All published articles of this journal are available on ScienceDirect.
The Mixture of Topical Anesthetic and Chlorhexidine at the Delivery Site in Microbial Reduction Efficiency
Abstract
Background:
Antimicrobial properties of some anesthetic agents have been reported which may be useful for infection control. Topical lidociane (10%) showed some extent of antimicrobial activity on oral microflora.
Objective:
This study aimed to determine whether the antimicrobial efficiency of topical lidocaine can be enhanced by adding chlorhexidine.
Methods:
The Lidocaine-Chlorhexidine (LD-CHX) preparation was prepared by mixing 2.0% CHX and 10% LD with various ratios. The anesthetic efficiency was tested on the oral mucosa of 26 volunteers by Pin Prick Test. Pain scores were recorded using the Numerical Rating Scale (NRS). Antimicrobial effects of 10% LD, 0.2% CHX, and LD-CHX preparations were evaluated. In vitro study was conducted against seven standard bacterial strains. For in vivo study, oral biofilms of 26 volunteers were collected by imprint technique using filter papers. Bacterial growth from the samples after applying the test solutions was compared to the control. Antimicrobial efficiency was expressed as microbial reduction scores from 4-0 (highest to lowest).
Results:
The LD-CHX preparations that had comparable anesthetic efficiency to 10% LD were those containing 9% and 8% LD. These LD-CHX preparations showed microbial reduction scores of 3 and 4 on seven bacterial strains and oral biofilms.
Conclusion:
This study showed the antimicrobial and anesthetic effectiveness of new lidocaine-chlorhexidine preparations both in vitro and in vivo. We also confirmed the effectiveness of infection control protocol in oral surgery using CHX mouthwash prior to topical LD.
1. INTRODUCTION
Dental treatments usually cause pain to patients so local anesthetic injections are given to relieve pain, especially in oral and maxillofacial surgery. The injection itself causes some degree of pain, therefore topical anesthetics are usually applied on the local anesthetic delivery site prior to the local anesthetic injection. The topical anesthetic is only effective in blocking the pain stimuli in the superficial layer of the mucosa or skin by temporarily anesthetizing the tiny nerve ending close to the target mucosa or skin surface. The widely used local anesthetics in anesthesia is Lidocaine (LD) hydrochloride, an amide-based anesthetic which has a rapid onset, moderate duration of action, and less complications [1, 2]. LD is available in both injectable and topical forms in various concentrations. For injections, a 2% concentration of lidocaine is commonly used with various vasoconstrictors, such as epinephrine. For topical anesthetics, a higher concentration is used and available in various forms of spray, gel, and ointment.
Besides pain blocking, several local anesthetic agents including lidocaine have been known to possess antimicrobial effects against various bacterial species and candida [3, 4]. The in vitro antimicrobial effectiveness depends on the type and concentration of drugs, tested microorganisms, and methods of antimicrobial susceptibility testing. However, the beneficial role of the antimicrobial activity in clinical use has not yet been confirmed. In patients, topical anesthetics are used to reduce pain before collecting a sample at the sensitive infected area, such as wound area, the cornea, or the upper respiratory tract. This procedure may cause false-negative results of pathogen detection from the specimen for diagnostic purposes [5-8]. During dental treatment, some local anesthetic injection techniques, such as buccal infiltration, conventional and modified intra-ligamental injection, have shown significant increases in bacteremia [9]. Bacterial levels in the bloodstream have been shown to increase immediately after local anesthetic injection occurs and decreased within 1 hour to normal levels [10]. The application of topical anesthetics to reduce pain from local anesthetic injections might, therefore, help decrease bacteremia caused by oral microflora due to the drug injection. In addition, the incidence of local infections or abscesses at the site of injection is very low.
In clinical settings, the use of antiseptic mouthwash is recommended to reduce oral microflora before some dental treatments with a high risk of bacteremia. Prophylaxis antibiotics are recommended in some circumstances prior to tooth extraction, dental cleaning, dental implant surgery and dentoalveolar surgery to reduce postoperative infections [11-14]. Among the several antiseptic agents available, Chlorhexidine (CHX) mouthwash is the gold standard for infection control due to its efficiency and wide range of antimicrobial spectrum [15]. However, using antiseptic mouthwash may not be appropriate for those allergic to the agents. In some patients, having severe oral lesions, mucositis due to HIV infection or an immunodeficiency state, or complications from radiotherapy, require agents to reduce pain and prevent infection.
