Are Combined Techniques using Video Laryngoscopes and Dynamic Stylets Superior to Fiberoptic Techniques for Anticipating Difficult Intubations? A Retrospective Single-center Comparative Analysis
Abstract
Introduction:
Studies point to the potential advantages of a combined technique using video laryngoscopes (VL) and dynamic stylets for difficult intubations. This study compares the outcomes of three advanced intubation techniques: combined technique (video laryngoscope + dynamic stylet), awake fiberoptic bronchoscope (FOB), and asleep FOB when used as the primary intubation technique.
Methods:
Airway notes of 138,387 consecutive anesthesia cases at a single academic medical center were filtered for the use of awake FOB, asleep FOB, or combined technique as the primary approach for potentially difficult intubations. The combined technique was defined as VL + dynamic stylet. The dynamic stylets available were FOB or TCITM (Total Control Introducer). The primary endpoint was the first pass success rate. Secondary endpoints included: failure to intubate with the primary technique, anesthesia “in room to intubation” time, “traumatic” intubation rate, and ease of intubation.
Results:
The first pass success rate was highest for combined techniques (88.7%) followed by awake FOB (74.2%, P<0.001) and asleep FOB (80.7%, P=0.06). “Failure to intubate” was lowest in the combined technique (1.8%), compared to awake FOB (9.2%, P=0.002). “In room to intubation” time was fastest for the combined techniques (13.0 minutes) followed by asleep FOB (15.1 minutes, P=0.002) and awake FOB (21.2 minutes, P<0.001). Combined techniques were recorded as “easy” significantly more often (72%) than awake FOB (38.2%, P<0.001). Combined techniques were recorded as “atraumatic” significantly more often (91.1%) than awake FOB (75.8%, P<0.001). Subgroup analysis of the combined techniques, VL + FOB vs. VL + TCITM, revealed that VL + TCITM was rated as “easy” and “atraumatic” significantly more often. It also achieved higher first pass success, lower “failure to intubate” rate, and faster “in room to intubated” time when compared with VL + FOB, although none reached significance.
Conclusion:
In this retrospective single-center comparative analysis, the combined techniques outperformed FOB techniques in effectiveness, speed, ease of use, and trauma.
1. INTRODUCTION
Multiple intubation attempts resulting in complications remain an important airway management problem [1, 2]. Standard tracheal intubation techniques using video laryngoscopy (VL) or direct laryngoscopy (DL) involve two steps; 1) glottic visualization and 2) tracheal access. Failure to intubate using standard DL or VL techniques is usually attributed to either difficult glottic visualization (most common in DL) or difficult tracheal access (most common in VL) [2-4].
Patients with risk factors for difficult intubation using standard DL or VL techniques may need advanced intubation techniques such as fiberoptic bronchoscopy (FOB), intubating supraglottic airways (SGA), lighted stylets or combined techniques (VL + dynamic stylet) [5]. The FOB helped overcome anatomic challenges by allowing both indirect visualization of the glottis and dynamic navigation around anatomic structures using a single device. In controlled studies of expertly trained providers, the FOB has a high rate of success [6]. However, these techniques require specific equipment, advanced training, and maintenance of specialized skills, potentially hindering safe airway management worldwide [1, 5, 7].
The combined technique is an advanced intubation technique that allows both indirect visualization of the glottis and dynamic navigation around anatomic structures using two separate pieces of equipment: 1) a VL for indirect visualization of the glottis and 2) a dynamic stylet for precise navigation of the trachea. Key features of dynamic stylets include an articulating tip for precision navigation and a flexible shaft that can conform to the entire serpentine pathway of the airway [8]. Recent studies of combined techniques have demonstrated high rates of success when managing anticipated and unanticipated difficult intubations [9-11].
The comparative performance of the combined techniques vs. FOB technique is unknown. We designed a study to compare effectiveness, speed, ease of performance, and oropharyngeal trauma between three advanced intubation techniques when used as a primary intubation approach in patients with anticipated difficult intubations. We formed a large database of perioperative medical records from a single academic anesthesiology department that consists of trainees, CRNAs, and anesthesiologists. The objective of this study was to compare combined techniques with awake and asleep FOB techniques. We hypnotized that combined techniques are associated with a higher first pass success rate, lower failure to intubate with the primary technique rate, faster “in-room to intubation time,” and higher ratings of “easy” and “atraumatic” intubations.
