T3.
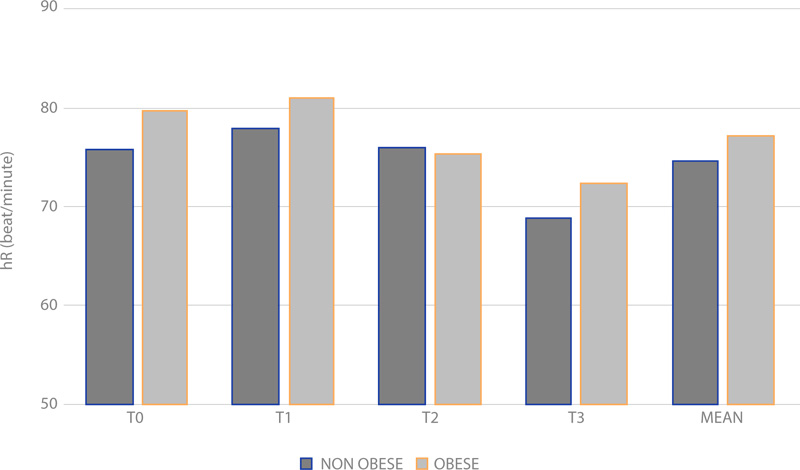
Otherwise, HR data do not show statistical significance (Fig. 5), (p > 0.05).
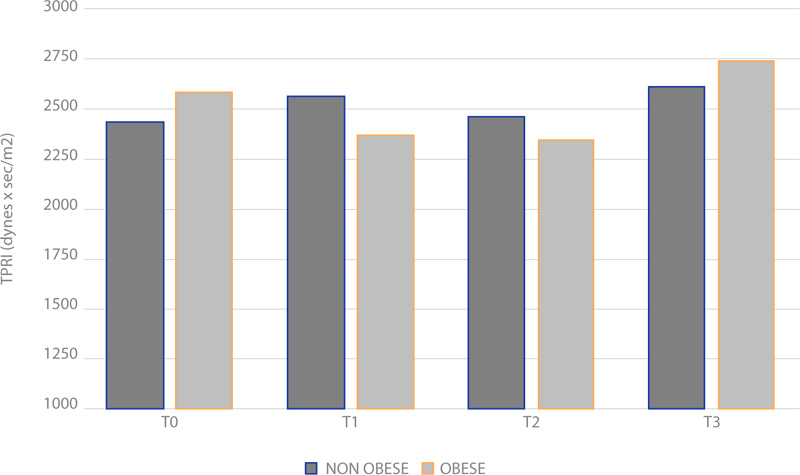
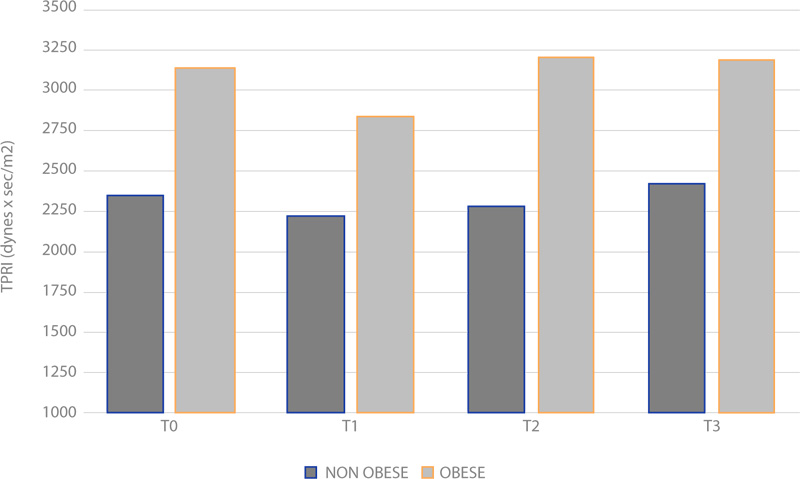
Concerning TPRI, the averages between the obese and normal weight groups do not show a significant change during operation under spinal anaesthesia (Fig. 6), (p > 0.05). Among the obese patients, TPRI is similar to the one in the NO group under spinal anesthesia. When local anesthesia was performed, we recorded an important difference in T0 (p = 0.0076), T1 (p = 0.0019) and T2 (p = 0.045); no significant difference was recorded in T3 (p = 0.10) (Fig. 7).
4. DISCUSSION
The goal of this observational study was to assess the impact of the BMI and anaesthesia technique during day-case surgery, as well as to evaluate the feasibility of using the non-invasive cardiac output monitoring NICOM® for the evaluation of haemodynamics in obese patients during these procedures.
Intraoperative haemodynamic perturbations are determined by the effects of anaesthetic agents and techniques, surgical manipulations, and the patient's medical comorbidities.
Furthermore, obesity produces a variety of haemodynamic alterations including elevated CO, low peripheral vascular resistance, and increased left ventricular end-diastolic pressure [18]. HR is normal or mildly elevated in obesity [18].
