Analgosedation Management in the Intensive Care Unit: A Narrative Systematic Review
Abstract
Background:
Intensive care unit (ICU) patients' pain and sedation management is a significant nursing challenge. Sedatives and muscle relaxants administration has been long used for improving patients' comfort and tolerance to mechanical ventilation. This practice led to an increase in adverse ICU outcomes in terms of health status, hospitalization stay, infections, and mortality. The use of appropriate ICU pain and sedation assessment tools is limited.
Methods:
We conducted a narrative literature systematic review (from 2010 to 2022) whose primary aims were to analyze the analgosedation definition and identify ICU patients’ pain, agitation, and sedation assessment tools; secondary aims were to explore analgesia and sedation pharmacological and non-pharmacological treatments and nurses’ perceptions and attitudes regarding analgosedation issues.
Results:
We retrieved 45 eligible articles. Analgosedation foresees early pain management - using pharmacological and non-pharmacological approaches and then, if necessary, implementing adequate sedation. Recommended assessment tools are the Behavioral Pain Scale (BPS) and the Critical Care Observational Tool (CPOT) for pain assessment, the Richmond Agitation Sedation Scale (RASS), and the Sedation Agitation Scale (SAS) for sedation assessment. Guidelines and specific protocols recommend both pharmacological and non-pharmacological approaches. Health professionals report mainly barriers (lack of adherence to guidelines and protocols, workload, reduced awareness, and own perceptions) to analgosedation correct application. The implementation of ICU analgosedation strategies requires continuous health professionals’ commitment and collaboration and valid assessment tools use.
Conclusion:
ICU analgosedation management (pain control first, and then sedation if necessary) is limited due to health professionals' knowledge gaps, inappropriate use of assessment tools, guidelines, and specific protocols. Recommended assessment tools are the BPS and CPOT for pain assessment and the RASS and SAS for sedation assessment. Interventions to improve ICU analgosedation awareness and practice include training events, the use and consultation of literature guidelines, and the use of validated assessment tools.
1. INTRODUCTION
The primary goal of Intensive Care Unit (ICU) patients’ pain and agitation management is to minimize patients’ physical and psychological discomfort. As such, it is considered a vital ICU nursing challenge. Nonetheless, 79% of ICU patients report having experienced moderate to severe pain [1], and 71% have an agitation state at least once during hospitalization [2, 3].
Sedative and muscle relaxant medications have been considered the best practice to promote ICU patients’ comfort and tolerance to mechanical ventilation. However, the literature shows that this practice has increased adverse outcomes for ICU patients regarding health status, hospital stay length, infection development, and mortality [4].
Pain is one of the most common symptoms among ICU patients. Undertreatment of pain at rest and during nursing and medical procedures causes increased patient suffering; it induces pathophysiological and psychological adverse clinical responses [3, 5, 6]. Notably, pain promotes catabolic hypermetabolism. The latter negatively affects wound healing, increases infection risk, alters hemodynamic function, and prolongs the need for mechanical ventilation [7]. Furthermore, psychological reactions to pain undertreatment lead to psychomotor agitation and delirium [1, 8]. The latter conditions often impose treatment with sedative drugs. Sedation objectives in the ICU are to reduce agitation and ensure patient safety, to minimize the risk of voluntary or involuntary patient self-removal of invasive devices (such as an endotracheal tube, drainages, and catheters), to optimize mechanical ventilation compliance to reduce respiratory work and oxygen consumption, improving patient's comfort, and providing amnesia and ease to promote adherence to stressful diagnostic and therapeutic procedures [8].
Analgosedation refers to applying pharmacological and non-pharmacological measures to ensure adequate analgesia and when required, adequate sedation [9]. Notably, one cannot treat what is not measured. Implementing adequate analgesia and sedation in ICU patients requires valid and reliable assessment tools to assess pain intensity, sedation, and agitation dimensions [8]. Several pain assessment tools are available for ICU patients. Nevertheless, the literature reports limited use of such tools [10, 11].
The primary aims of this study are to review the analgosedation definition and to identify ICU patients’ pain, agitation, and sedation recommended assessment tools. The secondary aims are to analyze analgosedation pharmacological and non-pharmacological treatments applicable in the ICU and, finally, to explore nurses’ perceptions and attitudes regarding analgosedation issues.
2. METHODS
2.1. Review Objectives
The objective of this comprehensive narrative synthesis of previously published information was twofold. First, we focused on analgesia and sedation in the critical care area as clinical concepts and their evaluation and management. In particular, we explored literature evidence for analgesia and sedation assessment tools, pharmacological and non-pharmacological management, and nursing management. Secondly, we surveyed the literature on ICU nurses’ attitudes, knowledge, and perceptions of analgesia and sedation issues.
2.2. Search Strategy
We conducted literature research, from January 2012 to June 2022, using the following biomedical databases: PubMed, Cinhal, Cochrane Library, and Trip Medical Database. We used specific MeSH terms and keywords combined with free search and specific search strings to select papers congruent with the research objectives, which may also enrich the topic knowledge.
We used the following MeSH terms: “analgesia”, “conscious sedation”, “critical care”, “deep sedation”, “intensive care units”, “mechanical ventilation”, “moderate sedation”, “nurse role”, “nurses”, “nursing assessment”, “pain management”, “pain measurement”, “pain perception”, “pain”, “pain/diagnosis”, and “psychometrics”.
In the free search phase, we used the terms: “analgosedation,” “drugs therapy,” “ICU analgesia,” “ICU sedation,” “mechanically ventilated patients or mechanical ventilation or intubated),” “nonpharmacological interventions,” “nonverbal intubated critically patients,” “nurse perception or experience,” “nurses attitude or perception.””nurses barriers,” “nurses perception,” “pain assessment and management,” “pain control,” “pain instruments,” “pain tools,” “sedation assessment and management,” “sedation,” and “sedoanalgesia,”
Finally, we used Boolean operators “AND” and “OR” to construct search strings to expand search options and a more thorough review of the present literature. Supportive material, table A, reports the 54 combinations we used for the literature research.
2.3. Papers Eligibility Criteria
Inclusion criteria for the review's eligible articles were articles published from 2010 to 2022, written in the English language, adult patients population (age >=18 years), relevant to the study's questions, and full-text availability. As for the articles' study design, eligible articles were: RCTs, systematic and non-systematic reviews, and guidelines. When appropriate, eligible articles were to clearly report information regarding data collection, statistical methods applied, and their results. Study design limitations were not used for articles regarding nurses' perceptions to obtain as comprehensive as possible results.
2.4. Papers Selection and Data Extraction
For their further selection, according to the inclusion criteria, the investigators (EL, VP, and CR) analyzed, independently and in parallel, the initially retrieved articles. Studies considered irrelevant to the research topics were discarded based on their title, keywords, and abstracts. Full-text duplicates and articles not fulfilling the study-design inclusion criteria were discarded. We also analyzed the selected articles' bibliographies to reveal papers not found in the first database research. In a subsequent session, the authors (EL, VP, CR, SS, and BGSD) discussed their screening results, and any discordance for discarding retrieved articles was solved by consensus.