2. METHODS
2.2. Ethics Approval
This study was approved by the University of Utah Institutional Review Board #0096411. This study was in accordance with the ethical standards of the Declaration of Helsinki (1964) and its’ subsequent amendments. As this is a retrospective chart review, the University of Utah IRB waived the need for individual patient consent for this study and publication.
2.3. Electronic Medical Record Review (EMR)
138,387 consecutive perioperative records from 5/12/15 through 8/20/2020 were analyzed for the use of an advanced intubation technique as the primary approach for intubation. Inclusion criteria for advanced airway techniques: awake FOB, asleep FOB, or combined techniques (VL + FOB and VL + dynamic stylet). VL at the University of Utah (Salt Lake City, Utah) consists of GlideScope® Laryngoscope only; the dynamic stylet at this institution consists of TCITM dynamic introducer (Total Control Introducer, TTCmed.com; Salt Lake City, UT) only. This was verified by a review of the recorded devices used in the EMR. All devices studied were available as standard equipment in the University of Utah anesthesia workroom. No device required separate funding.
1,791 cases were identified in which an advanced airway technique was used as the primary approach to intubation. These cases were then filtered for at least one patient risk factor for difficult intubation. The inclusion criteria for an anticipated difficult airway were: Mallampati score of > 3; limited neck mobility; small mouth opening; body mass index (BMI) > 35 kg/m2; neck circumference > 35.5 cm in males or 32 cm in females; and history of difficult intubation. The exclusion criteria included EMR-documented elective or educational use of advanced airway equipment. A total of 849 cases met our inclusion criteria. Each airway note was analyzed for intubation devices, free text, airway procedure notes, case date, number of intubation attempts, “in room to intubation time,” ease of intubation, and intubation trauma. See Fig. (1) for data flow, advanced intubation technique taxonomy, and the groups compared.
The 849 cases were then evaluated for the primary endpoint: first attempt intubation success rate with primary advanced technique. Secondary endpoints included:
1) Failure to intubate using the primary advanced technique after 2 attempts.
2) Time from patient entry into the room to successful intubation (“in room to intubation” time).
3) User recorded ease of intubation in EMR airway note; easy, difficult.
4) User recorded intubation trauma in EMR airway notes; atraumatic, semi-traumatic, or traumatic.
The rationale for the choice of endpoints measuring effectiveness is as follows:
First intubation attempt success- Optimizing the first attempt intubation success is ideal when planning any intubation. Understanding the first-attempt success rates for different advanced intubation techniques can help clinicians choose an effective tool. Any attempt ≥ 2, whether successful or not, was excluded from this endpoint.
Failure of primary technique- We defined failure as ≥ 3 intubation attempts. Persistence with a failing technique correlates with poor outcomes [1]. It can increase the risk of adverse events, such as airway edema, oropharyngeal bleeding, or traumatic intubation.
In room to intubation time- This is the time from the patient is in the operating room to being intubated. Operating room time is a valuable and expensive resource. Aside from patient characteristics, the choice of intubation technique is known to affect the time needed to ready a patient before a surgical procedure can begin [12].
Ease of use- difficult intubations can be stressful for providers. Increased mental task load can impede performance and elevate the risk of negative outcomes during intubations [13]. Airway techniques necessitating the development and upkeep of advanced skills may be avoided by practitioners even when their use is appropriate [13, 14].
2.4. Groups and Subgroups Compared
The combined techniques (VL + FOB and VL + dynamic stylet) collectively were compared to awake FOB and asleep FOB. In a subgroup analysis of the combined techniques, VL + FOB was compared to VL + dynamic stylet.
