RESEARCH ARTICLE
Repeated Epidural Anesthesia and Incidence of Unilateral Epidural Block
Ramy Mahrose*, Mohamed M. Kamal
Article Information
Identifiers and Pagination:
Year: 2019Volume: 13
First Page: 6
Last Page: 11
Publisher ID: TOATJ-13-6
DOI: 10.2174/2589645801913010006
Article History:
Received Date: 15/01/2019Revision Received Date: 20/03/2019
Acceptance Date: 30/03/2019
Electronic publication date: 30/04/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Epidural block is today the most common method of pain relief during labor. Nowadays, facing a multiparus parturient requiring epidural for the second or third time is common due to increased frequency of using epidural analgesia during labor.
Objectives:
Examination of the performance and outcome of women receiving their first versus repeated epidural block.
Methods:
The study included 140 American Society of Anesthesiologists (ASA) Physical Status II parturients (age range 20 to 40 years) and scheduled for normal vaginal delivery. The parturients were divided randomly into two equal groups. Group (A) in which 70 women primipara subjected to their first epidural block, while group (B) in which 70 women multipara subjected to their repeated epidural block. Our primary outcome of the study is the incidence of a unilateral block and secondary outcomes include Visual Analogue Scale (VAS) before the epidural and 30 minutes after injection of local anesthetic and details of labor as gestation and cervical dilatation.
Results:
The results showed that there was a statistically significant decrease in the incidence of a unilateral block in the group (A) when compared to the corresponding values in the group (B) (P-value < 0.05). Moreover, group (A) showed a statistically significant decrease in Visual Analogue Scale (VAS) values 30 minutes after the injection of local anesthetic (P-value < 0.05).
Conclusion:
The conclusion of our study is that there is a higher incidence of unilateral block amongst women receiving their repeated epidurals for labour than those receiving their first epidural block.
1. INTRODUCTION
Epidural analgesia is now the commonest method to provide pain relief during labor in many institutions. The use of epidural analgesia has become so widespread in recent years that many women are now requesting to repeat epidural analgesia for their second or subsequent labor [1].
Repeated epidural block due to repeated delivery or any other operation during which epidural block was used may be associated with the formation of adhesions and fibrous septa in the epidural space which causes misdistribution of the local anesthetic in the epidural space and plays a major role in the occurrence of unilateral epidural block and failure to control labor pain [2].
The reported incidence of the unilateral epidural block in obstetric patients varies from 5-21%. This complication is annoying for both the patient and the anesthesiologist and may require a redo of the epidural block with subsequent psychological and financial burdens [3].
The effect of previous epidural injection on performance and outcome of subsequent epidurals has not received much attention. It was our impression that there was a higher incidence of unilateral blockade among women receiving their second epidural.
The purpose of the study is to examine performance and outcome in women receiving their first versus repeated epidural.
2. PATIENTS AND METHODS
2.1. Selection of Patients and Randomization
This study was performed after obtaining approval from the ethics committee of the Ain Shams University. A sample of 140 healthy ASA II female Parturients, 20-40 years of age, is scheduled for normal vaginal delivery. Parturients were randomly allocated by computer-generated random number list into two study groups of 70 patients each.
Group (A) in which 70 primipara women subjected to their first epidural block while group (B) in which 70 multipara women subjected to their repeated epidural block. The study was carried out between January 2018 and March 2018.
Patients were excluded for any physical reason for difficult epidural performance e.g.: morbid obesity, scoliosis, severe hypertension, congestive heart failure, coagulopathy, significant hepatic or renal disease or withdrawal of consent.
All patients in this study were subjected to a detailed pre-anesthetic evaluation. All basic investigations according to the hospital protocol (e.g. serum hemoglobin, platelet count, coagulation profile) were checked.
The patient's demographic data, details of labor (gestation, cervical dilatation) and details of epidural insertion were recorded by the anesthetist performing the epidural.