Finally, the investigators (EL, VP, and CR) independently extracted data from the eligible studies using a standardized data collection table that included the papers’ authorship, year of publication, context/study population, study design, objectives, and outcomes. In the final data collection table, articles reporting was split, for convenience, into 2 major areas of interest: the analgosedation and nurses’ perception, and grouped by article’s type.
3. RESULTS OVERVIEW
Fig. (1) is a PRISMA flow diagram describing the eligible articles' selection process. Of the 1045 retrieved articles, 138 showed relevance to this review's objectives. Of the latter, we have discarded 93 because they were duplicates or not written in English. To the 41 selected studies, we have added another four found in the bibliography of the previously selected papers. The final 45 papers selected for this review are RCTs (n=11), guidelines (n=3), systematic reviews (n=11), reviews (n=9), and qualitative studies (n=11).
Table 1 is the data summary table reporting for each selected article the first author, publication year, context and study population, study design, objectives, and outcomes. Articles within the table were split into 2 areas of interest: analgosedation and nurses’ perception, and hence grouped by their study design.
Of the selected papers we have identified regarding the ICU analgesia and sedation topics, four specific macro-areas of interest: the clinical concept of analgesia and sedation, its perception by nurses, pain and sedation assessment, and pharmacological and non-pharmacological management. The following results presentation and discussion will follow these four specific macro-areas.
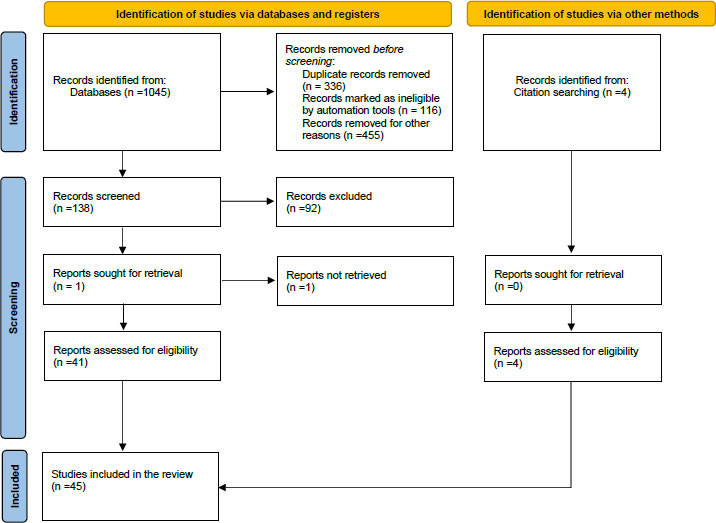
Table 1.
| Authors / Date | Context/Study Population | Study Design | Objectives | Outcomes |
|---|---|---|---|---|
| A. Analgosedation | ||||
| Aitken et al., 2018 [40] | ICU adults and children patients. | Systematic Review | To assess the effects of protocol-directed sedation management compared to usual care on the duration of mechanical ventilation, ICU and hospital mortality, and other patient outcomes. | There is currently limited evidence from RCTs evaluating the effectiveness of protocol-directed sedation. The four included RCTs reported conflicting results, and heterogeneity limited the interpretation of results for the primary outcomes of mechanical ventilation duration and mortality. |
| Barzanji et al., 2019 [28] | Critically ill adult patients admitted to cardiac surgical ICU. | Systematic Review | To identify the behavioral scales which are reliable and valid for pain monitoring in critically ill patients, incapable of verbalizing. | CPOT tool is likely to be an appropriate tool for pain assessment in patients admitted to post-cardiac surgery ICU under Mechanical ventilation who cannot express their pain according to examined validity, reliability, responsiveness rate, and utility. |
| Birkedal et al., 2021 [20] | Critically ill adult patients admitted to general and surgery ICU unable to self-report on pain. | Systematic Review | To compare the validity and reliability of the CPOT and BPS during painful procedures. | Both BPS and CPOT showed good reliability and validity and were good options for assessing pain during painful procedures. The CPOT is to be preferred since this tool was shown to have good reliability and validity for evaluating pain during procedures. |
| Marques et al., 2019 [27] | Critically ill adult patients admitted to medical/surgical/ trauma ICU unable to verbalize. | Systematic Review | To identify available scales/indicators for pain evaluation in critically ill patients unable to communicate. | The BPS and the CPOT are two scales recognized as reliable, valid, and easy to apply for pain monitoring in critically ill patients who cannot report their pain. |
| Pinheiro et al., 2019 [26] | Critically ill adult patients admitted to ICU unable to verbalize. | Systematic Review | To compare the validity and reliability of the CPOT and BPS. | Both BPS and CPOT showed good reliability and validity and were good options for pain assessment. |
| Shetty et al., 2018 [49] | Critically ill, mechanically ventilated, adult ICU patients. | Systematic Review | To assess the effects of BIS monitoring compared with clinical sedation assessment. | There is insufficient evidence about the effects of BIS monitoring for sedation in critically ill mechanically ventilated adults on clinical outcomes or resource utilization. The findings are uncertain due to the low- and very low-quality evidence derived from a limited number of studies. |
| Temesgen et al., 2021 [35] | Critically ill adult patients admitted to ICU. | Systematic Review | To define which outcomes are consequent to the management of analgosedation. | No protocol establishes how to treat pain and control sedation in ICU patients. Over sedation causes adverse effects such as prolonged mechanical ventilation, and hypo-sedation is associated with improved patient outcomes; RASS and CPOT are then described. |
| Varndell et al., 2017 [15] | Critically ill adult patients admitted to the ICU. | Systematic Review | To compare the validity and reliability of five tools (BPS, CPOT, FLACC, PAINAD, NVPS) in intubated patients unable to communicate and admitted to the adult emergency department. | The CPOT has the most substantial evidence regarding validity and reliability for pain assessment in intensive care critically ill patients. |
| Qi et al., 2021 [38] | Critically ill, mechanically ventilated, adult ICU patients. | Systematic Review and Meta-Analysis | To compare nurse-led sedation protocols with physician-led usual care in ICUs in treating mechanically ventilated adult patients. | Findings raise the considerable possibility that a sedation protocol can be safely implemented by nurses to reduce mortality in ICUs and sedation-related adverse events in patients on mechanical ventilation compared with physician-led usual care. |
| Wang CT et al., 2019 [9] | Critically ill adult patients admitted to ICU. | Systematic Review and Meta-Analysis | To assess the impact of analgosedation on mortality and delirium in critically ill patients. | The ICU mortality was decreased by implementing analgosedation, but the hospital mortality and the delirium rates were not. |
| Barr et al., 2013 [8] | Critically ill ICU adult patients. | Guidelines | To describe pain, agitation, sedation, and delirium management in ICU. | Pain and analgesia: pre-procedural pain assessment and under rest conditions, using rating scales and pharmacological and non-pharmacological interventions. Sedation: Prefer light sedation, avoid benzodiazepines, and use rating scales (RASS). Delirium: Definition of strategies pharmacological and non-pharmacological. |
| Devlin et al., 2018 [1] | Critically ill adult patients admitted to ICU. | Guidelines | To update and expand the 2013 guidelines “Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium” for patients admitted to the Intensive Care Unit. | 37 recommendations are identified. Two topics related to mobilization and sleep have been added. |
| Hinkelbein et al., 2018 [6] | Adult patients subjected to procedural sedation and analgesia. | Guidelines | To evaluate recommendations regarding procedural sedation and analgesia. | The assessment of PSA, the monitoring and prevention of adverse events, the role of doctors, and the drugs used are investigated. |
| Donato et al., 2021 [39] | Critically ill adult patients with COVID-19-associated acute respiratory distress syndrome. | Non systematic Review | To propose agile strategies for a comprehensive approach to analgesia, sedation, delirium, early mobility, and family engagement for patients with COVID-19. | It recommended using BPS and CPOT for pain assessment, RASS for level sedation, CAM-ICU for delirium assessment, and pharmacological and non-pharmacological strategies. |
| Burry et al., 2014 [41] | Critically ill, mechanically ventilated, adult ICU patients. | Review | To compare protocolized sedation with protocolized sedation plus daily sedation interruption in critically ill patients. | The addition of daily sedation interruption did not reduce the duration of mechanical ventilation or ICU stay. Patients in the daily interruption group received more opioids and benzodiazepines, and self-assessed nursing workload was higher for patients in the daily interruption group than in the control group. |