2.5. Statistical Analysis
Patient demographics and outcomes were summarized descriptively and stratified by airway techniques. Continuous variables were summarized as mean and standard deviation (SD), median and inter-quartile range (IQR), and range. Categorical variables were summarized as frequency and percent. For each variable, we compared: combined techniques (VL+ FOB and VL + dynamic stylet) to Asleep FOB and Awake FOB using Wilcoxon rank sum test for continuous variables, and Chi-squared or Fisher’s exact test for categorical variables. Significance was assessed at P ≤ 0.05. Time from “in room to intubation” was summarized descriptively across the number of attempts, and the Jonckheere-Terpstra test was used to assess for a trend across the number of attempts. For this comparison, significance was assessed at P ≤ 0.05. Density plots were created to graphically present the distribution of time from “in room to intubation” across airway techniques.
All analyses were conducted in R v4.0.x [R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/], and all tests were two-sided.
3. RESULTS
The cohort included 934 intubation procedures and 849 patients (some patients presented for multiple procedures during the time frame evaluated). All filtering criteria were applied to the data already. Patient characteristics for each of the groups compared are presented in Table 1.
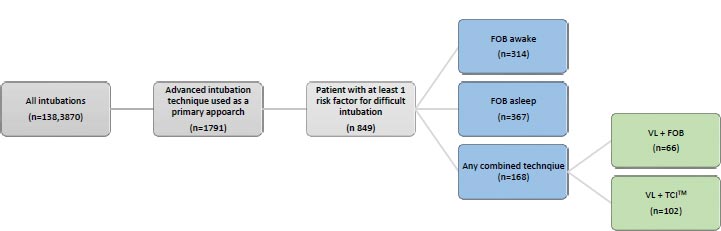
 Advanced intubation technique primary groups compared.
Advanced intubation technique primary groups compared. Combined technique subgroups compared.
Combined technique subgroups compared.
| Variable | Combined Techniques (N=168) | FOS Asleep (N=367) | P-value | FOS Awake (N=314) | P-value |
| BMI ≥ 35 kg/m2 | 41 (27%) | 46 (13.5%) | <0.001*c | 84 (27.8%) | 0.85c |
| Small mouth opening | 11 (6.5%) | 20 (5.4%) | 0.61c | 24 (7.6%) | 0.66c |
| Limited neck mobility | 55 (32.7%) | 144 (39.2%) | 0.15c | 183 (58.3%) | <0.001*c |
| Large neck circumference (cm) | 10 (6%) | 11 (3%) | 0.10c | 9 (2.9%) | 0.10c |
| Cervical spine precautions | 8 (4.8%) | 47 (12.8%) | 0.004*c | 24 (7.6%) | 0.23c |
| History of difficulty airway | 39 (23.2%) | 20 (5.4%) | <0.001*c | 40 (12.7%) | 0.003*c |
| Mallampati Class: | - | - | - | - | - |
| I | 22 (13.7%) | 51 (15.3%) | 0.016c | 22 (7.7%) | <0.001*c |
| II | 56 (34.8%) | 152 (45.5%) | - | 52 (18.2%) | - |
| III | 58 (36%) | 76 (22.8%) | - | 80 (28.1%) | - |
| IV | 25 (15.5%) | 55 (16.5%) | - | 131 (46%) | - |
c Chi-squared test, f Fisher's exact test.
*indicates statistical significance.
|
Variable |
Combined Techniques (N=168) |
FOS Asleep (N=367) | P-value | FOS Awake (N=314) | P-value |
| Number of Attempts: | - | - | - | - | - |
| 1 | 149 (88.7%) | 296 (80.7%) | 0.06c | 233 (74.2%) | <.001*c |
| 2 | 16 (9.5%) | 54 (14.7%) | - | 52 (16.6%) | - |
| ≥3 | 3 (1.8%) | 17 (4.6%) | ^0.11c | 29 (9.2%) | ^0.002*c |
| Minutes from in room to intubated: | - | - | - | - | - |
| Mean (SD) | 13.0 (7.3) | 15.1 (7.5) | - | 21.2 (11.2) | - |
| Median (IQR) | 12.0 (9.0, 15.0) | 13.0 (10.0, 18.0) | 0.002*w | 19.0 (14.0, 25.0) | <0.001*w |
| Range | (0.0, 65.0) | (4.0, 44.0) | - | (6.0, 96.0) | - |
| Difficulty: | - | - | - | - | - |
| Easy | 121 (72%) | 231 (62.9%) | 0.12c | 120 (38.2%) | <0.001*c |
| Difficult | 11 (6.5%) | 29 (7.9%) | - | 49 (15.6%) | - |
| Not rated | 36 (21.4%) | 107 (29.2%) | - | 145 (46.2%) | - |
| Traumatic: | - | - | - | - | - |
| Atraumatic | 153 (91.1%) | 328 (89.4%) | 0.91f | 238 (75.8%) | <0.001*f |
| Traumatic | 1 (0.6%) | 4 (1.1%) | - | 3 (1%) | - |
| Unknown | 14 (8.3%) | 35 (9.5%) | - | 73 (23.2%) | - |
c Chi-squared test, w Wilcoxon rank sum test, f Fisher's exact test.
