Mixed Reality versus Mass or Self-directed Training for Adolescents’ Basic Life Support Instruction: A Prospective, Randomized Pilot Study
Abstract
Background:
There is limited information about adolescents' Basic-Life-Support (BLS) training.
Objectives:
In this study, adolescents' BLS training proficiency and knowledge retention of the Mixed Reality (MR), Mass-Training (MT), and Self-Directed Learning (SDL) methods were prospectively compared, following the training-outcomes levels-model classification.
Methods:
First-year secondary-school students were randomized into the MR, MT, and SDL groups, and after baseline evaluation, at T0, they received congruent BLS theoretical and Cardiopulmonary-Resuscitation (CPR) training. Knowledge, skills retention, and trainees' training-activity self-evaluation were evaluated utilizing ten (knowledge) and five-items (self-evaluation) questionnaires, a BLS-sequence checklist, and chest compressions recording mannequin one and three months after T0. We used the Kruskal-Wallis test for median comparison.
Results:
At all times, the MR group knowledge answers' median (≥6/10) was significantly higher (p<0.05) than groups MT and SDL (≤6/10), with no significant differences between the latter. The MR CPR skills and BLS checklist acquisition and retention were significantly superior (p<0.05) to the other groups; the SDL group showed limited results. Hands position and chest recoil showed excellent outcomes in all groups and at all times. At all times, trainees positively evaluated the BLS-training importance. Pre-training low self-confidence in BLS practice improved over time, yet not significantly, in group MT. The trainees' majority (62%) preferred the MR method.
Conclusion:
In an adolescent cohort, MR methods' BLS/CPR knowledge and skills acquisition and retention were comparable, if not better, than the MT method and superior to the SDL one. Future multicenter randomized and controlled studies with larger sample sizes and more limited instructor-to-participant ratios are warranted to generalize findings.
1. INTRODUCTION
Early Basic Life Support (BLS) is the mainstay intervention for Out-of-Hospital Cardiac Arrest (OHCA). OHCA survival rates are higher when bystanders deliver prompt Cardiopulmonary Resuscitation (CPR) [1]. Although BLS training among laypeople has increased, only a minority of the OHCAs undergo bystander CPR.
Given its importance, BLS training should be extended to the entire population, including adolescents, by applying a suitable methodology. The latter should be adapted to the trainees’ socio-cultural features to promote interest, active participation, and the role of saving lives. Adolescents and adults may benefit from various training methods. The most shared method is classroom-based courses consisting of skill demonstrations, hands-on practice, and qualified trainer lectures [2]. Mass Training (MT), often used in schools, provides a lesson to multiple trainees, who simultaneously acquire practical skills under the instructor’s supervision.
Moreover, technological progress using electronic devices has enabled options like e-learning videos, mobile applications, gaming platforms, and Virtual Reality (VR). Among VR methods, Mixed Reality (MR), in particular, projects the trainee into the target scenario, allowing both virtual and physical first-hand experience [3-7]. Reality-simulation influence on learning outcomes is still debated; however, the importance of its positive stress and cognitive load in education has been proven; thus, it might be embedded into the training design [8]. Finally, Self-Directed Learning (SDL) showed no significant difference in learning outcomes when compared with instructor-led courses [9].
We sought to compare, within an adolescent cohort, the BLS training proficiency and knowledge acquisition and retention of the MT, MR, and SDL methods. We hypothesized no difference between the three methods.
2. MATERIALS AND METHODS
This prospective and randomized pilot study aims to compare, within a secondary-school-students cohort (aged 14 to 15 years), the BLS training outcomes of the MT, MR, and SDL methods. A comparison follows the training-outcomes levels-model classification [10, 11]. In particular, the assessed levels are: reaction to the learning experience (Level 1), modification of attitudes and perceptions (Level 2a), knowledge/skills acquisition (Level 2b), and retention over time (Level 2c). Compared outcomes are the BLS theoretical and practical skills retention over time (primary outcome), the trainees' self-evaluation of the BLS training activity, their confidence as BLS-trained people, and their preferred BLS-training method (secondary outcomes).
2.1. Population, Context, Inclusion and Exclusion Criteria
The target population was secondary-school students in Casalecchio di Reno (Italy). The study and BLS training took place during regular school hours. We planned a sample size of at least n=45 participants. Given the pilot study model of long-term multiple measurements design, we considered a dropout rate of 25%. Thus, we planned to recruit at least n=60 subjects.