The patient was asked to mark a Visual Analogue Scale (VAS) (Table 1) before the epidural and 30 minutes after injection of local anesthetic. Also, the incidence of the unilateral epidural block is reported 30 minutes after injection of local anesthetic.
2.2. Anesthetic Technique
On arrival to operation room, 18 g cannula was inserted then 500 ml of Ringer solution was infused while performing the epidural.
Basic monitors including automatic blood pressure measurements, five-lead ECG monitor, and finger pulse oximetry were applied to all patients.
A standard procedure was followed for epidural insertion and establishment of the block. With the patient in the sitting position, the midline approach was used using 16-g Tuohy needle and the epidural space was identified by the loss of resistance to air, as is our routine practice.
Once the epidural space was reached, Bupivacaine 0.25% plain, was given in three 5 ml increments at five-minute intervals, the first administered through the needle while the patient is in sitting position, and then through the catheter with the patient in supine position.
Multi-orifice catheters were inserted and fixed to a standard 4 cm extra to the distance between the skin and epidural space. At the time of insertion of the catheter, the patient was asked to report any pain or tingling experienced [5].
The operator recorded the ease of insertion of the catheter (difficult or easy) and the occurrence of blood in a needle or catheter. Epidurals were performed by the same anesthetists.
At 30 min after the injection of bupivacaine, the second VAS was completed and the level of blockade checked by cold sensation test. If an inadequate level was noted (less than T10), the pain score remained high or increased, or if the patient complained of poor pain relief, she was asked to describe the site and type of pain experienced.
A unilateral block was defined as the description by the patient of worse pain on one side than the other, or pain on one side only, combined with either a 30-min pain score minimally changed or increased from time zero or a low level of the blockade on the painful side, or both [6]. If unilateral or inadequate block occurred, the catheter was withdrawn 0.5-1 cm and a further 5 mL bupivacaine 0.25% was administered with the patient lying on the unblocked side. If the block was still inadequate, epidural fentanyl 50 micrograms (diluted in 5 mL of normal saline) was given in the lateral position.
The number of repeated injections of bupivacaine and length of time between epidural insertion and delivery was noted.
2.3. Sample Size Estimation
The incidence of unilateral block among groups was the primary outcome of the study and was compared using Chi-square test, to achieve a power of 0.8 and alpha error of 0.05, a minimum sample size of 70 patients was calculated for each group.
2.4. Statistical Analysis
Analysis of data was done by IBM computer using SPSS (statistical program for social science, version 16). The quantitative variables were described as mean and standard deviation, while the qualitative variables expressed as number and percentage.
Statistical analysis was performed using statistical tests which included Student’s t-test, Chi-square test and table analysis. P-value < 0.05 is considered significant.
3. RESULTS
One hundred and forty women were studied, 70 were primipara had received their first epidural and 70 had received epidural analgesia or anesthesia during a previous pregnancy. The two groups were comparable with respect to weight and height (Table 1). The multiparas were, predictably, older than the primipara and had greater cervical dilatation at epidural insertion. The time between epidural insertion and delivery was also shorter in the multipara. There were 22 caesarean sections in the primipara compared with two in the multipara. The number of repeated injections of bupivacaine till delivery showed no significant difference between the two groups (Table 2).
There is no statistical difference between the two groups as regards visual analogue scale assessment before the epidural block but there was a significant reduction of the VAS in both groups after the block indicating more relief of labor pain after the epidural block (Table 2 and Fig. 1).