*indicates statistical significance.
^Comparing #Attempts >=3 vs. <3.
| Variable | VL + TCI (N=102) | VL + FOB (N=66) | P-value |
| BMI ≥ 35 kg/m2 | 23 (23.7%) | 18 (32.7%) | 0.23c |
| Small mouth opening | 5 (4.9%) | 6 (9.1%) | 0.34f |
| Limited neck mobility | 31 (30.4%) | 24 (36.4%) | 0.42c |
| Large neck circumference | 8 (7.8%) | 2 (3%) | 0.32f |
| Cervical spine precautions | 2 (2%) | 6 (9.1%) | 0.06f |
| History of difficulty airway | 33 (32.4%) | 6 (9.1%) | <0.001*c |
| Mallampati Class: | - | - | - |
| I | 19 (19%) | 3 (4.9%) | <0.001*c |
| II | 40 (40%) | 16 (26.2%) | - |
| III | 33 (33%) | 25 (41%) | - |
| IV | 8 (8%) | 17 (27.9%) | - |
* Indicates statistical significance.
| Variable | VL + TCI (N=102) | VL + FOB (N=66) | P-value |
| #Attempts: | - | - | - |
| 1 | 92 (90.2%) | 57 (86.4%) | 0.63f |
| 2 | 9 (8.8%) | 7 (10.6%) | - |
| ≥3 | 1 (1%) | 2 (3%) | ^0.56f |
| Minutes from in room to intubated: | - | - | - |
| Mean (SD) | 12.1 (5.0) | 14.3 (9.9) | - |
| Median (IQR) | 12.0 (9.0, 14.0) | 13.0 (9.2, 17.0) | 0.12w |
| Range | (4.0, 34.0) | (0.0, 65.0) | - |
| Difficulty: | - | - | - |
| Easy | 85 (83.3%) | 8 (12.1%) | - |
| Difficult | 3 (2.9%) | 36 (54.5%) | <0.001*f |
| Not rated | 14 (13.7%) | 22 (33.3%) | - |
| Traumatic: | - | - | - |
| Atraumatic | 98 (96.1%) | 55 (83.3%) | 0.009f |
| Traumatic | 0 (0%) | 1 (1.5%) | - |
| Unknown | 4 (3.9%) | 10 (15.2%) | - |
* Indicates statistical significance.
^Comparing #Attempts >=3 vs. <3.