The inclusion criteria were belonging to the first-year secondary school target class, not having previous theoretical/practical knowledge of BLS/CPR, and having informed consent to participate in the study signed by the parent or legal guardian of the student; the exclusion criterion was being ineligible for physical education.
2.2. Ethical Statement
The Medical and Surgical Sciences Department of Bologna's University (Italy) approved the study (Protocol # 3295–14/10/2019). Written informed consent was obtained from each parent or legal guardian of the participants. All information collected was anonymous. The study was conducted following Helsinki Declaration as revised in 2013.
2.3. Study Design
Fig. (1) depicts the flowchart of the study, including screening, recruitment, randomization, theoretical and practical training evaluation and interventions (T0), and follow-up evaluations at one (T1) and three (T2) months after T0. At T0, eligible participants were randomized into the three study groups (MT, MR, and SDL) with different BLS training interventions using a random number generator. At T0, we administered an anonymous Multiple-Choice Questionnaire (aMCQ) to establish the participants' socio-demographic characteristics and pre-course BLS theoretical knowledge. The participants' pre-course practical skills were evaluated using an advanced mannequin without prior BLS training. Hence, participants of the MT and MR groups received congruent theoretical training via a frontal lesson; participants of the SDL group received a regular BLS manual for independent self-appraisal. BLS theoretical training included the Survival Chain, BLS checklist, and CPR maneuvers for laypeople. Hence, MT and MR groups underwent a two-hour congruent BLS practice training. MT group members received a mannequin for individual practice under BLS-qualified instructor supervision. MR group members practiced using the MR technology under a BLS-qualified instructor and the Italian Resuscitation Council (IRC) staff assistance. SDL group had no hands-on practice training.
For the initial practice part, we used Prestant Ultralite® mannequins that allow chest compressions without performance recording. For the MR technology, we used the computer VR-CPR® software, HTC SteamVR Base Station, and HTC Vive Trackers audio headphones allowing the trainee to watch the Prestant Ultralite® mannequin as a natural person. The virtual scene area was a central square (Piazza Santo Stefano) in Bologna, Italy.
At T1 and T2, we administered once more the aMCQ, and participants individually performed a recorded BLS practice simulation; parallelly, an instructor filled out a six-item BLS-flow checklist. Finally, we also investigated the participants' opinions regarding the BLS training activity, their confidence as BLS-trained people, and their preferred BLS training method.
2.4. Measurement Tools
2.4.1. Questionnaires and BLS Checklist
We used three ad-hoc anonymous questionnaires and a checklist. In particular: a questionnaire for participants’ socio-demographic characteristics, a ten-item Multiple-Choice Questionnaire (aMCQ) for the BLS theoretical knowledge evaluation, a Likert-type five-item questionnaire inquiring about participants’ opinions regarding the BLS training activity, their confidence as BLS-trained people, and their preferred training method; and six-item checklist for the BLS sequence evaluation. For questionnaires and checklist details, see Supplementary Material appendixes I to III.
2.4.2. BLS Practice Evaluation
For BLS-practice evaluations, we used, at all times, the BT-Inc BLS Training Simulator: CPTA® (BT-CPTA). The latter detects the hands' position, frequency, depth, and chest recoil during chest compressions. BLS Practice performance outcomes were chest compressions rate (endpoint, 100-120/min), depth (endpoint, 50-60 mm), and percentage score of both correct hands position (endpoint, sternum lower third) and complete chest recoil, respectively. In the latter two outcomes, the score indicates the proportions of correct endpoints out of all compressions, respectively. At T1 and T2, for the BLS sequence evaluation, a six-item checklist was scored by the instructor.
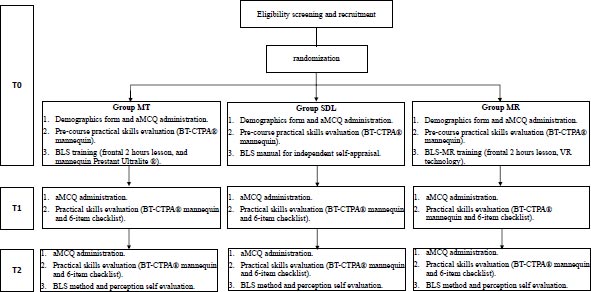
Footnotes: aMCQ, anonymous Multiple-Choice Questionnaire; MT, Mass Training; SDL, Self-directed learning; MR, Mixed Reality. For details on mannequins, see the main text.