| Garrett et al., 2016 [4] | Critically ill adult patients admitted to ICU. | Review | To assess the impact of the guidelines published in 2013 by the Society for Critical Care Medicine. | Realization of a PAD Bundle and ABCDEF Bundle that provide a framework for facilitating the implementation of the guidelines. |
| Pearson and Patel, 2020 [37] |
Critically ill, mechanically ventilated, adult ICU patients. | Review | To explore the current evidence for sedation management during mechanical ventilation, including choice of sedatives, sedation strategies, and special considerations for acute respiratory distress syndrome. | Light sedation should be targeted early during mechanical ventilation utilizing daily interruptions of sedation and/or nursing protocol-based algorithms, even in severe ARDS. When choosing a sedative, benzodiazepines should be avoided in favor of dexmedetomidine or propofol. |
| Nordness et al., 2021 [10] | Critically ill adult patients admitted to ICU. | Review | To identify available scales for pain, agitation, and delirium assessment. | The BPS and the CPOT are scales recognized as reliable and valid for pain monitoring. At the same time, the NRS is helpful for patients who can verbalize. The main non-pharmacological intervention strategies are identified, such as massage therapy, music therapy, cold therapy, and relaxation therapies. |
| Wiatrowski et al., 2016 [3] | Critically ill adult patients admitted to ICU. | Review | To explore the concept of analgosedation, to provide better pain management and sedation. | Analgosedation can be a viable method for providing adequate pain control while minimizing sedation. It can decrease the risk of drug-related adverse events, increase pain control, decrease the length of mechanical ventilation and its associated risks, and decrease the length of ICU stay. |
| Gosselin et al., 2019 [55] | Critically ill adult patients admitted to the ICU. | Narrative Review | To explore whether the presence of the family during the pain assessment and treatment in ICU patients may be relevant. | The role of the family has been defined as of fundamental importance in the definition of pain in the ICU. Family members are careful in using the pain scales and reporting the pain of loved ones. |
| Laerkner et al., 2016 [60] | Critically ill, mechanically ventilated, adult ICU patients. | RCT | To investigate the differences in patient consciousness and nursing workload by comparing patients receiving no sedation with those sedated patients with daily sedation interruption and to estimate economic consequences. | Patients receiving no sedation were more awake, with a RASS score close to zero, compared with patients receiving sedation and daily interruption. Nurses reported no difference in self-assessed workload between the no-sedation and sedated groups of patients. |
| Mansouri et al., 2013 [14] | Critically ill adult patients admitted to ICU. | RCT | To design and use a protocol for systematic assessment and management of pain, agitation, and delirium by the nurses to improve clinical ICU outcomes. | The trial provided evidence for a substantial reduction in the duration of need for ventilatory support, length of ICU stay, and mortality rates in ICU-admitted patients through protocol-directed management of pain, agitation, and delirium. |
| Mehta et al., 2012 [42] | Critically ill, mechanically ventilated, adult ICU patients. | RCT | To compare protocolized sedation with protocolized sedation plus daily sedation interruption in critically ill patients. | For mechanically ventilated adults managed with protocolized sedation, the addition of daily sedation interruption did not reduce the duration of mechanical ventilation or ICU stay. |
| Olson et al., 2014 [36] | Critically ill, mechanically ventilated, adult ICU patients. | RCT | To determine whether the addition of a neurophysiological monitor, bispectral index, aided the ICU nurse in reducing the amount of drug use, compared to a clinical tool alone. | The clinical evaluation of sedation depth remains the most reliable method for the titration of pharmacological sedation. BIS-augmented assessment helps reduce the amount of propofol and narcotic medication used. It may be considered an adjunct when such agents are utilized. |
| Olsen et al., 2020 [43] | Critically ill, mechanically ventilated, adult ICU patients. | RCT | To investigate whether a plan of no sedation would result in a better survival outcome than a plan of light sedation with daily interruption. | Mortality at 90 days did not differ significantly between patients assigned to a no-sedation plan and those set to a light sedation with a daily interruption plan. Time on mechanical ventilation, length of ICU, and hospital stay did not differ significantly between the trial groups. |
| Rashidi et al., 2020 [44] | Critically ill, mechanically ventilated, adult ICU patients. | RCT | To evaluate the effect of using the Richmond agitation and sedation scale on hospital stay duration and dependency rate in the ICU. | Applying the RASS could reduce hospital or even ICU stay duration. This protocol can effectively optimize sedative medication use in the intensive care unit. |
| Saadatmand et al., 2015 [5] | A sample of 60 patients receiving mechanical ventilation support from a general ICU. |
RCT | To evaluate whether listening to pleasant natural sounds can reduce anxiety, agitation, and pain in patients able to communicate. | Listening to natural sounds for over 90 minutes is a practical, feasible, safe, and inexpensive intervention for reducing pain in patients undergoing mechanical ventilation. |
| Shehabi et al., 2013 [52] | Critically ill, mechanically ventilated, adult ICU patients. | RCT | To assess the feasibility and safety of early goal-directed sedation compared with standard sedation. | Delivery of early goal-directed sedation was feasible, appeared safe, achieved early light sedation, minimized benzodiazepines and propofol, and decreased the need for physical restraints. The findings justify further investigation of early goal-directed sedation. |
| Walsh et al., 2016 [59] | Critically ill, mechanically ventilated, adult ICU patients. | RCT | To assess 3 interventions effectiveness to improve sedation and analgesia quality: ● An online education program; ● Regular feedback on sedation-analgesia quality data; ● Use of a novel sedation-monitoring technology (the Responsiveness Index). |
RI monitoring and online education can improve sedation-analgesia quality and patient safety. The RI monitoring seemed to improve sedation-analgesia quality, but inconsistent adoption by bedside nurses limited its impact. The online education program resulted in a clinically relevant improvement in patient safety and was valued by nurses. Providing sedation-analgesia quality feedback to ICUs did not appear to improve quality metrics. |
| Mehta et al., 2016 [53] | Critically ill, mechanically ventilated, adult ICU patients. | RCT, Secondary analysis | To describe daytime and nighttime doses of sedatives and opioids, and to identify associations between these doses and conduct of spontaneous breathing trials and success of extubation. | Patients received higher doses of opioids and benzodiazepines at night. Higher nighttime doses were associated with spontaneous breathing trial failure and delayed extubation. |
| Nassar et al., 2019 [45] | Critically ill, mechanically ventilated, adult ICU patients. | Secondary analysis of RCT | To identify organizational factors associated with a moderate to light sedation target on the first 48 h of mechanical ventilation and the association between the early achievement of within-target sedation and mortality. | Board-certified intensivists on morning and afternoon shifts were associated with increased patients achieving lighter sedation goals. These findings reinforce the importance of organizational factors, such as intensivists’ presence, as an adjustable quality improvement target. |
| B. Nurses’ perception | ||||