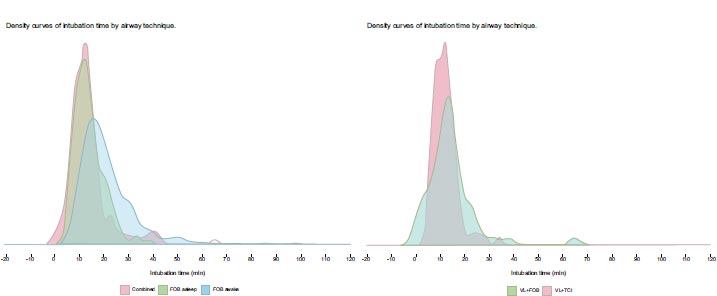
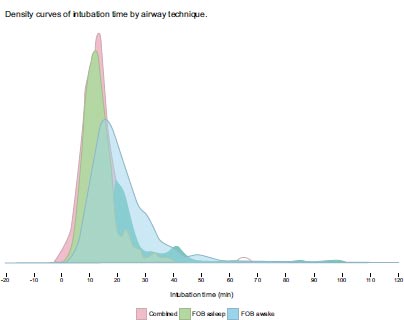
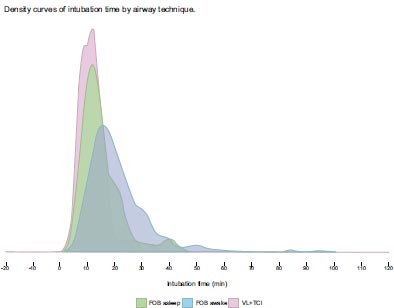
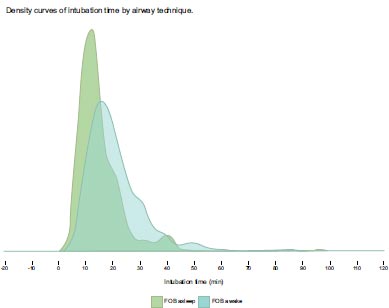
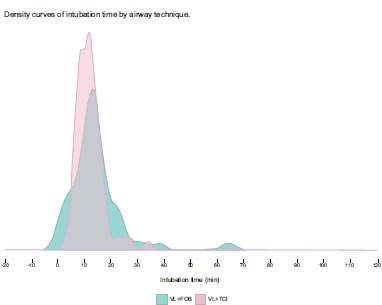
Results of the comparison of the combined techniques vs., awake FOB, and asleep FOB are presented in Table 2. A subgroup analysis was performed within the combined techniques category, comparing VL + FOB with VL + TCITM. That data is presented in Tables 3 and 4. Results of “in room to intubation” time for different techniques are presented as destiny curves. (See Fig. 2a and Fig. 3b).
The combined techniques achieved the highest first-pass intubation success rate of (88.7%). This was significantly higher than awake FOB (74.2%, P<0.001). The combined technique also had the lowest rate of “failure to intubate with the primary technique” at (1.8%), compared to awake FOB (9.2%, P = 0.002). The combined techniques were rated as “easy” (72%) significantly more often than awake FOB (38.2%, P < 0.001). The combined techniques were found to have a significantly shorter “in room to intubated” time (13.0 min) than either awake FOB or asleep FOB (15.1 min and 21.2 min, P = 0.002).
4. DISCUSSION
Our study reveals important information about the combined techniques, awake FOB, and asleep FOB as primary approaches to anticipated difficult intubations. “Difficult” implies increased mental task load which can compromise operator performance, thereby increasing risk. [13, 15] “Difficult” also implies additional training for proficiency and maintenance of skills, which can limit the success of advanced intubation techniques.
Operating room time is an expensive and limited resource. Joseph et.al. studied “in room to intubation” time and found significant increases in time associated with awake FOB vs. asleep FOB [12]. Our study confirms this finding. “In room to intubated” times for the combined techniques have not been studied. Minutes spent setting up the operating room is precious time. Minutes spent in prolonged single attempts or multiple intubation attempts may cause harm. Further study of efficiency is important for patient safety and reducing operating room costs.
As all techniques (combined techniques, awake FOB, asleep FOB) utilize dynamic and precise tracheal access, this implies that differences in trauma may be influenced by the mode of glottic visualization and/or navigation. Trauma from ETT tip catching on the glottis is a well-known problem with FOB intubation. VL provides visualization and displacement of the glottis as the ETT tip enters; a FOB alone does not. Additionally, the combined techniques achieve visualization and dynamic tracheal access with physically separate pieces of equipment, mechanically uncoupling visualization from dynamic tracheal access. This allows dynamic tracheal access to be monitored in a stable (non-dynamic) and panoramic visual field. In FOB equipment, visualization, and dynamic tracheal access components are mechanically coupled. This means visualization remains dynamic and non-panoramic throughout tracheal access when a FOB is used alone. We speculate that the combined techniques’ separation of visualization and dynamic tracheal access into two distinct entities may contribute to easier and less traumatic intubations.
Subgroup analysis of dynamic stylets revealed significant differences. While the VL component (GlideScope® Laryngoscope with hyper-angulated blade) of the combined techniques studied did not vary, the type of dynamic stylet did (FOB vs. TCITM dynamic introducer). The TCITM is a novel dynamic stylet with a fully articulated tip and a flexible shaft. Tip articulation is controlled by a removable pistol grip handle allowing single-handed dynamic navigation of the trachea. (Fig. 3).