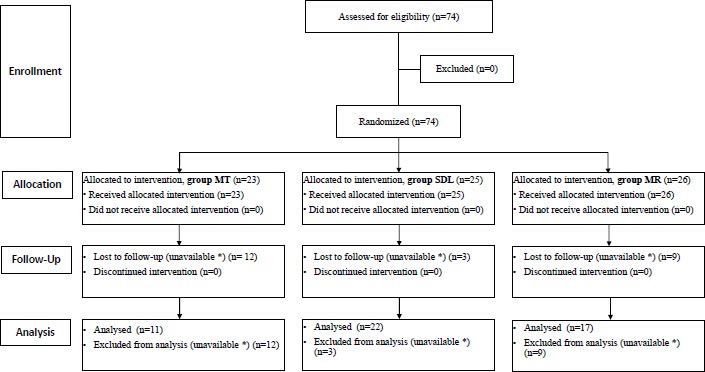
Footnotes: MT, Mass Training; SDL, Self-directed learning; MR, Mixed Reality. *, unavailable (school absence) at one of the study’s time points.
| Demographic Variables | All Groups N=50 |
MT Group n=11 |
MR Group n=17 |
SDL Group n=22 |
|---|---|---|---|---|
| Age (years) * | 14.5 (± 0.6) | 14.3 (± 0.5) | 14.4 (± 0.5) | 14.7 (± 0.6) |
| Gender (females) ** | 26 (52.0) | 7 (63.6) | 9 (52.9) | 10 (45.5) |
| Weight (> 50 kgs) ** | 44 (88.0) | 11 (100.0) | 14 (82.4.2) | 19 (86.4) |
*, Mean (±SD).
**, n (%).
| T |
All Groups* (n=50) |
MT* (n=11) |
MR* (n=17) |
SDL* (n=22) |
SDL vs MT p-value ** |
SDL vs MR p-value ** |
MT vs MR p-value ** |
| T0 | 4.5 (2.3; 1-9) | 4.0 (2.0; 1-7) | 6.5 (2.7; 3-7) | 4.0 (2.0; 1-9) | 0.443 | 0.009 | 0.013 |
| T1 | 5.5 (3.0; 1-9) | 5.0 (2.0; 1-7) | 7.0 (2.7; 4-9) | 5.0 (2.5; 1-7) | 0.614 | 0.013 | 0.023 |
| T2 | 6.0 (2.0; 1-9) | 6.0 (3.0; 1-8) | 7.0 (2.0; 4-9) | 6.0 (1.5; 2-7) | 0.132 | 0.002 | 0.217 |
T, Time point; MT, Mass Training; MR, Mixed Reality; SDL, Self-Directed Learning.
*, Median (IQR; range)
**, Pairwise comparison (Kruscal-Wallis test, p-value).
2.5. Data Presentation and Analysis
For statistical analyses, we used SPSS (Chicago) software version 28. Continuous, ordinal variables are reported as the median, interquartile range (IQR), and range; continuous variables are reported as absolute numbers and relative frequency. Data are reported both within the entire cohort and the study groups. We used the Kruskal-Wallis test to compare groups’ medians. Box and whiskers plots are used to represent the data and compared outcomes. Statistical significance was considered for p-value <0.05. We considered a positive outcome for the participants’ self-evaluation items if the proportions of negative answers (Not-at-all and Little) were ≤50% and vice-versa.
3. RESULTS
Fig. (2) is a Consort flow diagram of the study population. We excluded the participants who were unavailable (school absence) at one of the study’s time points from the final data analysis. The final study groups’ composition was: MT, n=11 (22.0%), MR, n=17 (34.0%), and SDL, n=22 (44.0%) participants.
Table 1 shows the participants' main Demographic Characteristics. Participants' mean age was 14.4 (± 0.5) years; n=26 (52%) were females, and n=6 (12%) weighed <50 kgs. Demographic variables showed no significant differences between the groups.
3.1. Theoretical Evaluation (aMCQ)
This section's results account for knowledge-outcome-classification levels 2b (knowledge acquisition) and 2c (knowledge retention over time). Table 2 reports the aMCQ's correct answers (out of ten) median, IQR, and range at the three study's time points for the entire cohort and each study group. It also reports the results of the pairwise comparison analyses (Kruskal-Wallis test) of the groups' correct-answers’ medians for each time point. At all times, the correct answers' median of group MR was ≥6, while that of groups MT and SDL was ≤6. The correct answers' median of the MR group was significantly higher than that of the SDL group at all times and the MT group at T0 and T1 (Table 2, p<0.05, respectively). Groups SDL and MT showed no significant differences in correct answers’ medians at all times. These results yield a comparable, if not better, BLS theoretical knowledge retention of MR training over MT and SDL methods.
