Tube-first Technique as a Conduit for Easy and Fast Nasal Fiberoptic Intubation
Abstract
Background:
Classical nasal fiberoptic bronchoscope intubation may be a challenging and lengthy procedure with a 1-10% failure rate.
Objectives:
This study aimed to compare among patients with difficult airway intubation undergoing general anesthesia, the safety, and efficacy of Tube-First (TF) nasal fiberoptic bronchoscope intubation against the Classic (CL) procedure.
Methods:
This single-blinded, parallel-group, randomized trial enrolled 40 adult patients with known difficult airways and scheduled for surgery under general anesthesia. The patients were randomly allocated into two (n=20 each) patient groups. In the CL group, the endotracheal tube and fiberoptic bronchoscope were inserted together through the nostril; in the TF group, the endotracheal tube insertion preceded the fiberoptic bronchoscope. In both groups, the bronchoscope was used to visualize the vocal cords and removed after ensuring the endotracheal tube position. The primary (efficacy) outcomes were the time elapsing from the bronchoscope insertion and visualizing the vocal cords (T1) and the time elapsing from the bronchoscope advancing initiation to its removal (T2). The secondary (safety) outcomes included oxygen saturation and hemodynamic parameters during the procedure.
Results:
The TF group showed a significant T1 and T2 mean reduction compared to those of the CL group (37.15 ± 3.87 and 64.25 ± 8.28 vs. 55.05±4.52 and 88.25±5.49 seconds, respectively; p < 0.0001). The oxygen saturation was comparable in both groups with no desaturation (SpO2 < 90%) cases. The heart rate and mean arterial blood pressure changes were significantly lower in the TF group compared to the CL group.
Conclusion:
Among patients with difficult airway intubation undergoing general anesthesia, we found the Tube-First intubation approach was quicker and safer compared to the classical intubation technique.
1. INTRODUCTION
Difficult intubation is one of the most significant issues anesthesiologists deal with occasionally. Among these, craniomaxillofacial deformities face the biggest challenge in intubation and make an anticipated difficult airway [1].
There are several strategies to approach these patients and each technique has unique benefits that should be used with experience [2]. Nowadays, the utilization of the conventional fiber-optic nasal intubation method in which the nasal tube is inserted in one step after visualization of the vocal cords by a flexible fiber-optic laryngoscope without the use of any facilitating techniques has proven to be a difficult task [3]. Fiberoptic bronchoscope (FOB) nasal intubation-aiding devices were originally designed to keep the airway patent by passing the relaxed redundant collapsible pharyngeal structure obstructing the airway. Attaching a nasal airway to a breathing circuit as a tool to assist or control ventilation is a very helpful trick in challenging airway management situations [4-6].
Inserting a tube nasally to or near the larynx has the advantage of keeping the airway patent as well as carrying the FOB tip immediately in front of the laryngeal inlet facilitating the process of laryngeal visualization and intubation without bloody secretions, especially in critical cases in which direct visualization is most challenging [7].
In the present study, the authors performed FOB nasal intubation as classically done (classical “CL” group) and thorough tube first (tube first “TF” group) comparing the effectiveness and safety in each group.
2. METHODOLOGY
The sample size was calculated using PASS 11.0 and based on a study carried out by Shoukry et al.,2018. revealed that forty subjects were needed, twenty in each group, to detect a difference of 6.2 between the null hypothesis that both group means are 92.6 and the alternative hypothesis that the mean of group II is 86.4 with estimated group standard deviations of 3.1 and 3.8 and with a significance (alpha) of 0.00500 using a two-sided two-sample t-test. The sample size was inflated by 10% to account for attrition in prospective studies.