While both the FOB and TCITM are dynamic stylets, they differ in two ways; 1) the TCITM has no intrinsic visualization capacity while a FOB does, 2) the TCITM dynamic introducer can be operated with a single hand enabling the execution of a single operator combined technique.
The use of a TCITM dynamic introducer was rated by the operator as “easy” and “atraumatic” at a significantly higher rate than FOB used as a dynamic stylet. The combined technique using a TCITM dynamic introducer resulted in a higher first pass rate and a lower “failure to intubate with the primary technique” when compared to FOB as a dynamic stylet. We speculate that two factors may account for these differences: 1) single-view vs dual-view combined technique and 2) single-operator vs. dual-operator execution.
| Combined Technique Subgroup | Dual View / Dual Operator | Dual View / Dual Operator | Single View / Single Operator |
|---|---|---|---|
| Visualization component |
 Dual view (VL + FOB) |
 Single view (VL only) |
 Single view (VL only) |
| Tracheal access component |
 FOB as dynamic introducer |
 FOB as dynamic introducer |
 TCITM dynamic introducer |
| Operator component |
 Dual operator |
 Dual operator |
 Single operator |
Both single-view and dual-view combined techniques are practiced at our institution. As the TCITM dynamic introducer has no intrinsic visualization capability, cases utilizing VL + TCITM are, by definition, a single-view combined technique. The combined technique using VL + FOB can be single-view (VL visualization) or dual-view (both VL and FOB visualization) [8, 11, 16]. In our database, the VL + FOB subgroup contains some dual view combined technique cases. We were unable to distinguish from airway notes between dual view and single view combined techniques for this subgroup. Both single-view and dual-view combined techniques have been reported and studied individually, however, these two subgroups have never been directly compared [9, 10]. Our data raises the possibility that a second FOB view may have an impact on the performance of the combined technique.
Furthermore, the combined techniques can be performed by a single operator or dual operator depending on the type of dynamic stylet used. (Table 5) [8], Single-operator procedures require less coordination and planning. The VL + TCITM allows for single or dual-operator use, while the VL + FOB requires additional assistance from a second provider. Coordination of the two operators and monitoring of the two fields of view may increase the mental task load in the primary operator and may affect performance [13, 15].
This study has limitations inherent to single-center, retrospective design. First, this study is not controlled for technique selection bias. Experience with a technique, availability of equipment, patient-specific physiology, and anatomical features can influence technique choice and outcomes. Second, this is a single-center study with providers of various skill levels. Caution is urged in generalizing these results. Third, Table 1 shows significant differences in potential difficult intubation risk factors between groups. These differences might influence the choice, difficulty, and outcomes of the different techniques studied. Fourth, this study includes only operating room intubations performed by anesthesia providers. Performance in other environments may vary. Fifth, recall bias is inherent as we are relying on provider documentation, which can be affected by providers inaccurately reporting the intubation. Despite these limitations, we believe this data provides new insights into the performance of different advanced intubation techniques in the natural workflow of a large teaching hospital’s surgical system.
CONCLUSION
The combined techniques may have advantages over the awake FOB and asleep FOB intubation approaches. It is a technique that could be considered a primary approach in anticipated difficult intubations. Prospective controlled trials should be designed and conducted to better understand the role of combined techniques as an advanced intubation technique.
AUTHOR’S CONTRIBUTION
Sean Runnels is the inventor of the TCITM dynamic introducer and holds shares in Cords LLC. He was not involved in data analysis or design in this study. He was involved in project management and manuscript preparation. No other authors have declared any competing interests. Presson and C Zhang (University of Utah, Dept of Statistics) handled all statistical evaluations including preparation, statistical methods, and preparation of results, (Tables 1, 2 and Fig. 3a-d).
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the University of Utah Institutional Review Board #0096411.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
As this is a retrospective chart review, the University of Utah IRB waived the need for individual patient consent for this study and publication.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the current study are available from the corresponding author [A.S] upon reasonable request.
FUNDING
None.