In general, local anesthetics are recommended to relieve pain and chlorhexidine is used to prevent infection [16, 17]. Our previous study has shown that topical anesthetics spray containing 10% lidocaine inhibited the growth of some oral microflora in vitro and showed 60-95% biofilm reduction on buccal mucosa [18]. It suggests a prophylaxis use of lidocaine in the clinical setting. However, the antimicrobial efficiency of the 10% lidocaine spray is less than 0.2% chlorhexidine. Therefore, the purpose of this study was to determine whether the antimicrobial efficiency of topical lidocaine can be enhanced by adding chlorhexidine. The antimicrobial effectiveness against some oral microflora, oral biofilms and the anesthetic property of various lidocaine-chlorhexidine preparations will be evaluated.
2. MATERIALS AND METHODS
This study was performed at the Faculty of Anesthesia, Mahidol University, Bangkok, Thailand. The study protocol was approved by the Institutional Review Board, Faculty of Anesthesia and Faculty of Pharmacy, Mahidol University (No.MU-DT/PY-IRB 2018/044.2708). With the ORCID iD of every author, the volunteers gave informed consent before conducting the experiments.
2.1. Reagents
Xylocaine® (10% w/v Lidocaine) was purchased from AstraZeneca, UK. Chlorhexidine, 0.2% v/v was prepared from a 2% v/v chlorhexidine solution (M Dent®) using sterile phosphate-buffered saline. Brain Heart Infusion (BHI) agar, BHI broth, and Blood agar for bacterial cultivation were purchased from Difco™, France. Lidocaine-Chlorhexidine (LD-CHX) preparation was prepared by mixing 10% Lidocaine and 2% Chlorhexidine with various ratios under a sterile procedure and used within 2 hours after mixing. Three LD-CHX preparations were shown in (Table 1).
| Lidocaine-Chlorhexidine Preparation | Concentration | |
|---|---|---|
| Lidocaine (%w/v) |
Chlorhexidine (%v/v) |
|
| Preparation I | 9 | 0.2 |
| Preparation II | 8 | 0.4 |
| Preparation III | 7 | 0.6 |
2.2. Subjects
Twenty-six volunteers were recruited from students and staff of the Faculty of Anesthesia at Mahidol University. Table 2 shows the eligible criteria of inclusion and exclusion in this study. All volunteers have an American Society of Anesthesiologists (ASA) physical status I or II [19]. Subjects’ past medical history and dental history were recorded along with current dental status and oral hygiene status. The experiments were done at least 1 hour after meals or brushing teeth.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| 1. The volunteers were healthy with ages above 18 years. | 1. The volunteer had oral lesions on the buccal mucosa. |
| 2. The volunteers had the same number of teeth on the left and right side of their mouth. | 2. The volunteer had poor blood circulation, |
| 3. The volunteers had ASA physical status of I or II. | 3. The volunteer had allergies to chlorhexidine or lidocaine. |
| 4. The volunteers had the intact oral mucosal membrane. | 4. The volunteer use antimicrobial mouthwash prior to the experiment. |
| 5. The volunteer received antibiotics within 2 weeks prior to the study. |
2.3. Experimental Designs
2.3.1. Anesthetic Efficiency of the LD-CHX Preparations in vivo
Anesthetic efficiency of 10% lidocaine and the LD-CHX preparations was tested in twenty-six volunteers. The designated test area for local anesthetic delivery was at the palatal mucosa, which is approximately 5 mm away from the gingival margin of the first molar. The area was dried using sterile gauze, then a 2 x 2 mm filter paper impregnated with the test solution was applied on the mucosal surface for 2 min. The pinprick test was conducted by pressing an explorer tip to the mucosa gently three times. Pain perception was assessed by the Numerical Rating Scale (NRS) where the subjects were asked to rate their pain from 0 (no pain) to 10 (worst possible pain). At the end of all sessions, the volunteers were asked whether they recognized the difference in pain perception between the 10% lidocaine and the LD-CHX preparations.