Fig. (3) is a box and whiskers plot showing the median and IQR of the aMCQ's correct answers at the three study's time points for each study group. It also shows the comparison results of correct answers’ median between the study's time points for each group. In particular, the T0 to T2 median increase of correct answers was from 6.0 to 7.0 for group MR and 4.0 to 6.0 for groups MT and SDL. All groups showed significant correct answers' median improvement from T0 to T2; only group MR showed significant improvement from T0 to T1 (Fig. 3, p<0.05, respectively).
All groups showed improvement and retention of theoretical knowledge over time; however, improvement in the correct answers’ median was the greatest in the MR group and limited in the SDL group.
3.2. CPR Performance
This section's results account for skills’ outcome classification levels 2, b (acquisition) and c (retention over time). Table 3 reports the median, IQR, and range of the single CPR performance outcomes at the three study's time points in the study groups. It also reports the results of the pairwise comparison analysis (Kruskal-Wallis test) of the groups' CPR outcome medians at each time point.
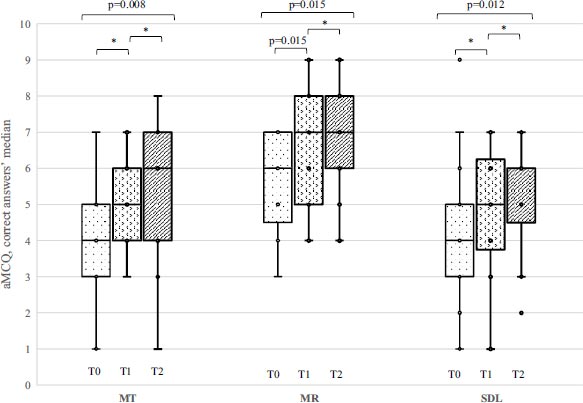
Footnotes: aMCQ, anonymous Multiple-Choice Questionnaire; MT, Mass Training; MR, Mixed Reality; SDL, Self-Directed Learning; T0, allocation pre-intervention; T1, one-month follow-up; T2, Three months follow-up *, Kruskal-Wallis test, p>0.05.
| CPR Variable | T |
All Groups Median (IQR; Range) |
MT Median (IQR; Range) |
MR Median (IQR; Range) |
SDL Median (IQR; Range) |
SDL vs MT * p-value |
SDL vs MR * p-value |
MT vs MR * p-value |
| Compression rate (n/min) | T0 | 104 (53; 50-218) | 96 (15; 71-218) | 128 (28; 94-156) | 82 (31; 50-162) | 0.373 | < 0.001 | 0.296 |
| T1 | 89 (50; 38-180) | 108 (18; 64 -123) | 97 (59; 38-155) | 78 (36; 44-180) | 0.009 | 0.306 | 0.296 | |
| T2 | 107 (33: 61-181) | 105 (16; 82-119) | 124 (21; 100-144) | 90 (28; 61-181) | < 0.001 | < 0.001 | 0.005 | |
| Compression Depth (mm) | T0 | 31 (14; 13-56) | 33(15; 13-41) | 34 (15; 21-50) | 31 (13; 13-56) | 0.264 | 0.394 | 0.296 |
| T1 | 39 (12; 14-66) | 41 (5; 24-66) | 43 (14; 30-64) | 33 (12; 14-52) | 0.004 | 0.005 | 0.296 | |
| T2 | 35 (13; 19 -62) | 37 (6; 23-62) | 44 (18; 26 -58) | 32 (10; 19-54) | 0.049 | < 0.001 | 0.003 | |
| Compression deviation (mm) | T0 | 19 (14; 37-0) | 17 (15; 37-9) | 16 (14; 29 – 0) | 21 (13: -37-0) | 0.264 | 0.394 | 0.296 |
| T1 | 11 (12; 39-6) | 9 (5; 26-6) | 8 (13; -20-4) | 17 (12; 39-0) | 0.004 | 0.005 | 0.296 | |
| T2 | 14 (13; 31-2) | 13 (6; 27-2) | 5 (13; 24-0) | 18 (8; 31-0) | 0.049 | < 0.001 | 0.003 | |
| Hands position (Sternum inferior third) | T0 | 100% (25%; 0-100%) | 100% (22%; 6-100%) | 100% (46%; 0-100%) | 100% (33%; 0.0-100%) | ** | ** | ** |
| T1 | 96% (27%; 0-100%) | 100% (2%; 35-100%) | 91% (43%; 0-100%) | 95% (27%; 6 -100%) | 0.063 | 0.350 | 0.034 | |
| T2 | 100% (13%; 10-100%) | 100% (15%; 66-100%) | 99% (24%; 10-100%) | 100% (33%; 0.0-100%) | ** | ** | ** | |
| Chest recoil | T0 | 100% (0.0%; 70-100%) | 100% (1%; 96-100%) | 100% (0%; 70-100%) | 100% (6%; 44-100%) | ** | ** | ** |
| T1 | 97% (27%; 0- 100%) | 97% (10%; 5-100%) | 100% (0%; 90-100%) | 100% (4%; 61-100%) | ** | 0.368 | 0.182 | |
| T2 | 100% (3%; 9-100%) | 100% (5%; 9-100%) | 100% (5%; 57-100%) | 100% (2%; 55-100%) | ** | ** | ** | |
| Check list (six items) |
T1 | 3 (2; 0 - 6) | 4 (2; 2 - 6) | 3 (1; 1 - 6) | 2 (1.9; 0 - 4.5) | 0.009 | 0.350 | 0.096 |