| Parameters |
Group A
(n = 70) Mean ± SD |
Group B
(n = 70) Mean ± SD |
P- value |
|---|---|---|---|
| Age (years) | 26.6 ± 7.1 | 27.4 ± 7.4 | P = 0.515 |
| Weight (kg) | 74.4 ± 11.0 | 71.8 ± 18.8 | P = 0.304 |
| Height (cm) | 163.8 ± 5.8 | 164.5 ± 2.3 | P = 0.349 |
| Gestational age (wks.) | 38.9 ± 5.8 | 37.3 ± 9.3 | P = 0.224 |
| Cervical' dilatation (cm) | 3.2 ± 1.8 | 3.45 ± 1.8 | P = 0.412 |
| Labor” duration (min) | 360 ± 180 | 310 ± 151 | P = 0.077 |
|
VAS1 0 30 min |
6.8 ± 2.2 1.6 ± 2.2 |
6.2 ± 2.4 2.4 ± 2.3* |
P = 0.125 P = 0.037 |
| Unilateral block (%) | 5 (7.1%) | 15 (21.4%)* | P = 0.029 |
|
Number of repeated injections of bupivacaine |
5 (7.1%) | 4 (5.7%) | P = 0.828 |
| Number of usage of fentanyl | 5 (7.1%) | 15 (21.4%)* | P = 0.029 |
Five primipara fulfilled the criteria for a unilateral block (7.1%) as did 15 multipara (21.4%) (P < 0.02). This difference was statistically significant between the two groups (Table 2 and Fig. 2). There were no differences between the groups with respect to paraesthesia, the difficulty of catheter insertion or blood appearing in the catheter. There were no dural taps during the study.
Number of fentanyl usage (50 microgram diluted in 5 mL of normal saline was given in the lateral position) due to unilateral block or inadequate block was increased in group B than in group A but fentanyl usage did not improve the unilateral or the inadequate block (Table 2).
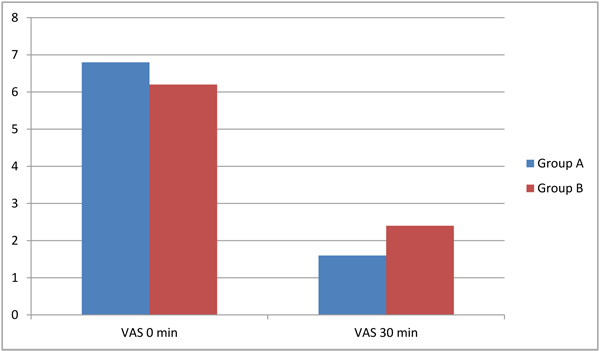 |
Fig. (1). Visual Analogue Scale (VAS) in the two groups. Bars represent Mean ± SD. |
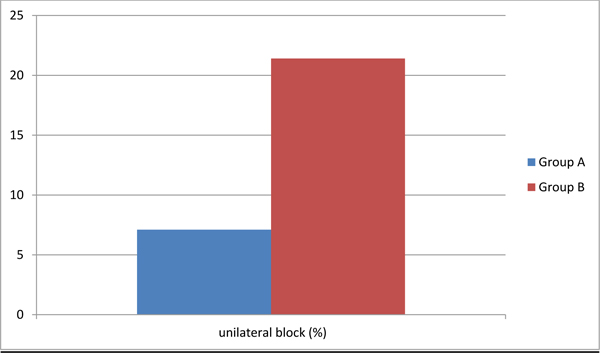 |
Fig. (2). Incidence of unilateral epidural block. |
4. DISCUSSION
Unilateral epidural analgesia is a common and persistent issue after epidural block. The phenomenon of unilateral epidural analgesia was first described in 1967 through radiographic analysis and examples of unilateral epidural analgesia continued to exist a half-century later [1].
The unilateral epidural blockade has an incidence between 5% and 21% of all epidural blocks. Persistent unilateral blockade is reported in 0.5% - 2% [2].
We evaluated the effectiveness of epidural analgesia between first and multiple epidural blockades in normal vaginal delivery and the incidence of unilateral epidural blockade. The major finding of our study was that the incidence of the unilateral epidural blockade was significantly higher in patients who received multiple epidurals than those who received it for the first time.