2.3.2. Antimicrobial Activity of the Lidocaine, Chlorhexidine and the LD-CHX Preparations Against Oral Bacteria in vitro
Seven bacterial strains were used in this study, including 1) Escherichia coli ATCC 25922, 2) Enterococcus faecalis ATCC 9433, 3) Staphylococcus aureus ATCC 6538, 4) Streptococcus salivarius ATCC 19258, 5) Streptococcus pyogenes ATCC 19615, 6) Streptococcus sanguinis ATCC 10556, and 7) Pseudomonas aeruginosa ATCC 27853. The bacterial strains were cultured in BHI broth, and then adjusted to the turbidity of the 0.5 McFarland standard. The bacterial suspensions were diluted to obtain approximately 1.0 x 105 CFU/ml. A 100-μl of bacterial suspension was inoculated on the entire surface of a blood agar plate using a sterile swab.
The plate was divided into 4 quadrants where each was placed with a filter paper containing the test solution. The test filter papers (Whatman® Qualitative Filter Papers, Grade 1)-1.5 x1.5 cm- were impregnated with 40-μl of sterile Phosphate-Buffered Saline (PBS), 10% lidocaine, 0.2% chlorhexidine, or the LD-CHX preparation. Then each test filter paper was placed on a quadrant of the blood agar surface for 2 min. The filter papers were removed, and the plates were further incubated at 37 ºC in a CO2 incubator for 24 h.
The growth of bacteria in each quadrant was observed. The quadrant exposed to PBS was served as negative control which showed the confluent growth of the bacteria. The bacterial growth on other quadrants was compared to the control, and microbial reduction scores were recorded as shown in (Table 3). Each bacterial strain was tested at least twice to ensure the results.
| Growth Compared to the Negative Control | Antimicrobial Scores |
|---|---|
| No growth or > 95% bacterial reduction | 4 |
| Growth density was 60–95% bacterial reduction | 3 |
| Growth density was 40–60% bacterial reduction | 2 |
| Growth density was 5–40% bacterial reduction | 1 |
| Growth density comparable to the negative control or less than 5% bacterial reduction | 0 |
2.3.3. Effect of the LD-CHX Preparations on Oral Biofilm Reduction
The effects of the LD-CHX preparations on oral biofilm reduction were evaluated in 26 volunteers. Sterile filter papers were used to collect oral biofilm samples from the buccal mucosa of the volunteers. The filter papers, size 2 x 2 cm, containing phosphate-buffered saline (PBS, pH 7.0) served as the negative control. The filter paper was placed on one side of the buccal mucosa above the occlusal plane for 1 min, and transferred onto one half of a blood agar surface for 1 min.
Four sets of experiments were carried out one week apart. In the first experiment, the subjects were asked to use 0.12% chlorhexidine mouth rinse for 30 seconds. Then, the filter paper (2 x 2 cm) containing 100 µl of 10% lidocaine was placed on the other side of the buccal mucosa for 2 minutes and replaced with the 1.5 x 1.5 cm filter papers containing PBS to collect any remaining microflora in the area. After 1 min, the filter paper was placed on another half of a blood agar surface for 1 min. The plate was incubated in a CO2 incubator for 24 hr. The growth of bacteria on the lidocaine side was compared with the negative control showing confluent oral biofilm growth and recorded as the microbial reduction score.
In the second experiment, the filter papers (2x2 cm) containing 10% lidocaine were placed on the other side of the buccal mucosa for 2 min, and replaced with the 1.5 x 1.5 cm filter papers containing PBS for 1 min. The filter paper was then placed on the other half of the blood agar surface for 1 min. The growth of bacteria was determined as previously mentioned. The third and fourth experiments were conducted in a similar manner using 0.2% chlorhexidine and the LD-CHX preparations.