| T2 | 3 (3; 1 - 6) | 3 (2; 2 - 6) | 4 (2; 2 - 6) | 1 (0.5; 1 - 4.5) | < 0.001 | < 0.001 | 0.377 |
*, Pairwise comparison (Kruscal-Wallis test, p-value). **, no p value results because of similar medians.
3.2.1. Chest Compression Rate
Group MT showed median compressions rate congruent with the established endpoint (100-120/min) at T1 and T2, while group MR showed compression rates slightly above the endpoint at T0 and T2 and slightly under at T1. At all times, in the group SDL, the median compressions rate was under the expected endpoint. MR group median compression rate was significantly higher than group SDL at T0 and T2 and group MT at T2 (Table 3, p<0.01, respectively). At T1 and T2, the MT group median compression rate was significantly higher than group SDL (Table 3, p<0.01, respectively). No significant differences were shown, at T0, between compression rate medians of group MT and that of groups SDL and MR, respectively, and at T1, between group MR and groups SDL and MT, respectively.
3.2.2. Chest Compression Depth
At all times, no study group’s depth median reached the established depth endpoint (50-60 mm). Only the MR group showed a compression depth median of 44 mm at T2. MR group median compression depth was significantly greater than group SDL at T1 and SDL and MT at T2 (Table 3, p<0.01, respectively). At T1 and T2, the median compression depth of group MT was significantly greater than the SDL group (Table 3, p<0.01 and p<0.05, respectively). No significant differences were shown, at T0, between depth medians of all groups and at T1 between MR and MT groups.
3.2.3. Compressions’ Negative Deviation from the 50 mm Depth Target
At T0 median negative depth deviation in all groups was 19 mm, with no significant differences between the study groups. Group's MR median negative depth deviation further decreased at T1 and T2. MR group negative depth deviation median was significantly lower than group SDL at T1 and T2 and of group MT at T2 (Table 3, p<0.01, respectively).
3.2.4. Hands Position and Chest Recoil
All the study groups' median proportions of hands position and chest recoil variables reached, at all times, the established endpoints (Table 3, hands position at sternum lower third and chest recoil). In particular, at all times, correct hands position median proportions ranged from 91 to 100%, and those of valid chest recoil ranged from 97 to 100%. We found no significant differences between the study groups' hand position and chest recoil medians at all times.
3.2.5. Six-item BLS Checklist
SDL group checklist performance was poor at T1 and T2, showing a median of 2 and 1 correct items, respectively. MT group checklist median was significantly higher than that of the SDL group at T1 and T2; the performance of group MR was significantly higher than that of the SDL group at T2 (Table 3, p<0.01, respectively). In particular, group MR showed median improvement from 3 to 4, while group MT decreased from 4 to 3 correct items.
Finally, we analysed the BLS-sequence checklist and CPR performance in each group over time. Fig. (4) (panels A to D) shows, for each group, the checklist and three major CPR items (compression rate, depth, and depth deviation) median results and pairwise overtime comparison (Kruskal-Wallis test). From T1 to T2, checklist outcomes of groups MT and MR significantly improved, while those of SDL deteriorated (Fig. 4A, p<0.05, respectively).