| Rababa et al., 2021 [21] | ICU nurses. | Systematic review | To examine nurses' perceived barriers and facilitators of pain assessment and management in adult critical care patients. | Lack of pain assessment and management knowledge; pain scales are not used. Pain evaluation and preventive analgesia are underestimated before invasive procedures in low-level consciousness patients. Facilitating factors: a better understanding of pain-triggered behaviors and effects of pharmacological interventions, educational interventions on pain management evaluation. Barriers: inability of the patient to communicate, hemodynamic instability, absence of pain assessment tools, lack of standardized guidelines and protocols, workload, inadequate ratio nurse/patient, inadequate training, lack of knowledge of pharmacological and non-pharmacological pain management. |
| Kerbage et al., 2021 [16] | Critically ill adult patients admitted to ICU who cannot self-report pain. | Scoping review | Examine the evidence for pain assessment practices in adult sedated/ventilated patients. | Behavioral pain scales are essential but have limits, such as nurses' limited knowledge and skepticism, the impossibility of determining pain intensity and type, and no consideration for the patient's history. |
| Waterfield and Barnason, 2021 [19] | ICU nurses | Integrative review | To explore critical care nurses' perspectives of and intent to use recommended PADIS patient assessment tools in adult ICUs. | Examples of barriers to tool use and perceived norms found in the reviewed studies were low prioritization by colleagues and perceptions that the tool use annoyed others. Facilitating factors: communication and discussion with other professionals, implementation of educational interventions to teach its use and benefits. |
| Asman et al., 2019 [17] | A sample of 220 nurses of medical and surgical ICU. | Cross sectional qualitative study | To assess whether nurses' knowledge and perceptions of pain-expressing behaviors in mechanically ventilated patients may affect pain management and assessment in ICU. | High levels of knowledge. Discussion of analgesia during the nursing handover. The therapy prescription is based on the score of the scales rather than the direct evaluation. Barriers: workload, patient instability, inability of the patient to communicate, sedation that interferes with pain monitoring, absence of assessment pain scales. Facilitating factors: priority of management of pain, staff motivation, use of lines guidance and specific protocols, standardized pain assessment. |
| Deldar et al., 2018 [22] | A sample of 20 ICU nurses. | Qualitative study | To assess the knowledge, perceptions, and barriers nurses encounter regarding using behavioral observation scales in patients unable to communicate. | Different organizational, attitudinal, and cognitive barriers to correctly using these scales emerge (absence of pain scales and protocols, doctor-nurse inadequate interaction, significant workload, the inappropriate relationship between nurses/patients, the ratio of nurses with little experience, and insufficient nurses training. |
| Hamdan et al., 2020 [23] | A sample of 300 ICU nurses. | Qualitative study | To explore ICU nurses' pain education, perceived barriers, and enablers of pain assessment and management practices among critically ill patients. | Barriers: workload, patient instability, inability of the patient to communicate, sedation that interferes with pain monitoring, absence of pain scales. Facilitating factors: priority of management of pain, staff motivation, use of protocols, standardized pain assessment. Analgesia is discussed more during the handover. |
| Hetland et al., 2018 [24] | A subsample (n = 67) of ICU nurses | Qualitative study | To assess nurses’ perceptions of current sedation administration practices. | Multiple factors guided sedation administration practices, including individual patient needs, nurses' synthesis of clinical evidence, application of best practices, and various personal and professional practice perspectives. Sedation assessment is done using scales, BIS, and physical parameters. |
| Kizza et al., 2016 [58] |
A sample of 170 ICU nurses | Qualitative study | To determine nurses’ level of knowledge concerning principles of acute pain assessment in critically ill patients. | Most nurses report how scales are not used for pain evaluation; those who confirm using pain scales would use NRS, VAS, and Wong-Baker FACES. More than 70% report discussing the correct management of analgesia during the transition of deliveries. Barriers: excessive workload, poor knowledge of the topic, unfamiliarity and absence of validated tools, protocols, and guidelines, poor documentation, and discussion of analgesia. Facilitating factors: prescription of correct analgesia. |
| Mortensen et al., 2019 [25] | A sample of five pairs of expert and competent ICU nurses with respectively >8 and 2-3 years of ICU experience. | Qualitative study | To compare the perspectives of expert and competent nurses regarding their interaction with non-sedated mechanically ventilated ICU patients. | Benefit of sedation but difficulty in interaction with the patient due to insecurity in communication. More accessible nursing care to the sedated patient; furthermore, the awake patient is more easily subject to developing delirium. The awake patient requires a 1:1 patient/nurse ratio. |
| Randen et al., 2013 [56] | A sample of 183 ICU nurses in Norway. | Qualitative study | To describe intensive care nurses' perceptions and assessments of unpleasant symptoms and signs in mechanically ventilated and sedated adult intensive care patients. | More attention should be regarding under sedation rather than over sedation. Nurses consider behavioral signs (e.g., response to contact) and ventilatory signs as the most important. |
| Rose et al., 2012 [11] | A sample of 842 nurses responded to a self-administered questionnaire. | Qualitative study | To document knowledge and perceptions of pain assessment and management practices among Canadian intensive care unit nurses. | Nurses use behavioral scales less than self-reported pain scales. The analgesia is more discussed during the handover. The most commonly used behavioral scale is the BPS. Vital parameters are considered moderately to extremely important for pain assessment. |
| Sneyers et al., 2014 [18] | A sample of seven nurses per ICU in the 101 adult ICUs in Belgium. | Qualitative study | To assess common nurses’ perceptions by facilitating and stimulating analgosedation strategies. | Perceptions on analgosedation: the use of scales increases autonomy, enhances one's own role, improves patients' outcomes, and helps the monitoring of sedatives and control of costs; However, half of the professionals think that the level of sedation can also be assessed without using validated scales. A sedated patient is easier to manage: it involves less nursing work and fewer risks for the patients. |
| Tsang et al., 2019 [57] | A sample of 46 ICU nurses. | Qualitative study | To explore ICU nurses' experiences, beliefs, and perceptions on managing pain, agitation, and delirium in critically ill patients. | Deep sedation does not allow neurological status evaluation. Still, at the same time, the awake and agitated patient can cause damage to himself and to the operators. Also, it is reported that it is easier to assist deeply sedated patients than awake and restless. Attention to the environment that improves the patient's comfort (turn off the lights in the evening, minimize noise, etc.) and integration of the family in decision-making and care processes. |
| Wang and Tsai, 2010 [13] | A sample of 370 ICU nurses from 16 hospitals in Taiwan. | Qualitative study | To explore nurses' knowledge and barriers regarding pain management in ICUs. | Most respondents have never received pain management training. More than 80% of nurses believe patients overestimate their pain; opioid use leads to respiratory depression and addiction. It is reported that there are no tools to assess pain in patients who cannot communicate. |
3.1. The Analgosedation Concept
Patients’ sedation with hypnotic drugs and pain management with analgesics (opioids or not) are among the critical practices in the ICU [12]. Sedoanalgesia refers to applying hypnotic drugs and, hence, analgesics as needed. However, sedation hampers pain and discomfort evaluation [10]. Analgosedation, a newer concept, refers to pain management first and, if necessary, applying sedation [9].