3. RESULTS
3.1. Anesthetic Efficiency of the LD-CHX Preparation in vivo
We initially assessed the anesthetic efficiency of the LD-CHX preparations I, II, III containing 9%, 8% and 7% lidocaine, respectively, compared to 10% lidocaine. After applying 10% topical lidocaine, 11 of 26 subjects showed no pain (NRS = 0) while 9 subjects reported NRS of 1 and 6 subjects reported NRS of 2. When the LD-CHX preparation I (9% lidocaine) and II (8% lidocaine) were tested, similar results to 10% lidocaine were obtained. Each subject reported the same NRS scores. As the concentration of lidocaine was reduced to 7% in the LD-CHX preparation III, the anesthetic efficiency was also reduced. As shown in Table 4, only 6 subjects showed no pain and the NRS scores of 3 were reported in 8 subjects.
| NRS Scores | Lidocaine (10%) | Lidocaine - Chlorhexidine Preparations | ||
|---|---|---|---|---|
| LD-CHX I (lidocaine 9%) | LD-CHX II (lidocaine 8%) | LD-CHX III (lidocaine 7%) | ||
| 0 | 42.3 (11) | 42.3 (11) | 42.3 (11) | 23.1 (6) |
| 1 | 34.6 (9) | 34.6 (9) | 34.6 (9) | 23.1 (6) |
| 2 | 23.1 (6) | 23.1 (6) | 23.1 (6) | 23.1 (6) |
| 3 | 0 | 0 | 0 | 30.7 (8) |
3.2. Antimicrobial Activity of the Lidocaine, Chlorhexidine and the LD-CHX Preparations Against Oral Bacteria in vitro
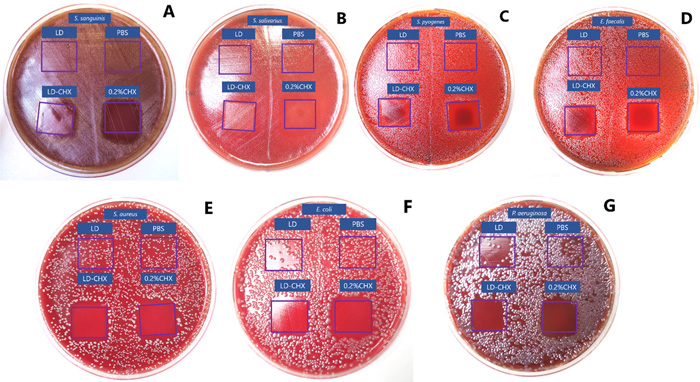
The antimicrobial effects of 10% lidocaine, 0.2% chlorhexidine, and the LD-CHX preparations were tested against seven bacterial strains. The in vitro results showed that 10% lidocaine had no antimicrobial effects against S. sanguisnis, S. salivarius, S. pyogenes, E. faecalis, S. aureus, and some partial inhibition to E. coli and P. aeruginosa. Chlorhexidine 0.2% and all LD-CHX preparations showed a microbial reduction score of 4 to all tested bacterial strains as presented in Fig. (1).
3.3. Effect of the LD-CHX Preparations on Oral Biofilm Reduction
Imprinted techniques were used to collect oral biofilms from the applied site using filter papers and then cultured to determine the microbial growth. Representative results of oral biofilm reduction from the subject using 0.12% chlorhexidine mouthwash followed by 10% lidocaine, 10% lidocaine, 0.2% chlorhexidine, LD-CHX preparations, compared to the negative control, Phosphate Buffered Saline (PBS) were showed in Fig. (2).
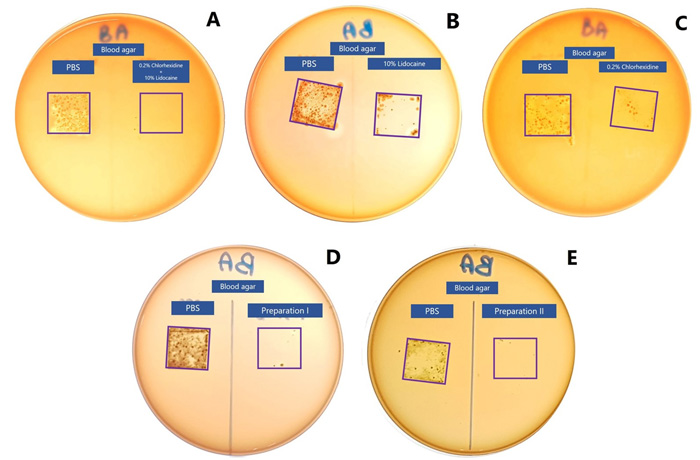
Results from all subjects using the chlorhexidine mouthwash followed by 10% lidocaine exhibited an antimicrobial reduction score of 4. Microbial reduction after using 10% lidocaine, 0.2% chlorhexidine, and the LD-CHX preparation I and II are summarized in Table 5. Lidocaine 10% had the least antimicrobial effect. Only 2 out of 9 subjects showed an antimicrobial score of 4. The remaining subjects had an antimicrobial score of 3. Chlorhexidine 0.2% and the LD-CHX preparation I (lidocaine 0.9% and chlorhexidine 0.2%) exhibited the same results.