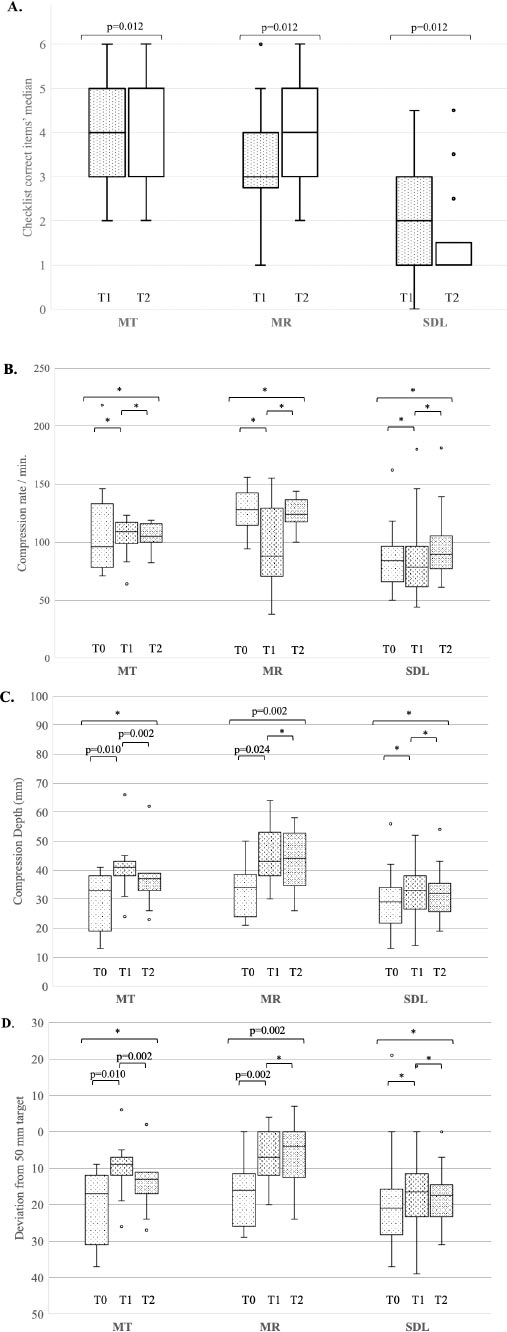
Footnotes: Panel A, BLS checklist correct items; Panel B, compression rate; Panel C, compression depth; Panel D, depth deviation. MT, Mass Training; MR, Mixed Reality; SDL, Self-Directed Learning. *, Kruskal-Wallis test, p>0.05.
| Participants’ Self-evaluation Item | T |
All Groups Median (IQR; Range) |
MT * Median (IQR; Range) |
MR * Median (IQR; Range) |
SDL * Median (IQR; Range) |
| 1. How much BLS training is useful and may serve you in the future? | T0 | 4 (1; 3-5) | 4 (1; 3-5) | 4 (2; 3-5) | 4 (1; 2-5) |
| T1 | 4 (2; 3-5) | 4 (2; 3-5) | 4 (2; 2-5) | 4 (1; 2-5) | |
| T2 | 4 (1; 3-5) | 4 (1; 2-5) | 4 (2; 2-5) | 3 (1; 2-5) | |
| 2. How much comfortable would you feel in helping by yourself a person needing BLS? | T0 | 2 (0; 1-4) | 2 (1; 1-3) | 2 (1; 1-4) | 2 (1; 1-4) |
| T1 | 3 (1; 1-5) | 3 (1; 2-5) | 3 (0; 2-4) | 3 (1; 1-4) | |
| T2 | 3 (1; 1-5) | 3 (1; 1-4) | 3 (1; 2-4) | 2 (1; 1-3) | |
| 3. Altogether, how much are you satisfied with the BLS training activity? | T0 | 3 (1; 2-5) | 3 (1; 3-5) | 4 (1; 3-5) | 3 (1; 2-5) |
| T1 | 3 (1; 1-5) | 3 (1; 3-5) | 4 (1; 3-5) | 3 (1; 1-5) | |
| 4. How satisfied you are with the BLS training you received? | T1 | 4 (1; 1-5) | 4 (1; 3-4) | 4 (2; 3-5) | 3 (1; 1-4) |
| 5. How would you evaluate your learning proficiency with the proposed teaching method? | T2 | 3 (1; 1-5) | 3 (2; 2-5) | 4 (1; 2-5) | 3 (1; 1-4) |
Answers score: N, Not at all = 1; L, Little = 2; S, Sufficient = 3; M, Much = 4; O, Overmuch = 5.