2.1. Inclusion and Exclusion Criteria already Mentioned with the Type of Surgeries Done
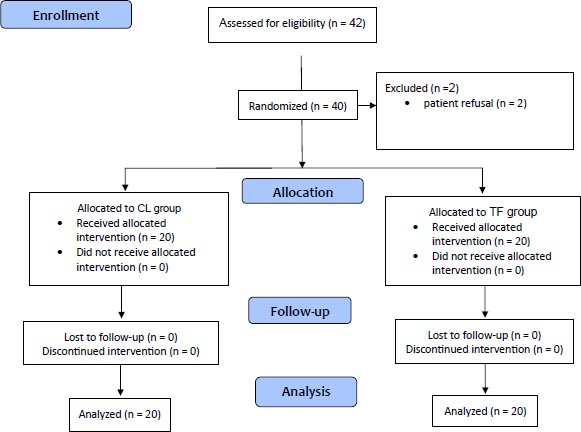
This prospective randomized controlled clinical study was conducted on 40 patients of both genders at the general surgery theater of Ain Shams University Hospitals after receiving approval from the local research ethics committee (No. IRB FWA 000017585 date 14/2/2022). The study was registered with clinical Trials.gov with No. (NCT05399147). Written informed consent was obtained from the patients. Patients were randomly divided into 2 groups (20 in each group) using a computer-generated random number table with either the classic technique group (CL group) or tube first technique group (TF group). We included ASA-I&II (American Society of Anesthesiologist) patients with difficult airway intubation, aged 20-60 years, undergoing maxillofacial surgeries, e.g.; mandibular surgery, orthognathic surgery, dental extraction surgery, or other surgeries like oral graft surgery, facial trauma, limited mouth opening e.g.; submandibular and facial abscess. Exclusion criteria included patient refusal with ASA III or more, intrinsic and idiopathic coagulopathy, known allergy to any of the study medications for all enrolled patients, full history, clinical examination, and routine laboratory investigations were done (Fig. 1). Pre-induction all patients had IV access (20-gauge peripheral cannula or more) using EMLA cream, premedication drugs such asmidazolam 0.05 mg/kg iv, dexamethasone 0.02 mg/kg iv, ondansetron 0.1 mg/kg iv, and atropine 0.05 mg/kg iv were given, nasal preparation using local vasoconstrictors (Xylometazoline hydrochloride 0.1% solution drops in each nostril) and Ceftriaxone 50 mg/kg after making sensitivity test as antibiotic prophylaxis.
General anesthesia with spontaneous ventilation was conducted under basic monitoring including Electrocardiogram (ECG), pulse oximetry, and non-invasive blood pressure applied to all patients, throughout the whole procedure, and in the post-anesthesia care unit (PACU).
In both groups, after oxygenation using a facemask with 100% fraction of inspired oxygen FiO2 & Sevoflurane 2%, and propofol 0.5 mg/kg IV were given, the nasopharyngeal airway (PVC airway, SunMed, Grand Rapids, MI, USA) with internal diameters of 6.0,6.5,7.0,7.5, and 8.0 mm) lubricated introduced to one of the patients preferred nostril and connected to modified Ayres’s T-piece circuit using endotracheal tube connector of the same size. Anesthesia was maintained using Sevoflurane 2% in 100% FiO2 and additional IV incremental doses of propofol (0.5 mg/kg) per dose titrated to deepen the level of anesthesia avoiding patient movement & coughing during the procedure when needed. Baseline arterial oxygen saturation (SpO2) together with hemodynamic parameters in the form of heart rate, systolic, diastolic blood pressure and mean arterial blood pressure (MABP) were recorded every minute throughout the procedure. Rocuronium (0.5 mg/kg) was given after securing the endotracheal tube (ETT).
In the CL group, after deepening anesthesia, ETT (Portex Ivory PVC, nasal soft seal cuff, tracheal tube by: Hi-tech surgical system, LLP, Mumbai) of average size was mounted in its place in the fiberoptic bronchoscope (KARL STORZ 11900 BP, Germany) and then after lubricating the fiberoptic bronchoscope the operator introduced it genteelly and smoothly through the nose till he visualized the vocal cord then the trachea and then ETT was slided over the bronchoscope to be inside the trachea and above the carina. After getting sure of the position, the fiberoptic bronchoscope was withdrawn and ETT was fixed and secured.
In the TF group, ETT (Portex Ivory PVC, nasal soft seal cuff, tracheal tube by: Hi-tech surgical system, LLP, Mumbai) of average size was lubricated well and its tip smoothed using hot fomentation, gently and smoothly inserted into the nose to the nasopharynx, then suctioning through the tube was done before introducing the fiberoptic, fiberoptic bronchoscopy was introduced through the previously positioned ETT till the end of the tube and slight manipulations were done till seeing the vocal cord and then the advancement of the bronchoscope to the trachea with smooth sliding of the ETT into the trachea, then removal of the bronchoscope from the tube after getting sure of the position and ETT fixed and secured.