Compared to sedoanalgesia, analgosedation shows better patient, health professionals, caregiver interaction, and ICU clinical outcomes, including mortality reduction [1, 9, 10, 13, 14].
A practical tool to manage ICU patients’ analgosedation is the ABCDEF Bundle [2, 12]. The ABCDEF acronym is “Assess, prevent and manage pain (A), both spontaneous awakening and spontaneous breathing trials (B), Choice of analgesia and sedation (C), assess, prevent and manage Delirium (D), Early mobility and exercise (E), and Family engagement (F).” Implementing the ABCDEF Bundle recommendations may improve ICU patients’ comfort, and interpersonal communication, and clinical outcomes [4, 9, 12].
3.2. Pain Assessment in the ICU
Because pain is multidimensional and subjective, a patient's pain self-assessment is the gold standard for its quantification [1, 7, 15]. Indeed, in ICU patients who can communicate, the numerical rating scale (NRS) and the visual analog one (VAS) have proved to be the most valid for self-assessment.
Pain assessment is challenging in patients who cannot communicate because they are intubated or mechanically ventilated. Several tools are available for appropriate pain assessment in the ICU [15, 16]. Nevertheless, a Canadian study shows that only 19% of the analyzed ICUs use such tools [10].
The American Society for Pain Management Nursing recommends using pain assessment tools to detect observable pain as a substitute for the patient's pain self-assessment [17].
Behavior observation is recommended to detect pain in the unconscious patient [16, 17]. Research has focused on studying behavioral manifestations that may indicate pain presence [16]. Such behavioral manifestations include facial expressions, upper limb movement, and patient compliance with mechanical ventilation. Behavior observation most used scales in the ICU are the Behavioral Pain Scale (BPS) and the Critical Care Observational Tool (CPOT) [15, 17, 18].
CPOT and BPS have been extensively validated, and thus applicable to ICU patients [15, 17, 19]. Validation has been done in several languages, including Italian [20, 21].
3.3. Sedation Assessment in the ICU
Appropriate sedation treatments for different types of patients remain challenging for ICU professionals [22]. Using sedation rating scales as part of a sedation management protocol enables professionals to appropriately titrate and administer sedation treatments to ICU patients [14, 23-27].
However, while there is evidence that protocols are effective in patients receiving no- or light sedation [3, 9, 14], not all studies agree on their effectiveness in patients with daily sedation interruptions [28, 29].
Furthermore, Olsen et al. [30] investigated the effects of a non-sedation protocol compared with the light sedation one. They found no differences in terms of 90-day mortality, ventilator-free days, ICU and hospital length of stay.
ICU multidisciplinary teams commonly use sedation rating scales to promote professional communication and to set goals that can lead to reductions in sedation use, mechanical ventilation duration, and ICU length of stay [25, 31, 32].
Several sedation assessment scales with different quality levels are available for ICU patients [22]. In 2013, the ICU Pain, Agitation, and Delirium (PAD) Guidelines concluded that the Richmond Agitation Sedation Scale (RASS) and the Sedation Agitation Scale (SAS) are the most valid and reliable sedation quality and depth assessment tools for critically ill patients [8]. The PAD bundle recommends sedation assessment and documentation in all ICU patients, using the RASS or SAS, at least four times per shift (i.e., every 2 or 3 hours) and as needed.
Finally, for other sedation monitoring systems, the bispectral index (BIS), showed insufficient evidence for ICU sedation monitoring [33].
3.4. Pharmacological Management
Clinical Practice Guidelines for the “Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption” in ICU Adult Patients were published in 2013 and 2018 [1, 8]. These guidelines recommend, in the first instance, intravenous opioids for the treatment of non-neuropathic pain [34]. All intravenously administered opioids [35] (such as fentanyl, hydromorphone, methadone, morphine, and remifentanil) are equivalent when titrated to pain intensity [1, 8].
The individual patient's sedation indications and goals should guide the sedative drug choice considering the patient's clinical conditions and the chosen drug onset, offset, and side effects [1, 8]. Some studies have shown that midazolam, propofol, and dexmedetomidine are the most used ICU sedative drugs [1, 8, 35, 36].
3.5. Non-Pharmacological Management
In recent years several studies addressed the use of non-pharmacological strategies for ICU pain management [5, 34, 35, 37]. Non-pharmacological strategies include options such as music intervention, imagery, aromatherapy, massage, and family presence [8, 8, 10, 38-42]. However, the latter strategies are still not fully explored and are rarely used in daily practice [34].
The Society of Critical Care Medicine's ICU Liberation Bundle recommends four main non-pharmacological methods: massage therapy, cold therapy, music therapy, and relaxation techniques [1, 10, 13]. These methods aim to address the pain's physical-sensory component (massage therapy and pain therapy) and the emotional and cognitive ones (music therapy and relaxation techniques). Some methods have demonstrated a pain score reduction in both visual/verbal numerical scales and behavioral scales [1, 10].
3.6. Analgosedation and Nurses’ Perception
Nursing personnel prefer evaluating pain and analgesia by measuring the patient's physiological parameters or observing behavioral elements while using behavioral dedicated scales is limited [43-47]. Limitations to the latter scale application by nurses are their limited knowledge and the mistrust concerning the effectiveness and benefit of their use [43-46, 48, 49].
Further barriers to nurse analgosedation evaluation are heavy workload, the patient's clinical instability and communication inability, deep sedation interfering with pain monitoring, lack of appropriate pain and sedation assessment tools, nurse-physician poor communication, lack of workplace standardized guidelines and protocols, inadequate training and education, lack of knowledge and consideration for the analgosedation issue by health professionals [11, 13, 43-52].
Recognized elements that may improve correct ICU patient pain and sedation management are understanding pain-triggered behaviors, pharmacological interventions effects, pain management educational interventions, facilitating communication and discussion among health professionals, educational interventions on assessment tools benefits, pain management priorities, staff motivation, using specific guidelines and protocols, standardized methods of pain assessment and correct prescription of analgosedation [11, 13, 39, 44, 47-49, 51, 52].
4. DISCUSSION
In this narrative review, we analyzed 45 papers from international databases published between 2012 and 2022 addressing the issues of ICU patients’ analgesia and sedation with additional attention to the nurses’ point of view. Analyzed articles included RCTs, guidelines, systematic reviews, reviews, and qualitative studies. We focused on four macro-areas relative to ICU patients: the analgosedation concept, pain and sedation assessment, pharmacological and non-pharmacological management, and analgosedation perception by nurses.
4.1. The Analgosedation Concept
Minimizing ICU patients’ physical and psychological distress by managing their pain and agitation is an obvious nursing consideration. However, over 70% of ICU patients experience moderate to severe pain and an agitation state at least once during their hospital stay [1, 2]. ICU patients can experience significant pain and elevated levels of agitation, which, if left untreated, can lead to psychological and physical complications and the development of chronic pain post-ICU discharge [3, 5].