The number of subjects showing an antimicrobial score of 4 increases to 6 out of 9. For the LD-CHX preparation II (lidocaine 0.8% and chlorhexidine 0.4%), the number of subjects showing an antimicrobial score of 4 was 12 out of 26 and the remaining subjects showed an antimicrobial score of 3. This indicates the effectiveness of LD-CHX preparations in the antimicrobial reduction potential.
| Antimicrobial Score | Test Solutions | |||
|---|---|---|---|---|
| Lidocaine (10%) |
Chlorhexidine (0.2%) |
LD-CHX-I (lidocaine 9%) | LD-CHX-II (lidocaine 8%) | |
| 4 | 22.2 (6) | 66.7 (18) | 66.7 (18) | 46.2 (12) |
| 3 | 77.8 (20) | 33.3 (8) | 33.3 (8) | 53.8 (14) |
4. DISCUSSION
Due to the fact that oral mucosa is commonly colonized with mixed-species biofilms, antimicrobial property of topical anesthetics suggests a beneficial supplemented role in clinical settings for infection control. Our previous study showed the antimicrobial effectiveness of topical lidocaine spray against oral biofilms. However, the antimicrobial efficiency of 10% lidocaine on oral biofilms was lesser than 0.2% chlorhexidine [18]. In this study, we aimed to enhance the antimicrobial effect of lidocaine by adding chlorhexidine, and determine whether the preparations containing various concentrations of lidocaine and chlorhexidine exhibit effective anesthetic and antimicrobial effects. We simply prepared the Lidociane-Chlorhexidine preparations by mixing 10% topical lidocaine with 2% chlorhexidine in various ratios. The LD-CHX preparations were then assessed by anesthetic and antimicrobial efficiency.
Initially, pain perception was determined in a group of volunteers. At the ratio of lidocaine and chlorhexidine 7:3, which contains 7% lidocaine and 0.6% chlorhexidine, anesthetic efficiency was reduced to approximately 65% of subjects. The higher concentration of lidocaine at 8% and 9%, anesthetic efficiency was comparable to 10% lidocaine. Therefore, these two LD-CHX preparations were further assessed for antimicrobial activities.
The antimicrobial activities were evaluated against the standard strains of 7 bacterial species. These bacteria included oral streptococci- S. sanguinis and S. salivarius, pathogenic gram-positive cocci- S. pyogenes, E. faecalis, and S. aureus, pathogenic gram-negative bacilli- E. coli and P. aeruginosa. The results showed that LD-CHX preparations had comparable antimicrobial effectiveness comparable to 0.2% chlorhexidine (antimicrobial score of 4). It is not unexpected since the LD-CHX preparation I and II contained chlorhexidine 0.2% and 0.4%, respectively. No antagonist effect on antimicrobial activity was observed.
Since the LD-CHX preparations were aimed to be used clinically as both antiseptics and
anesthetics, it is necessary to assess the effectiveness of antimicrobial and anesthetic activity in vivo. To assess antimicrobial effectiveness, biofilm bacteria on the buccal mucosa were collected after applying the LD-CHX preparation for 2 min using the imprint technique. The imprint technique using filter papers to collect biofilms from oral mucosa is fast, non-invasive, and can be compared within each subject. It is convenient for the researchers and enables quantitative comparison regarding the growth of bacteria by using the same area of sample collection sites. Regarding the antimicrobial effectiveness of the LD-CHX preparations, a significant reduction of the oral bacterial flora on the buccal mucosa was observed (antimicrobial score of 3 and 4).