*, Pairwise comparison of SDL vs MT, SDL vs MR, and MT vs MR: Kruskal-Wallis test, p>0.05, respectively, at all times.
| Preferred Method |
All Groups n (%) |
Group MT n (%) |
Group MR n (%) |
Group SDL n (%) |
| MT | 12 (24.0) | 4 (36.4) | 4 (23.5) | 4 (18.2) |
| MR | 31 (62.0) | 3 (27.3) | 13 (76.5) | 15 (58.2) |
| SDL | 7 (14.0) | 4 (36.4) | 0 (0.0) | 3 (13.6) |
| Total | 50 (100.0) | 11 (100.0) | 17 (100.0) | 22 (100.0) |
Within each group, compression rate showed no significant changes over time (Fig. 4B). Group MT showed significant median changes, between T0 and T1 and between T1 and T2, for depth and depth deviation items; group MR showed significant improvements for the same CPR items between T0 and T1 and T2 (Fig. 4C and D, p<0.01, respectively).
3.3. Participants' Self-evaluation of BLS-training
This section's results account for outcomes of the classification of the learning experience (Level 1) and modification of attitudes and perceptions (Level 2a). Table 4 reports the participants' median answers (IQR and range) to the five-items self-evaluation questionnaire at the registered time points. Supplementary Material Appendix II, table B, reports the five items' answers' proportions in the study's groups.
For item 1, the median answer was 4.0 (Much), at all times, in the entire cohort and the study groups.; only at T2, the median of the SDL group was 3.0 (Sufficient). For item 2, the median answer at T0 was 2.0 (Little) in the entire cohort and the study groups, showing pre-training low self-confidence in BLS practice. At T1 and T2, this item median improved to 3.0 (Sufficient) in groups MT and MR but remained 2.0 (Little) in group SDL. For item 3 median answer was at all times 4.0 (Much) in group MR and 3.0 (Sufficient) in the entire cohort and groups MT and SDL. For item 4, the median answer was 4.0 (Much) in the entire cohort and groups MT and MR; and 3.0 (Sufficient) in group SDL. For item 5, the median answer was 3.0 (Sufficient) in the entire cohort and groups MT and SDL; the median was 4.0 in the MR group (Much).
At all times and for all items, there were no significant differences between the groups' medians (Table 3, p>0.05, respectively).
Participants' answers proportions for the self-evaluation items in the entire cohort and the study groups are reported in Supplementary Material Appendix II, Tables B and C, respectively. The proportions of negative answers (N+L) for all items and times were <50%, except for item 2 at T0. Notably, at T0, negative answers proportions in groups MT, MR, and SDL were 63.6, 74.9, and 86.4%, respectively, showing pre-training low confidence in BLS practice.
Finally, Table 5 reports the participants' preferred BLS training proportions. MR was the preferred method in the majority of the entire cohort (62%) and of groups MR (76.5%) and SDL (58.2%). Group MT showed a relatively low preference for the MR method (27.3%) and an equal preference (36.4%) for the MT and SDL methods.
4. DISCUSSION
In this prospective randomized pilot study, we compared the BLS training outcomes of the MT, MR, and SDL methods within a secondary-school-students cohort. The comparison followed the training-outcomes levels-model classification. [10, 11] We hypothesized no difference between the three methods.
Trainees within all the study groups broadly considered their Learning Experience as positive and satisfactory since, at all times, the portion of low satisfaction outcome (Not-at-all or little satisfied) of the BLS training activity was <50%. Notably, MR trainees showed higher satisfaction rates than MT and SDL trainees.
At all times, trainees positively evaluated the BLS-training importance. Pre-training low self-confidence in BLS practice in the entire cohort improved over time. Although not significantly, confidence improvement proportions were more enhanced in group MT. Notably, at T1, proportions of negative confidence in the group MR were the lowest; however, at T2, they increased to ≥50% in both MR and SDL groups. Thus, modification of attitudes and perceptions were shown in MT and, to a lesser extent, in MR and SDL groups.
All groups showed significant improvement and retention of BLS knowledge; however, improvement in the correct answers' median to the aMPQ was the greatest in the MR group and was limited in the SDL group. The MR group's CPR skills and BLS checklist acquisition and retention were generally significantly better than the other groups, whereas the SDL group was relatively poorer. Hands position and chest recoil showed excellent results in all groups and at all times.