The time elapsing from the bronchoscope insertion and visualizing the vocal cords (T1) and the time elapsing from the bronchoscope advancing initiation to its removal (T2) were recorded as our primary (efficacy) outcomes. The secondary (safety) outcomes included oxygen saturation and hemodynamic parameters during the procedure. Any complications like nasal bleeding or failure of the technique were recorded and ETT was inserted orally by laryngoscope. In case episodes of desaturation (Defined as SpO2 < or = 90%) occur, the procedure was stopped and the lowest SpO2 was recorded and ventilation assisted. The total incremental doses of propofol given were recorded and compared between both groups. Persistent hypoxemia that needed mechanical ventilation and muscle relaxant drugs (e.g.; laryngospasm or bronchospasm), Severe bleeding at the nasal side, or appearance of allergy to any of the drugs used were considered endpoints for the study.
2.2. Statistical Analysis
Data were analyzed using Statistical Package for Social Science (SPSS) version 22.0, quantitative data were expressed as mean and standard deviation (SD). Qualitative data were expressed as frequency and percentage. T-test was used for comparison between two groups with continuous data. The Chi-square (x2) test of significance was used to compare the proportions between two qualitative parameters. The confidence interval was set to 95% and the margin of error was set to 5%. So, the significance level was set at P ˂ 0.05.
3. RESULTS
This study enrolled 40 patients who were randomly allocated to two groups, either the classic technique group (CL group) or the tube first technique group (TF group). Both groups (20 patients each) were comparable regarding demographic data (Table 1).
Compared to the TF group, the CL group showed a significantly higher heart rate at the 2nd and 3rd minutes after induction with p values 0.0048 & 0.004, respectively (Table 2). Moreover, the mean arterial blood pressure was significantly higher at the 2nd and 3rd minutes after induction with p-values 0.0001 & 0.0028, respectively (Table 3). Meanwhile, there is a statistical elevation in the TF group in SpO2 compared to the CL group during the second minute only without a statistically significant difference at the first and third minute of oxygen saturation assessment (Table 4). The TF group showed a statically shorter time from inserting the fibreoptic till viewing the vocal cord T1 (p=< 0.0001), and also the total procedure time from inserting the fibreoptic till its removal is shorter when compared to the CL group T2 (p=< 0.0001) (Table 5). There were no significant differences between both groups regarding the total incremental dose of propofol consumed during the procedure (Table 6).
| Demographic Data | ||||
|---|---|---|---|---|
| - | Group CL | Group TF | Test | P-value |
| Age | 35.3 ± 14.94 | 33.9 ± 14.02 | 0.306 | 0.76 |
|
Sex • Male • Female |
12 (60%) 8 (40%) |
11 (55%) 9 (45%) |
0.102 |
0.75 |
| Weight | 73.95± 6.99 | 72 ± 6.15 | 0.937* | 0.35 |
| Height | 1.77 ± 0.09 | 1.74 ± 0.06 | 1.24 | 0.22 |
| BMI | 23.75 ± 1.95 | 23.72 ± 1.15 | 0.06 | 0.93 |
| Heart Rate (bpm) | ||||
|---|---|---|---|---|
| - | Group CL | Group TF | T test | P-value |
| Pre-procedure | 78.15 ± 6.16 | 75.9 ± 5.1 | -1.25 | 0.22 |
| 1st minute | 80.55 ± 6.41 | 77.15 ± 4.6 | -1.93 | 0.06 |
| 2nd minute | 82.65 ± 6.49 | 77.4 ± 4.4 | -2.99 | 0.0048 |
| 3rd minute | 83.05 ± 6.76 | 77.5 ± 4.4 | -3.08 | 0.004 |
| Mean Arterial Blood Pressure | ||||
|---|---|---|---|---|
| - | Group CL | Group TF | T test | P-value |
| Pre-procedure | 96.35 ± 5.07 | 98.25 ± 3.54 | 1.37 | 0.18 |
| 1st minute | 100.55 ± 4.52 | 99.9 ± 4.5 | -0.46 | 0.65 |
| 2nd minute | 104.35 ± 2.98 | 99.15 ± 3.83 | -4.79 | 0.0001* |
| 3rd minute | 100.35 ± 3.77 | 97.35 ± 1.84 | -3.2 | 0.0028* |
| Oxygen Saturation | ||||
|---|---|---|---|---|
| - | Group CL | Group TF | T test | P-value |
| Pre-procedure | 98.9 ± 0.3 | 99 ± 0 | 1.45 | 0.16 |
| 1st | 98.9 ± 0.31 | 98.9 ± 0.31 | 0 | 1 |
| 2nd | 98.5 ± 0.51 | 98.9 ± 0.31 | 2.99 | 0.048* |
| 3rd | 98.75 ± 0.55 | 98.95 ± 0.22 | 1.51 | 0.14 |
| Time | - | - | T test | P-value |
|---|---|---|---|---|
| - | Group CL | Group TF | - | - |
| T 1 | 55.05 ± 4.52 | 37.15 ± 3.87 | -13.45 | < 0.0001* |
| T 2 | 88.25 ± 5.49 | 64.25 ± 8.28 | -10.804 | < 0.0001* |