Additionally, we conducted the clinical experiment to mimic the conventional protocols used in oral surgery in which the 0.12% chlorhexidine mouthwash is used prior to the application of 10% topical lidocaine. No bacteria were found at the applied site of topical lidocaine. It suggests that the prior use of chlorhexidine mouthwash to reduce oral bacteria may enhance the antimicrobial effectiveness of a subsequent application of lidocaine. The LD-CHX preparations might not be as effective in clinics as the conventional method (using chlorhexidine mouthwash prior to topical lidocaine). This might be due to the different procedures as mouth rinse may have better mechanical removal of biofilms than the application method. In addition, bacteria from saliva were reduced after mouth rinse and caused less contamination on the mucosa when applying lidocaine. For intraoral application, the mucosa at the target area should be dried prior to an anesthetic
administration. The topical anesthetic is then applied to the surface area by spraying or using a cotton swab. To get the significant anesthetic effect, it requires at least 2 minutes application before the injection of the local anesthesia. There were discrepancies in the results when antimicrobial effectiveness of the LD-CHX preparations was conducted in a clinical situation. This might be due to the variable of oral biofilms in each individual, which differed in microbial species and concentration, and biofilm thickness. Other factors that may interfere with the effectiveness are the contact time, or the diluting effects by saliva. We are aware that the concentrations of chlorhexidine in the LD-CHX preparations (0.2% and 0.4%) were higher than chlorhexidine mouthwash (0.12%). Due to the small amount and short duration of application, the toxicity should be less concerned. Nevertheless, the preparation of lidocaine mixing with chlorhexidine may be an alternative useful option for particular patients who require dual effects.
It has been proposed that local anesthetics can eliminate the local pain by blocking the Na+ channel within the neuronal membrane during their activated and inactivated state [20]. This mechanism of action also explains the mechanism of antimicrobial property of local anesthetics. The electrostatic binding of anesthetic molecules to the cell membrane leads to disruption of the bacterial cell wall or cytoplasmic membrane [21, 22]. Consequently, membrane solubility and permeability are changed, causing K+ leakage from bacterial cytoplasm. The anesthetic molecules also inhibit membrane respiratory activity [23]. Antifungal mechanisms might be presented in the same way, germ tube formation inhibition and K+ leakages are caused by changing of cell membrane permeability [24, 25]. In addition, some studies reported the effect of lidocaine on DNA, RNA and protein synthesis [26].
Taken together, results from this study suggest that it might be possible to use the preparation of LD-CHX for infection and pain control. Enhancing the antimicrobial effect on anesthetic agents makes it more practical to use in clinical settings. Lidocaine topical anesthetic and chlorhexidine are available in most dental clinics and hospitals in the liquid preparation. It may reduce cost, time, and more convenience for a dentist to prepare the solution. It will benefit patients who need both an antiseptic agent and pain-relief on the local site.
CONCLUSION
This study showed the antimicrobial and anesthetic effects of the lidocaine-chlorhexidine mixtures both in vitro and in vivo. The LD-CHX preparations that had comparable anesthetic efficiency to 10% LD were those containing 9% and 8% LD. These LD-CHX preparations showed a 60-95% bacterial reduction on tested bacterial strains and oral biofilms. In addition, using CHX mouthwash prior to topical LD was effective to be used as an infection control protocol in oral surgery.
LIST OF ABBREVIATIONS
| ASA | = American Society of Anesthesiologists |
| ATCC | = American Type Culture Collection |
| BHI | = Brain Heart Infusion |
| CHX | = Chlorhexidine |
| CFU | = Colony Forming Unit |
| DNA | = Deoxyribonucleic Acid |
| HIV | = Human Immunodeficiency Viruses |
| LD | = Lidocaine |
| NRS | = Numerical Rating Scale |
| PBS | = Phosphate-Buffered Saline |
| RNA | = Ribonucleic Acid |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol was approved by the Institutional Review Board, Faculty of Anesthesia and Faculty of Pharmacy, Mahidol University (No.MU-DT/PY-IRB 2018/044.2708) Bangkok, Thailand.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
This study was done after approval of the local ethics committee and obtaining written informed consent from the enrolled participant.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this research are available from the corresponding author upon a reasonable request.
FUNDING
None
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors would like to thank the staff and dental assistants in Department of Oral and Maxillofacial Surgery and Mr. Arthit Kloa-Phimai, a Scientist, Department of Oral Microbiology, Faculty of Anesthesia, Mahidol University.