Consistent to our result, Narchi et al. [7] reported a unilateral block rate of 16% in repeated epidural analgesia against 7% in women receiving first epidurals. The point of difference was that the assessment was retrospective by means of a questionnaire administered in the post-partum period and the incidence of the persistent unilateral block was not recorded.
However, Bray and Carrie found no difference between women receiving their first or subsequent epidurals for labour when compared the efficacy of first with second epidurals [8].
Narchi et al. described a 13% incidence of the persistent unilateral block in women who had previous lumbar and caudal epidurals and 7% in women receiving their first epidurals [7].
Some studies reported the failure of epidural analgesia and its relation to a repeated epidural procedure. Camann reported an increased proportion of failed blocks as the number of previous epidurals increased [1].
Many hypotheses assumed to be the cause of unilateral epidural block. One of these causes is the presence of median connective tissue band, which may act as a barrier to the bilateral spread of local anesthetic. However, in autopsy specimens, resin injection studies have disagreed as to the consistent presence of a dorso-median fold [9].
Another method of examination was performed in cadavers; Epiduroscopy that had demonstrated a dorso-median fold in all the 48 cases studied [10].
Epidurography with computed tomography was also done to investigate the presence of a dorso-median fold in living patients. It has resulted in confirmation of its presence in 100% of examined people with 76% of them having sufficient midline tissue to be a potential impediment to catheter passage. This result is obviously grossly out of proportion to the clinical problem, suggesting that local anesthetic must diffuse through the connective tissue bands and the cause of unilateral block is not likely due to the dorso-median connective tissue band [11]. As barriers to the spread of local anesthetics are thought to be congenital, it may be also acquired as well as being congenital. It has been supposed formation of fibrous adhesions in the epidural space after the passage of an epidural catheter, mostly due to local irritation. There was one case of blood and granulation tissue in the epidural space in an autopsy after morphine infusion for a long time via an epidural catheter [12].
Localized adhesion bands and fibrosis after epidural blood patch are expected to be another cause as to affect subsequent local anesthetic spread as Selwyn Crawford that reported an incidence of two cases of an incomplete block (one unilateral block and one missed segment) in 17 women when received epidural analgesia after previous blood patch [13].
The sensory level could not be extended above T10 in Cesarean section in another case. A similar case has been reported with the failure of the block to spread above L2 following a blood patch performed at L1/2 three years previously [14].
The distance between skin and epidural space was also studied as a risk factor for the unilateral blockade. It has been suggested that the unilateral blockade is resulted from lateral catheter placement because of the deviation of the epidural Tuohy needle tip from the midline. The conclusion of a retrospective study of 3011 epidurals supported this theory as it found a strong positive correlation between the occurrence of unilateral blockade and distance between the skin and the epidural space. The incidence of the unsatisfactory block was more than 40% when the distance between skin and epidural space was greater than 6 cm [15].
Although the distance between the skin and the epidural space was not measured in our study, this factor is undoubtedly not responsible for the difference in the unilateral blockade in our study since there was no difference between the two groups in relation to weight (which has been shown to be directly related to the skin with the space of the epidural) [16].
CONCLUSION
The main conclusion of this study is that there is an increase in the incidence of unilateral block amongst women receiving repeated epidurals for labour than those receiving their first epidural block. Further investigation of this problem could be achieved by the study of a group of multigravida receiving their first epidural analgesia, a group difficult to find in our practice where the epidural rate is very high in primigravida. The role of the epidural catheter could be evaluated by injecting the initial dose through the needle prior to catheter insertion.
LIST OF ABBREVIATIONS
| ASA | = American Society of Anesthesiologists. |
| VAS | = Visual Analogue Score. |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the ethical committee of the Ain Shams University (file reference no. 105/2018).
HUMAN AND ANIMAL RIGHTS
No animals were used in the study. All humans research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2008 (http://www.wma.net/en/20activities/10ethics/10helsinki/).
CONSENT FOR PUBLICATION
A written consent for all the patients was taken.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.