| Propofol Dose | - | - | T test | P-value |
|---|---|---|---|---|
| - | Group CL | Group TF | - | - |
| Dose (mg) | 123.75 ± 16.05 | 126 ± 15.69 | 0.448 | 0.66 |
4. DISCUSSION
Classical nasal fiberoptic intubation is commonly used in difficult airway intubation. The technique requires a relatively long time of intubation with difficulty in visualizing the glottis, which increases the patient’s discomfort [3]. Hence, there is continuous research for the appropriate approach using various facilitating devices such as nasopharyngeal airways, and intubating laryngeal masks to achieve minimal duration of fiberscope with rapid glottic visualization in different airway procedures.
In this study, we compared the safety and efficacy of the first tube technique as a conduit for nasal fibreoptic intubation versus the classic technique in terms of hemodynamic effects and duration of the procedure.
Safety was assumed as regards the hemodynamics measured during the procedure and with no complications and monitored as secondary outcomes.
As regard efficacy being measured by time as a primary outcome.
Baseline characteristics were similar in both groups, including age, sex, weight, height, body mass index, preoperative hemodynamics, and oxygen saturation. This could reflect a fair and balanced randomization. TF group showed a faster time from inserting the fibreoptic till viewing the vocal cords and also the total procedure time from inserting the fibreoptic till its removal is shorter when compared to the CL group (37.15±3.87 and 64.25±8.28 vs. 55.05±4.52and 88.25±5.49 seconds, respectively; p < 0.0001). Our results are in agreement with Mohammadzadeh et al. [8], that compared the classic and tube-first techniques by inserting the nasal tube into the nasopharynx till mark 18 in Iranian patients. It was thought that at 18 cm, the endotracheal tube reached a location near the vocal cords and served as a tool to help optimize the fiberscope as it is guided through the nasal cavity and toward the vocal cords. Both TI and T2 were significantly reduced in the tube first group (65.2 ± 33.2 and 87.1 ± 41.0 seconds, respectively) compared to the classic group (151.0±56.5 and 176.2±56.3 seconds, respectively). However, Mohammadzadeh et al. [8] found the power to detect a difference in the success rate of the tube first compared to the classic technique to be only 16% due to their small sample size. In our study, we didn’t need facilitation maneuvers such as head flexion or jaw thrust, or tongue retractors, thus, we had shorter times and this may be attributed to the use of the nasopharyngeal device through the other nostrils, also we were not committed to a fixed mark for the tube due to the large variation and discrepancy of various maxillofacial procedures.
Khalifa [9] compared awake nasotracheal intubation using the classic technique of video-scopic nasotracheal intubation and the tube first technique in which a lubricated nasal tube was introduced first into the nasopharynx until mark 18 in males and 16 in females acting as a conduit for the new disposable video-scope (scope 2). Both TI and T2 were significantly reduced in the tube first group (156.0 ± 0.81 and 198.6 ± 0.82 seconds, respectively) compared to the classic group (201.6 ± 1.15 and 244.8 ± 1.15 seconds). Furthermore, the tube-first approach decreased the scope twisting and the resulting traumatization of the upper airway, which increased the overall success rate of intubation with the tube-first approach. It was going the same with our study using the tube as a conduit, the difference was that we used the tube first technique in sedated patients not awake.
Syal et al. [10], compared the classic technique with a modified tube first technique by inserting the nasal tube into the nasopharynx until mark 15 in wakeful Indian patients. The tube crossed the nasopharynx, and its tip stood above the larynx, acting as a conduit to guide the tip of the scope through the glottis. This provided an appropriate space for manipulation. Both TI and T2 were significantly reduced with the modified tube first approach (108.6 ± 43.1 and 128.8 ± 43.7 seconds, respectively) compared to the other methods (142 ± 49.2and and 164.80 ± 48 seconds, respectively). Also, he did the technique in awake patients, but we used the same technique with sedation.