In our study, the obese show an increase in SBP, DBP and MAP with a return to baseline values at the end of surgery. These results are in accordance with those of preceding studies, which demonstrate that obesity is closely related to blood pressure [19].
CO shows a similar trend, whereas HR is normal. Indeed, the CO raise in obesity is due mainly to the augmentation of left ventricular stroke volume [18].
To attenuate the effects of BMI, we indexed haemodynamic measurements to BSA. A reduction in CI during operation was noticed in both groups, the one in obese patients being greater. In the same way, SVI was lower in the obese during surgery. Indexing haemodynamic data to BSA helps to remove any uncertainty regarding the interpretation of CO and SV at the extremes of body size [20].
We also evaluated the haemodynamic status after spinal and loco-regional anesthesia in the obese patients. In spinal anesthesia, TPRI was not statistically different between the groups of study. As for the TPRI in obese patients, we reported values similar to non-obese patients in spinal anesthesia. In local anesthesia, TPRI was higher in obese patients than in non-obese ones.
Spinal anesthesia induces sympathetic blockade with subsequent reduction in myocardial contractility, heart rate, and change in cardiac loading conditions [21]. It leads to a decrease in venous return due to increased compliance of the venous system, vasodilatation and, finally, decreased blood pressure [21]. Concerning local anesthesia, it may cause stress leading to blood pressure change, haemodynamic and cardiovascular reactions [23]. Pain causes an alarm reaction with an increase in systemic arterial pressure and pulse rate due to the release of endogenous catecholamine [22].
NICOM® was easy to use: installation, operation, and monitoring could be performed by one person. Problems with the device were the detachment of the electrodes and the temporary loss of the signal due to the displacement of the electrode or unknown reasons. This device did not affect the standard of care in the operating room, including anesthesia and all surgery procedures.
NICOM® is deployable in a wide variety of clinical settings, and has demonstrated clinical utility with diverse patient populations, and for a wide range of clinical conditions. Common clinical sites for non-invasive cardiac monitoring are the operating room and the Critical Care, such as the Intensive Care Unit (ICU) and the Emergency Department (ED).
Critical care patient populations are often haemodynamically unstable and only 50% of these patients respond to fluid administration by increasing CO and perfusion. NICOM® provides the ability to rapidly and noninvasively test fluid responsiveness, allowing critical care clinicians to make more informed decisions, guiding effective fluids, vasopressors and inotropes administration [24-26].
According to Enhanced Recovery after Surgery (ERAS), an accurately administration of fluids and vasoactive agents throughout the entire perioperative period has been shown to improve patient outcome [27]. ERAS protocols have resulted in a length of hospital stay 30% to 50% shorter and similar reductions in complications, while readmissions and costs are reduced. This is particularly important in day-case surgery, where patients are admitted to hospital, have the operation or treatment and go home the same day. Until recently, haemodynamic evaluation required invasive monitoring, which was unsuitable in awake patients for day-case surgery. NICOM® provides a continuous, non-invasive haemodynamic measurement. This device does not bring inconvenience to patients making it clinically suitable for monitoring awake patients having loco-regional anesthesia.
4.1. Limitations
The study has some potential limitations. Although, as far as we know, our study was the first evaluating non-invasive cardiac monitoring in day-case surgery, it would have been stronger if it had been conducted as a randomized prospective clinical trial with a larger sample size.
Another possible limitation is that there was no formal sample size calculation performed and enrolment was based on the feasibility of performing an exploratory analysis. Overall, the sample size was also small. Despite some compelling findings, it is possible that the study is underpowered. If so, the results may be exaggerated and there is a higher likelihood that the effect found may not represent a true effect.
Finally, multiple types of surgeries and different types of anesthesia were included in our analysis. However, this study was designed to provide first insights into the use of non-invasive cardiac monitoring in day-case surgery in settings and procedures that have not been evaluated routinely in controlled clinical trials.
However, taking into account the results of this study, non-invasive cardiac monitoring in obese patients in day-case surgery seems to be a promising technique and should be investigated in a larger clinical study.
CONCLUSION
Obesity produces a variety of haemodynamic alterations with greater risk of morbidity and perioperative mortality. Cardiovascular alterations related to obesity include an increase in blood pressure, CO and SV. Among the risk factors for perioperative complications there is the inadequate and insufficient monitoring of haemodynamic parameters. Especially in day-case surgery invasive monitoring is difficult to apply. NICOM® is often presented as a monitoring system that is easy to use, non-invasive, able to better evaluate and guide the correct anaesthetic plan for this type of patients. Further research is needed to confirm the clinical value of NICOM® monitoring and how this technology might help to further reduce postoperative morbidity and mortality in obese patients scheduled for day-case surgery.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee of the University of Campania "Luigi Vanvitelli", Italy, with the approval no. 0003208/2016.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all patients before inclusion in this study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICTS OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