BLS training using VR is increasing among professionals and nonprofessionals. VR methods, including semi-immersive, immersive virtual, and MR, support training by providing an immersive experience.7 These methods have been investigated regarding their goals, simulated procedures, and skills delivered. Nonetheless, the training outcomes’ comparison between MR-based and traditional BLS training methods is warranted since the literature on the potentialities of immersive methods for CPR training is limited [7, 12-14].
We used an MR application in collaboration with the IRC. MR is an immersive method that combines physical elements with a virtual environment; the trainee sees the virtual world and interacts with the real one. It provides tactile feedback and realistic interactions, enhancing the subjective impression of being part of a realistic experience [15], which further tempers training [16-18]. Our results show that the MR method’s outcomes of BLS knowledge and skills acquisition and retention are comparable, if not better than the MT method and superior to the SDL one.
We believe that VR methods, particularly the MR we used, have an essential role in nonprofessional BLS training, especially for younger people. The latter are more inclined to use electronic tools for apprehending new skills. Notably, MR was the preferred method in the majority of the entire cohort. Moreover, employing this preferred method among youngsters may indirectly raise BLS culture awareness among the general population.
Finally, despite the limited literature, a systematic review regarding BLS training methods for health science students found that the screened studies were of low methodological quality and had heterogeneous interventions and evaluations [19]. Moreover, no difference in the knowledge acquired was found between trainees receiving theoretical knowledge from an instructor and those who independently acquired knowledge through electronic support. Moreover, VR or MR methods were not included in this systematic review. To overcome these limitations, we conducted a prospective and randomized study, comparing the BLS training outcomes of the MT, MR, and SDL methods and using the well-established training outcomes’ level-model classification for the comparison evaluations.
The available participants and follow-up dropouts in this monocenter study partially limited its sample size. We preferred to include only participants present in all the study’s time points in the data analysis. In the literature, a maximum instructor-to-participant ratio of one to six for adults' CPR courses was recommended [20]. As the BLS training methods' effectiveness among adolescents is not yet defined, our groups' numerosity still permitted a randomized pilot assessment of the study's logistics and outcomes. Thus, it may enable further multicenter randomized and controlled studies with larger sample sizes and optimal instructor-to-participant ratios to generalize the study’s findings.
In our study, the SDL group had no hands-on practice training. This approach may raise the question of whether training was equivalent in all groups and thus comparable. In the literature, Self-Directed-Learning without hands-on practice is a known BLS training method. Therefore, as our goal was to compare different BLS training methods, we used the SDL method in its known format. In this study, compared to the MT and MR groups, the SDL group achieved limited proficiency in both theoretical and practical outcomes. Further studies may investigate whether the lack of hands-on practice is the cause of the shown poor SDL outcomes.
CONCLUSION
In a pilot study within a secondary-school-students cohort, we found that the MR methods' outcomes of BLS knowledge and skills acquisition and retention are comparable, if not better, than the MT method and superior to the SDL one. Future multicenter randomized and controlled studies with larger sample sizes and more limited instructor-to-participant ratios are warranted to generalize our findings.
LIST OF ABBREVIATIONS
| aMCQ | = Anonymous Multiple-choice Questionnaire |
| BLS | = Basic-life-support |
| BT | = CPTA, BT-Inc BLS Training Simulator |
| CPR | = Cardiopulmonary-resuscitation |
| IQR | = Interquartile Range |
| OHCA | = Out-of-hospital Cardiac Arrest |
| IRC | = Italian Resuscitation Council |
| MR | = Mixed Reality |
| MT | = Mass-training |
| SDL | = Self-directed learning |
| VR | = Virtual reality |
AUTHOR'S CONTRIBUTIONS
All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted, and (4) agreement to be accountable for all aspects of the work.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Medical and Surgical Sciences Department of Bologna's University (Italy) approved the study (Protocol # 3295–14/10/2019).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT OF PUBLICATION
Written informed consent was obtained from each parent or legal guardian of the participants.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
CONFLICT OF INTEREST
Boaz Samolsky Dekel is the member of the Editorial Advisory Board of the journal The Open Anesthesiology Journal.
ACKNOWLEDGEMENTS
The Italian Resuscitation Council (IRC) endorsed the study and supplied the study's technical instrumentations unconditionally.
SUPPLEMENTARY MATERIALS
Supplementary material is available on the Publisher’s website.