Sedation and analgesia are standard practices in the ICU environment to prevent patients' psycho-physical stress and discomfort. ICU patients' sedation, primarily with hypnotic drugs (e.g., midazolam or propofol) and analgesics (e.g., opiates or non-opiates drugs), as needed, has been considered the conventional practice [12]. This combination approach of hypnotic and analgesia agents is commonly described as sedoanalgesia. Nonetheless, hypnotic drugs yield consciousness suppression that prevents patients from directly reporting symptoms and thus humpers recognition, evaluation, and treatment of their discomfort and pain [10]. It was hence necessary to overturn from the sedoanalgesia concept, where sedation was the management pillar, to the analgosedation one, where analgesia is the primary approach, and sedation is complimentary. In particular, the patient's pain should be first identified and managed, and sedation should be added if needed [9].
Analgosedation includes pharmacological and non-pharmacological treatments to prevent and control the patient's pain. The analgosedation goal is to keep the patient pain-free and to provide, only if needed, an appropriate sedation level; this approach enables calmer and positively reacting patients, improving their interaction with the ICU environment, healthcare professionals, and family members, better clinical outcomes, and shorter ICU and hospitalization length of stay [13]. Compared with a sedation-based approach, ICU approaches based on patient pain assessment and management reduce the need for sedation, length of mechanical ventilation and ICU stay, and patient-reported pain [1, 10, 14]. Moreover, in their systematic review, Wang et al. demonstrated that the analgosedation approach reduces mortality in intensive care [9].
The analgosedation concept finds its implementation in the ABCDEF Bundle [2, 12]. The latter is a set of recommendations for the prevention, assessment, and management of pain, agitation, and delirium to optimize ICU patients’ management and clinical outcomes. It consists of specific sets of evidence-based interventions and ensures ICU liberation [10]. While the ABCDEF Bundle can be complex, it improves communication between healthcare professionals, standardizes care processes, and reduces the risk of deep sedation and prolonged mechanical ventilation, which can induce delirium, keeping the patient and the family at the center of care [4, 12].
In this review, we found that the clinical concept of analgosedation is of recent development and interest, and current guidelines show that there is still no analgosedation unambiguous definition [1, 8]. This definition is poorly understood, and most ICU nurses consider pain and sedation separately. Only three studies define the analgosedation concept as the practice that favors analgesia management over patient sedation [1, 9, 10]. The lack of consideration for this new concept can lead to an incorrect and incomplete control of the level of sedation and pain management. The diffusion of this new view according to standardized tools and protocols should be one of the most critical measures to deal with this issue.
4.2. Pain Assessment
Pain is a vital parameter to be constantly assessed during hospitalization; however, its evaluation in the ICU environment is not optimal. Managing pain and agitation requires valid and reliable tools for their assessment in ICU patients. For patients able to communicate, pain self-reporting is considered the gold standard. Patients' self-reporting tools are the VAS and NRS. In the latter, patients directly report their pain intensity by choosing a number ranging from 0 to 10, where '0' represents no pain, and '10' is the most intense pain imaginable [1, 7, 15]. The presence of delirium, motor, auditory or visual issues, and the patient's lack of cooperation represent the only practical limitations [8, 10, 38].
Pain evaluation is challenging when patients cannot communicate because they are sedated and mechanically ventilated. We found in the literature comprehensive agreement that the BPS and the CPOT are the most appropriate tools for pain assessment in patients who cannot communicate [8, 15, 17, 18].
In the literature, the patient’s vital signs may indirectly indicate pain presence; however, these signs are considered nonspecific pain indicators [8, 10, 16, 38]. Nevertheless, nurses often observe these signs to detect pain [10, 11, 17-19, 38]. Vital parameters (such as heart rate, respiratory rate, EtCO2, and SpO2) can increase and change during nursing and clinical procedures (painful or not); however, they can also remain unmodified, leading to an inappropriate pain assessment [8, 10, 38].
The BPS was the first pain assessment tool designed for the unconscious or sedated patient [16, 19]. It scores three observable behavioral dimensions: facial expressions, movement of the upper limbs, and patient compliance with mechanical ventilation. Each dimension score ranges from 1 to 4, and the possible total sum of the three dimensions scores ranges from 3 to 12. A total score of 3 denotes the pain absence, 4 to 6 mild, 7 to 9 moderate, and 10 to 12 severe pain; a total score ≥6 implies pain needing treatment [19, 42]. The BPS has proven to be valid for assessing pain in ICU patients, albeit with some limitations relating to the field of application. The BPS does not apply to patients with tetraplegia, curarized [42], or affected by peripheral neuropathies [53].
For patients with verbalization limitations, the CPOT considers four behavioral dimensions: facial expressions, body movements, muscle tension, and respiratory/phonatory activity. The latter dimension is split for intubated and not-intubated patients. In the intubated patient, compliance with mechanical ventilation is assessed; in the non-intubated patient, phonatory features are considered. Scores for each item range from 0 to 2, with a total score between 0 (absence of pain) and 8 (worst possible pain); a score greater than 2 implies pain needing treatment. In particular, scores from 0 to 3 indicate mild pain, 3 to 6 moderate, and 6 to 8 severe pain. Several studies have evaluated the CPOT validity in medical, surgical, and neurological ICUs [54]. CPOT and BPS do not appear suitable for people with head trauma because the underlying pathology can limit the pain's behavioral manifestations (e.g., the absence of muscle tone and grimacing) [16]. CPOT and BPS-NI appear valid in patients with delirium; still, more studies are needed to confirm these results [15]. There are no validation studies of CPOT and BPS in patients with cognitive impairment [54].
Nonetheless, these pain scales bear some limitations that may affect evaluation. For the BPS, items like body movement and compliance with mechanical ventilation may be subject to incorrect interpretation; they thus may lead to over- or underestimation of patients' pain levels [20, 34]. Moreover, the distinction between pain and discomfort is challenging when evaluating the patient's condition. For this reason, compared to the CPOT, the BPS showed more significant specificity but lower sensitivity. In an observational study, Severgnini et al. found that some CPOT items not addressed by the BPS (e.g., muscle tension and facial expression) are more representative of pain [34]. Thus, the CPOT appears more appropriate for ICU routine and procedural pain assessment. A systematic review conducted in 2019 concludes that the CPOT is probably the most valid, reliable, and with the best response rate scale for post-cardiac surgery ICU patients who cannot communicate [28]. Considering that pain is an ever-present symptom in the ICU, possessing knowledge about the most appropriate pain scales and indicators may contribute to improving practices.
ICU healthcare professionals tend to underestimate the patient's pain, and about half of ICU patients do not receive adequate pain management [7]. Causes are ineffective caregiver and patient communication due to the patient's intubation and mechanical ventilation, excessive sedation, or cognitive impairment [15, 20]. Aside from the latter, qualitative studies have identified other barriers to ICU patients' pain assessment caveats. These barriers include healthcare professionals' limited perceptions, knowledge, and autonomy in providing analgesia and the lack of appropriate pain assessment tools [16, 18, 21-25].