With the classic procedure, advancing the tube after glottis viewing might be challenging. Technical issues and a failure rate of 1% to 10% have been documented even in the best hands of experienced practitioners [11, 12]. The bronchoscope camera might become contaminated with nasal and oropharyngeal secretions [3]. Additionally, the gap between the tube and the fiberscope was thought to be the main cause of the difficulty in moving the tube over the fiberscope. This gap caused the tube to deviate in a direction that could damage the nearby anatomical structures like the esophagus, arytenoid cartilage, pyriform fossae, or epiglottis [13]. Additionally, the use of muscle relaxants or anesthesia causes the oropharyngeal muscles to paralyze, which causes the tongue and epiglottis to collapse back onto the posterior wall of the throat [5, 14]. The epiglottis has been reported as a common site of obstruction during nasotracheal intubation [5]. As a result, there isn't much space left for inserting the tube into the trachea [15, 16]. Thus, the tube-first technique could lessen the bronchoscope twisting and provide easier glottis viewing compared to the classic procedure.
Our study had a shorter time of intubation in both techniques than the previous research of Mohammadzadeh et al. [8] despite being done by junior staff under the supervision of an expert, we didn't need facilitation maneuvers such as head flexion or jaw thrust, or tongue retractors This may be attributed to the clinical condition of some patients where our patients were ASA class I-II, the use a nasopharyngeal device through the other nostril provided the advantage of both providing a state of deep sedation with inhalational anesthesia also preventing upper airway obstruction that might occur while using muscle relaxant. Furthermore, the frequent suctioning that was performed could have led to the clearing of the secretion and less fogging of the camera. These findings may oppose those of Khalifa [9] as he used a disposable fiberscope without suction for ASA class I-III patients who required careful and gentle manipulation. Some burn patients had limited mouth opening and restricted neck manipulation, which explains the prolonged time of intubation taken.
We did not find any cases of desaturation, and all patients had mean oxygen saturation above 90%. We found a statistical elevation in the tube first group compared to the classic group during the second assessment time, but it was of no clinical significance. Moreover, we found no statistically significant difference at the first and third time of oxygen saturation assessments. Syal et al. [10] reported a desaturation rate of just 3.3% with the modified tube first approach compared to a significantly higher frequency of up to 26.7% with the classic technique. This could be related to the use of sedatives and anesthetics that might collapse the upper airway. According to Law et al. [11], partial or total airway obstruction accounts for 5% of problems connected to awake fiberoptic bronchoscopy.
Meanwhile, the heart rate and mean arterial blood pressure were significantly increased with the classic technique compared with the tube first technique. Hemodynamic excitation was observed with the classic technique rather than with the tube-first technique. This could be explained in light of the research conducted by Mohamed El-Tawansy et al. [17]. They compared the classic technique to the split nasopharyngeal airway device that was inserted before the bronchoscope. The inserted fiberoptic bronchoscope shaft caused stressful excitation of the upper airway, mostly because - in the classical technique - the shaft is in direct contact with the airways for a considerable time during its journey.
One of the limitations of using this technique is that it limits the maneuvering of FOB, especially in some traumatic maxillofacial cases and also it needs careful preparation of the nose although we didn’t experience complications such as nasal bleeding.
CONCLUSION
Among patients with difficult airway intubation undergoing general anesthesia, we found the Tube-First intubation approach was quicker and safer compared to the classical intubation technique.
Quicker (1ry outcome): measured by the time.
Safer (2ry outcome): measured by the hemodynamics during the procedure.
LIST OF ABBREVIATIONS
| TF | = Tube-First |
| CL | = Classic |
| FOB | = Fiberoptic Bronchoscope |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This prospective randomized controlled clinical study was conducted on 40 patients of both genders at the general surgery theater of Ain Shams University Hospitals after receiving approval from the local research ethics committee (No. IRB FWA 000017585 date 14/2/2022). The study was registered with clinical Trials.gov with No. (NCT05399147).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patients.
STANDARDS OF REPORTING
CONSORT guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
The study utilized a grant from the Faculty of Medicine, Ain Shams University, and no external or industry funding was involved.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