Despite the comprehensive agreement on these assessment tools' validity and wide availability, the literature shows that their use is inconsistent and that healthcare professionals often apply pain and agitation assessments using subjective empirical criteria, such as personal perceptions, beliefs, and prior experience [11, 13, 43-52].
Furthermore, in a recent ICU pain-management guideline (2018), the pain assessment and reporting frequency are not defined; however, it recommends constant and routine pain assessment at rest and before nursing procedures [1]. In their review, Nordness et al. recommend pain assessment every 2-3 hours when the patient’s clinical conditions change and during invasive procedures [10]. To note, less than 25% of ICU patients do not receive adequate analgesia for invasive procedures [1, 20]. Notably, the lack of adequate analgesia for a painful procedure may induce pain-related adverse events such as tachycardia, bradycardia, desaturation, respiratory distress, altered blood pressure, and a vasovagal reaction [1].
4.3. Agitation and Sedation Assessment
We found in the literature comprehensive agreement that the RASS and the SAS are the most suitable tools for sedation assessment [8, 15, 17, 18]. Sessler formulated the RASS in 2002 [55]. It is a 10-item scale consisting of four levels of anxiety or agitation (scores from +1 to +4: the patient is restless, agitated, extremely agitated, or combative, respectively), an item to indicate a state of calmness and alertness (0), and five levels of sedation (scores from -1 to -5: drowsy, light sedation, moderate sedation, deep sedation, or unarousable, respectively). RASS scoring follows three types of evaluations: patient observation, verbal, and physical stimulation. Initial patient observation seeks signs of agitation: anxiety, purposeless movements or impaired patient-ventilator synchronization, aggressiveness, and violent behavior. Follows sedated patient's reaction to verbal stimulation seeking subsequent eye opening and eye contact maintenance time (more or fewer than 10 sec). Finally, when verbal stimulation yields no response, the observer looks for body movements or eye-opening following physical stimulation, like shaking the patient's shoulders or rubbing the patient's sternum. No reaction to physical stimulation implies an unarousable patient [36].
Riker designed the SAS in 1994 [56]. SAS is a seven-item scale with scores ranging from 1 (unarousable patient) to 7 (extremely agitated patient). As with the RASS, the observer first seeks agitation signs; if the patient is not awake, the observer applies verbal stimulation to look for the patient's arousal reaction and ability to execute simple commands. Finally, in case of no response, the observer uses light body shaking and, if necessary painful physical stimulation. The deepest sedation level corresponds to the patient's non-responsive to painful stimuli. To note, a very sedated patient may still have some spontaneous body movements [36].
Finally, for other sedation monitoring systems like the bispectral index (BIS), there is insufficient evidence for its value in monitoring sedation in critically ill and mechanically ventilated adults and its’ clinical outcomes or resource utilization. BIS effectiveness is uncertain due to the low- and very low-quality evidence derived from a limited number of studies [33].
For both pain and sedation assessment, our results show that the lack of scales available in the ICU is a significant nursing issue [13, 45, 46, 48, 49]. In addition, in the qualitative studies analyzed, common barriers to using assessment tools are the lack of education and knowledge and mistrust concerning their effectiveness [11, 13, 40, 45, 46, 48, 49, 51, 57]. Furthermore, altered vital signs are erroneously considered a pain presence indicator in patients unable to communicate. However, the literature denies such interpretation [1, 10, 11, 43, 44, 50].
This research suggests that active but relaxed patients facilitate collaboration with the nursing staff and improve patients' interaction with the environment, family members, and health professionals [11, 47, 51, 57].
4.4. Pharmacological Management
Our pharmacological pain and agitation management research yielded homogeneous results as guidelines define the recommended drug classes for ICU patients' analgesia and sedation [1, 8]. Primary pharmacological pain treatment includes intravenous opioid administration, while agitation treatment includes midazolam, propofol, and dexmedetomidine administration [1, 8, 34, 35]. Nonetheless, we could not find specific drug indications differentiated according to the ICU patient's clinical condition. In everyday practice, in the absence of established protocols, the pharmacological choice and drug combination are under the clinician's discretion and experience [1, 8, 34, 35, 58].
Individual opioid pharmacokinetics, pharmacodynamics properties, and expected side effects influence drug choice and dosages [1, 8]. The choice of opioids' continuous or intermittent boluses administration depends on the drug's pharmacokinetics and the frequency and severity of the patient's pain [8]. The use of non-opioid analgesics or pain-modulating drugs, such as local anesthetics (e.g., Bupivacaine), nonsteroidal anti-inflammatory drugs (e.g., ketolorac, ibuprofen), and anticonvulsants, may decrease total opioid administration, to stop opioids altogether, or to decrease their side effects [1, 8, 35, 36].
Opioid side effects may include cardiorespiratory depression, drowsiness, and potential psychological dependence. Thus, it is essential to use opioids’ lowest dose possible for the patient’s comfort [22] and simultaneously seek appropriate different and complementary analgesics [35, 36]. Ketamine can be used as an analgesic in hemodynamically unstable ICU patients [36]. Preventive analgesia and non-pharmacological pain-relieving interventions are recommended before invasive and potentially painful procedures in adult ICU patients [1, 8].
For safe treatment, ICU sedation drugs' pharmacological characteristics need to be known. Notably, benzodiazepines can cause respiratory depression and hypotension, especially when administered concomitantly with other cardiovascular depressant agents, such as opiates; moreover, in long-term administration, benzodiazepines can induce tolerance, with the consequent need for their dose to increase [1, 8, 29, 36].
Sedation with propofol implies hypnotic, anxiolytic, antiemetic, and anticonvulsant effects. With its rapid onset and offset, propofol is useful in patients requiring frequent awakenings for neurological assessments and facilitating daily sedation pause protocols [1, 8, 35].
Propofol may show several side effects [8]. Long-term administration can lead to peripheral tissue saturation and thus prolonged emergence. Dose-dependent effects may be respiratory depression and hypotension due to systemic vasodilation [8, 35]. Other side effects include hypertriglyceridemia, acute pancreatitis, and myoclonus. Finally, with an incidence of 1%, propofol administration may cause the propofol infusion syndrome (PRIS). The PRIS signs and symptoms vary but may include metabolic acidosis, hypertriglyceridemia, hypotension with increasing vasopressor requirements, and arrhythmias [59].
Dexmedetomidine has sedative, analgesic, and sympatholytic properties [1, 8, 34]. Dexmedetomidine sedation guarantees the patient’s ease of awakening and interaction with minimal respiratory depression [1, 8, 35, 58]. It produces a low incidence of delirium and accelerates its resolution [35]. With its limited effect on respiratory drive, dexmedetomidine is the drug of choice in non-intubated patients [8, 34]. The most commonly reported side effects are hypotension and bradycardia [1, 8, 35]. For these reasons, ICU sedation guidelines suggest using propofol or dexmedetomidine over benzodiazepines (midazolam or lorazepam) to improve clinical outcomes in mechanically ventilated adult patients [1, 8, 29, 34, 35, 37].
The 2018 sedation guideline indicates no essential differences in patient outcomes between using propofol or dexmedetomidine [1]. Nonetheless, benzodiazepines are essential for the ICU treatment of agitation, anxiety, and alcohol and benzodiazepine withdrawal [1, 8]. Patients at high risk of developing delirium should avoid benzodiazepines [37].
Mehta et al. showed that patients receive higher doses of opioids and benzodiazepines at night, and higher nighttime doses are associated with spontaneous breathing trial failure and delayed extubation [37].
4.5. Non-Pharmacological Management
Non-pharmacological options such as music intervention, imagery, aromatherapy, massage, and family presence may help reduce anxiety, thereby decreasing dependence on sedative and analgesic medications alone to manage distressful symptoms during mechanical ventilation [1, 8, 10, 34, 35, 37, 47, 60]. Particular attention should be paid to noise pollution reduction [1, 41].
Applying massage therapy addresses ICU patients' back, foot, and hand pain. The ICU Liberation Bundle recommends at least 20 minutes of light-pressure massage at least twice daily [10]. Cold therapy implies the application of ice packs onto appropriate body areas before invasive maneuvers [10]. Ice pack application for 10-20 minutes - until the skin temperature reaches about 15 degrees - helps pain perception reduction [13, 60].
Music therapy promotes pain perception reduction [10, 60]. The literature recommends using music for at least 20-30 minutes daily while carrying out daily practices. We have identified guided imagery, breathing exercises, and hypnosis practices among the interventions that can promote the patients' relaxation [10]. The most effective and used in collaborative patients are guided imagery and breathing exercises [10]. With the imagery-guided technique, the patient imagines being in a place of choice, thus stimulating positive images. This technique led to lower pain scores [10].
Sleep promotion is fundamental in preventing and reducing ICU patient agitation and stress. Non-pharmacological interventions, particularly those addressing the environmental context of noise pollution, should be addressed [1, 37]. Notably, some non-pharmacological interventions (e.g., massage therapy or music therapy) can be performed directly by the patient’s family members. Indeed, the literature shows that family members may play a fundamental role in managing analgosedation [10]. A 2019 review demonstrated that family members pay greater attention to their loved ones concerning pain assessment and the implementation of interventions to reduce pain and discomfort [61].
4.6. Analgosedation Perception by Nurses
Analgosedation evaluation and treatment by nursing personnel is influenced by a series of issues concerning lack of knowledge and consideration for the analgosedation, training, workplace organization, and communication barriers [11, 13, 43-52]. Improvement interventions should address understanding pain mechanisms and management, analgesia and sedation pharmacological features, assessment tools, and personal communication; further, attention should be paid to staff motivation, using specific guidelines and protocols, standardized methods of assessment, and correct prescription of analgosedation [11, 13, 39, 44, 47-49, 51, 52].
Sneyers et al. found that nurses consider using assessment scales as increasing professional autonomy, empowering their role, associated with benefits in patient outcomes, and helping to monitor sedation and cost control [43]. As for sedation, nurses believe that deep sedation impedes a patient's neurological assessment; nonetheless, an awake and agitated patient may be harmful to himself and the personnel [13, 40, 43, 45, 46, 50-52, 57]. Further, although sedation may be beneficial, it leads to complicated interactions with the patient. At the same time, it is easier to assist a sedated patient as an awake one requires more 'attention' [43, 50, 51, 57]. However, Laerkner et al. found no difference in self-assessed nurses’ workload between awake and sedated patients. There might be a potential economic saving with a 1:1 nurse-patient ratio and no sedation compared to a 1:2 nurse-patient ratio and sedation [41]. Several studies report that nurses' education on analgosedation assessment and management is poor, along with the lack of appropriate validated assessment tools for nurses [28].
Future research should focus on improving communication with mechanically ventilated patients to better manage sedation administration and pain control to patient needs, in addition to creating, validating, and employing reliable assessment measures for distressing symptoms such as pain and anxiety.
Finally, ensuring adequate sedation and analgesia for critically ill patients is an essential element for improving their clinical outcomes. Knowledge of signs for inadequate sedation and analgesia and the use of validated assessment tools and protocols for managing analgosedation would help healthcare professionals early recognize patients' discomfort and carry out targeted and timely interventions avoiding treatment delays. To promote the adoption of clinical guidelines, hospitals should focus efforts on improving the evidence-based knowledge of their nursing staff, provide adequate training by nurses with evidence-based practice experience, and offer ample support to allow nurses time to effectively implement guidelines. Nurses have a central role because they are in direct contact with patients. For this reason, specific nursing competence can improve the quality of care for critically ill patients and the quality of assistance focusing on the person.
4.7. Study limitations
This narrative review has some limitations that we wish to point out. The first limitation is that the research developed is not a foreground but a background one. As background review, we looked for general knowledge about analgosedation. Future foreground reviews should focus on specific analgosedation knowledge to inform clinical decisions or actions. Foreground reviews should overcome the issue of significant heterogeneity in the articles' typology and outcomes in the field of interest and that the populations considered comprise patients hospitalized in ICUs of different specialists. Secondly, the analysis of the studies was not conducted using validated tools but according to criteria pre-established by the researchers. A future systematic review may use such tools.
CONCLUSION
ICU analgosedation management (pain control first, and then sedation if necessary) is limited due to health professionals' knowledge gaps, inappropriate use of assessment tools, guidelines, and specific protocols. Recommended assessment tools are the BPS and CPOT for pain assessment and the RASS and SAS for sedation assessment. These tools, along with applying standardized protocols, based on specific guidelines, may reduce inadequate analgosedation adverse outcomes. The proper use of non-pharmacological methods may reduce pharmacological interventions for analgosedation management. Interventions to improve ICU analgosedation awareness and practice include training events, the use and consultation of literature guidelines, and the use of validated assessment tools. Such interventions may improve making informed clinical choices and implement effective and targeted assistance interventions.
ABCDEF BUNDLE
Assess, prevent and manage pain (A), both spontaneous awakening and spontaneous breathing trials (B), Choice of analgesia and sedation (C), assess, prevent and manage Delirium (D), Early mobility and exercise (E), and Family engagement (F).
LIST OF ABBREVIATIONS
| BIS | = Bispectral Index |
| BPS | = Behavioral Pain Scale |
| CPOT | = Critical Care Observational Tool |
| ICU | = Intensive Care Unit |
| NRS | = Numerical Rating Scale |
| PAD | = Pain, Agitation, and Delirium Guidelines |
| PRIS | = propofol infusion syndrome |
| RASS | = Richmond Agitation Sedation Scale |
| SAS | = Sedation Agitation Scale |
| VAS | = Visual Analog Scale |
AUTHOR'S CONTRIBUTIONS
All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted, and (4) agreement to be accountable for all aspects of the work.
ETHICAL STATEMENT
Ethical board approval for review studies is not required at our institutions for studies not involving human patient data collection. Nonetheless, the study project was endorsed and approved by the Critical Care Nursing Master Course Director (University of Bologna, Italy).
CONSENT OF PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this systematic review article are derived from published articles available at each article journal's public online database.
STANDARDS OF REPORTING
PRISMA guidelines were used.
FUNDING
None.
CONFLICT OF INTEREST
Boaz Samolsky Dekel is a member of the Editorial Advisory Board of The Open Anesthesia Journal.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the Critical Care Nursing Master Course Director (University of Bologna, Italy) who endorsed and approved the study project.
SUPPLEMENTARY MATERIALS
Supplementary material is available on the Publisher’s website.


